Podcast
Questions and Answers
What is the primary function of the cilia on ciliated columnar cells?
What is the primary function of the cilia on ciliated columnar cells?
How many cilia are typically found on the apical surface of a ciliated columnar cell?
How many cilia are typically found on the apical surface of a ciliated columnar cell?
What structure is primarily affected by the asymmetry of the heart?
What structure is primarily affected by the asymmetry of the heart?
How many lobes does the right lung have?
How many lobes does the right lung have?
Signup and view all the answers
Which of the following statements is true regarding goblet cells?
Which of the following statements is true regarding goblet cells?
Signup and view all the answers
What can be inferred about regions lacking cilia?
What can be inferred about regions lacking cilia?
Signup and view all the answers
What term describes the tubes that branch from the trachea to each lung?
What term describes the tubes that branch from the trachea to each lung?
Signup and view all the answers
Which cell type is described as the most abundant among those mentioned?
Which cell type is described as the most abundant among those mentioned?
Signup and view all the answers
Which of the following statements is true regarding the structure of the left lung?
Which of the following statements is true regarding the structure of the left lung?
Signup and view all the answers
What impact does the heart's position have on the left lung?
What impact does the heart's position have on the left lung?
Signup and view all the answers
What type of epithelium makes up the mucosa?
What type of epithelium makes up the mucosa?
Signup and view all the answers
What happens to cartilage as one moves distally in the bronchi?
What happens to cartilage as one moves distally in the bronchi?
Signup and view all the answers
What are the primary functions of the cilia and mucus in the mucosa?
What are the primary functions of the cilia and mucus in the mucosa?
Signup and view all the answers
What type of cells are included in the mucosa along with the epithelium?
What type of cells are included in the mucosa along with the epithelium?
Signup and view all the answers
What type of muscle predominates in the bronchi as you move distally?
What type of muscle predominates in the bronchi as you move distally?
Signup and view all the answers
Which of the following layers supports the mucosa?
Which of the following layers supports the mucosa?
Signup and view all the answers
What is the primary function of adventitia in the bronchi?
What is the primary function of adventitia in the bronchi?
Signup and view all the answers
Which characteristic is NOT associated with cilia found in the mucosa?
Which characteristic is NOT associated with cilia found in the mucosa?
Signup and view all the answers
What is NOT present in the most distal parts of the bronchi?
What is NOT present in the most distal parts of the bronchi?
Signup and view all the answers
What characterizes the bronchi at their most distal sections?
What characterizes the bronchi at their most distal sections?
Signup and view all the answers
What type of epithelium is found in the larger bronchioles?
What type of epithelium is found in the larger bronchioles?
Signup and view all the answers
How does the epithelium change from the larger bronchioles to the smallest terminal bronchioles?
How does the epithelium change from the larger bronchioles to the smallest terminal bronchioles?
Signup and view all the answers
What type of epithelium replaces the ciliated pseudostratified columnar in the smallest terminal bronchioles?
What type of epithelium replaces the ciliated pseudostratified columnar in the smallest terminal bronchioles?
Signup and view all the answers
Which feature characterizes the epithelium in the smallest terminal bronchioles?
Which feature characterizes the epithelium in the smallest terminal bronchioles?
Signup and view all the answers
What describes the arrangement of epithelial cells in the larger bronchioles?
What describes the arrangement of epithelial cells in the larger bronchioles?
Signup and view all the answers
What is the role of Type II cells in the alveoli?
What is the role of Type II cells in the alveoli?
Signup and view all the answers
What is the primary function of alveolar macrophages?
What is the primary function of alveolar macrophages?
Signup and view all the answers
Which statement is false regarding the differentiation of Type II cells?
Which statement is false regarding the differentiation of Type II cells?
Signup and view all the answers
Which of the following best describes macrophages in the lungs?
Which of the following best describes macrophages in the lungs?
Signup and view all the answers
What event can trigger Type II cells to differentiate into Type I cells?
What event can trigger Type II cells to differentiate into Type I cells?
Signup and view all the answers
Study Notes
Histology Study Notes
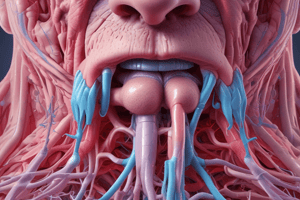
- The document details the respiratory system, including its structure and function.
- Two main categories are presented: structural and functional.
- Structurally, the respiratory system is divided into the upper respiratory system (nose, nasal cavity, pharynx, etc.) and the lower respiratory system (larynx, trachea, bronchi, lungs).
- Functionally, the respiratory system is categorized into the conducting zone (tubes and cavities filtering, warming, and moistening air) and the respiratory zone (sites of gas exchange within the lungs, involving respiratory bronchioles, alveolar ducts, and alveoli).
- Respiratory epithelium is pseudostratified columnar cells containing goblet cells.
- Cell types within the respiratory epithelium include ciliated columnar cells, goblet cells, brush cells, small granule cells (Kulchitsky cells), and basal cells.
- Specialized organ at the entrance to the respiratory system.
- Comprised of an external nose and an internal nasal cavity.
- The external nose has supporting bone and hyaline cartilage.
- The cartilaginous framework connects with the skull bones.
- The nasal cavity is lined with a mucous membrane.
- Air is filtered, warmed, and humidified in the nasal cavity.
- The nasal cavity contains the vestibule, which leads initially to areas with keratinized tissue, transitioning to pseudostratified columnar epithelium.
- Coarse hairs filter large particles, and sebaceous and sweat glands are present.
- Nasal septum: partitions the cavity into left and right halves.
Respiratory Cells
- Ciliated columnar cells (most abundant) have cilia propelling mucus toward the nose.
- Goblet cells are numerous and produce mucus.
- Brush cells are fewer, columnar with microvilli, connected to afferent nerves.
- Small granule (Kulchitsky) cells are part of the diffuse neuroendocrine system, rare in the structures.
- Basal cells are stem cells, creating more differentiated epithelial cells.
Components of the Respiratory System
- The nose contains a framework of bone and hyaline cartilage.
- The nose and nasal cavity have important components like the septum and conchae.
- The nasal cavity is protected by specialized tissues such as olfactory epithelium and seromucous glands.
- The structure of the respiratory tract includes ducts, which are important to the pressure normalization and tear drainage.
Pharynx
- Extends from the internal nares to the larynx and is divided into three regions.
- Nasopharynx.
- Oropharynx.
- Laryngopharynx.
- The nasopharynx is lined with respiratory epithelium.
- The oropharynx and laryngopharynx are lined with nonkeratinized stratified squamous epithelium.
Larynx
- Connects the pharynx to the trachea.
- Formed from nine cartilages (hyaline and elastic).
- The larynx's elastic and hyaline cartilage allow flexibility, while the thyroid cartilage is prominent.
- Contains vocal cords (in the larynx) important for voice production.
Trachea
- A tubular passage, 12cm long and 2.5cm in diameter.
- Lies anterior to the esophagus.
- Composed of 16-20 C-shaped hyaline cartilage rings.
Layers of tracheal wall
- Mucosa: epithelium (ciliated pseudostratified columnar with goblet cells) and lamina propria.
- Submucosa: areolar connective tissue with seromucous glands.
- Hyaline cartilage: C-shaped rings connected by dense connective tissue and fibromuscular membrane.
- Adventitia: areolar connective tissue connecting the trachea to surrounding structures.
Division of Bronchi
- The trachea branches into two primary bronchi, one for each lung.
- Each primary bronchus branches into lobar bronchi, then into segmental bronchi, continuing to terminal bronchioles.
- In smaller branches, cartilage decreases and smooth muscle increases.
Alveolar Walls
- Thin walls allow for gas exchange.
- Consist of a single layer of epithelial cells (Type I and Type II alveolar cells).
- The capillaries surround the alveoli for gas exchange.
- Alveolar macrophages are important for cleaning the alveoli.
Respiratory Membrane
- The respiratory membrane consists of alveolar epithelium, basement membrane, capillary basement membrane and capillary endothelium.
- This membrane facilitates gas exchange.
Bronchioles
- Smallest airways.
- Do not contain cartilage in their walls.
- Epithelium changes from pseudostratified to simple.
- Contain smooth muscle for adjusting airflow.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the anatomy and functions of the respiratory system with this quiz. Topics include ciliated columnar cells, lung structure, and mucosal functions. Perfect for students studying biology or related health sciences.