354 Questions
What is the primary function of the iris?
To regulate the amount of light entering the eye
What is the approximate diameter of the iris?
12 mm
What is the thickest part of the iris?
Iris collarette
What is the function of the dilator muscle?
To dilate the pupil
What is the term for the junction between the iris and the ciliary body?
Iris root
What is the approximate thickness of the iris at the iris root?
200 µm
What happens to the pupil in low lighting conditions?
It dilates
What are the two zones of the iris?
Peripheral ciliary zone and central pupillary zone
What is the function of the sphincter muscle?
To constrict the pupil
What is the anatomical location of the iris?
Most anterior component of the uvea
What is the primary function of the iris?
To control the amount of light entering the eye
What is the histological layer of the iris that contains melanocytes?
Anterior border layer
What is the name of the structure formed by the radial folds of the epithelium at the pupil margin?
Pupillary ruff
What is the function of the iris dilator muscle?
To dilate the pupil
What is the name of the muscle that constricts the pupil?
Iris sphincter
What is the purpose of the pupillary ruff?
To facilitate social signaling
What is the name of the layer of the iris that contains loose collagenous matrix with fibroblasts and melanocytes?
Stroma
What is the name of the cells that have engulfed melanosomes in the stroma?
Clump cells
What is the name of the structure formed by the apical processes of the anterior epithelial cells?
Apical process
What is the function of the posterior epithelium of the iris?
To attach to the apical process of the anterior epithelium
What is the characteristic feature of the anterior iris surface?
Thin, radial trabeculae
What is the function of the melanocytes in the posterior iris surface?
To prevent light from entering the eye
What is the inheritance pattern of iris pigmentation?
Polygenic inheritance
What is the characteristic feature of the iris vasculature?
Non-fenestrated vessels with tight junctions
What is the purpose of the radial vessels in the iris stroma?
To supply the iris
What is the pattern of the radial vessels in the iris stroma?
Spiral pattern
What is the result of the pupillary light reflex?
Constriction of the pupil
What is the pathway of the pupillary light reflex?
Retina -> optic nerve -> brainstem -> pupillary muscles
What is the function of the two smooth muscles in the iris?
To govern pupil size
What is the significance of the iris structure?
It relates to function, specifically pupil size and light entry
What is the purpose of the fluid layers in the globe?
To maintain structure and function
What is the approximate size of the cornea?
12 mm horizontally and 11 mm vertically
What is the function of the conjunctiva?
To produce mucus and protect the eye
What is the purpose of the limbus?
To connect the cornea to the sclera
What is the approximate width of the limbus?
1.75 mm
What is the name of the layer between the epithelium and stroma in the cornea?
Bowman's layer
What is the purpose of the scleral sulcus?
To form the boundary between the cornea and sclera
What is the name of the layer between the stroma and endothelium in the cornea?
Descemet's membrane
What is the total surface area of the conjunctiva?
16 mm²
How is the conjunctiva attached to the limbus?
Loosely attached
What is the primary function of Tenon's capsule?
To support and protect the globe
Which of the following structures is NOT part of the anterior chamber?
Ciliary body
What is the main component of the sclera?
Type I collagen
What is the purpose of the Superficial plexus in the episclera?
To provide nutrients to the sclera
What is the characteristic feature of the lamina fusca?
It is rich in elastic fibres
What is the function of the trabecular meshwork in the anterior chamber angle?
To drain aqueous humour
What is the primary function of the posterior chamber?
To store aqueous humour produced by the ciliary processes
What is the purpose of the stroma in the iris?
To contain the sphincter and dilator muscles
What is the characteristic feature of the scleral stroma?
It has interlacing collagen fibres of varying diameter and orientation
What is the primary function of the episclera?
To provide nutrients to the sclera
What is the primary function of the epithelium in the ciliary body?
To produce aqueous humour
What is the orientation of the smooth muscles in the ciliary muscle?
Longitudinally, radially, and circularly
What is the composition of vitreous humour?
98% water, 2% collagen and hyaluronic acid
What is the thickness of the light sensing film of the eye?
0.5 mm
What is the purpose of hyaluronic acid in the vitreous humour?
To stabilize the vitreous and maintain transparency
What is the vascular supply of the inner retina?
Central retinal vessels
What is the structure that supplies the outer retina?
Choroid
What is the function of the ciliary muscle?
To control the contraction of the zonular fibres
What is the structure that forms the lens fibres?
Lens epithelium
What is the characteristic of the lens fibres?
They start at the equator and migrate towards the poles
What are the two zones of the ciliary body?
pars plicata (anterior) and pars plana (posterior)
What is the function of the ciliary muscle?
to loosen zonular fibres, increasing lens convexity for accommodation
What are the three main structures of the lens?
capsule, cortex, and nucleus
What is the function of the vitreous humour?
to maintain transparency and stability of the vitreous chamber
How is the retina subdivided based on vascular supply?
into inner retina (supplied by central retinal vessels) and outer retina (supplied by choroid)
What is the function of the choroid?
to supply the outer retina
What is the percentage of water in the vitreous humour?
~98%
What is the purpose of the lens epithelium?
to produce lens fibres
What is the significance of the posterior chamber?
it is where the lens is located
What is the function of the hyaluronic acid in the vitreous humour?
to stabilise the vitreous and maintain transparency
What is the primary function of the Orbicularis oculi muscle?
To close the eyelid and facilitate tear drainage
Which muscle is responsible for voluntary closure of the eyelid?
Orbital orbicularis
What is the term for the opening between the eyelids?
Palpebra fissure
Which muscle has vertically orientated muscle fibres?
Frontalis
What is the name of the fascial sheath that surrounds the globe and optic nerve?
Capsule of Tenon
What is the function of the Muscle of Muller?
To maintain upper eyelid elevation
What is the term for the folds of skin and tissue that cover the globe?
Eyelids
Which muscle moves the brow medially, towards the nose?
Corrugator
What is the purpose of the tears in the eye?
All of the above
What is the term for the dense connective tissue that surrounds the bony orbit?
Periorbita
What is the main function of the meibomian glands in the eyelid?
Producing the lipid layer of the tear film
Which of the following glands is responsible for immune defense in the eyelid?
Glands of Moll and Zeis
What is the function of the mucin layer in the tear film?
Binding the tear film to the ocular surface
What is the pathway of tear drainage?
Puncta -> canaliculi -> nasolacrimal duct -> nasolacrimal sac
What is the approximate thickness of the tear film?
7-10 µm
What is the function of the Glands of Moll and Zeis?
Immune defense and unknown functions
What is the location of the accessory lacrimal glands?
Conjunctival fornix
What is the function of the conjunctiva?
A thin transparent layer over the eyeball and lids
What is the purpose of the tarsal plate in the eyelid?
Providing rigidity and shape to the eyelid
What is the characteristic of the tear film layers?
A blended phase, not three distinct layers
What is the primary characteristic of striated muscle histology?
Presence of cross-striations
What is the function of the epimysium in striated muscle?
To envelop the entire muscle
What is the characteristic feature of smooth muscle?
Specialised for continuous contraction of relatively low force
What is the purpose of gap junctions in smooth muscle cells?
To allow electrical excitation to pass between cells
What is the approximate length of smooth muscle cells?
12-200 µm
What is the characteristic feature of cardiac muscle?
Specialised for continuous, rhythmic contraction
What is the function of the perimysium in striated muscle?
To separate groups of muscle fibres into fascicles
What is the characteristic feature of skeletal muscle?
Presence of cross-striations
What is the function of the endomysium in striated muscle?
To envelop individual muscle fibres
What is the characteristic feature of myofibrils in striated muscle?
Longitudinally aligned, composed of repeating sarcomeres
What is the characteristic feature of the extracellular matrix in extraocular muscles?
Dense plaques attaching cells to the surrounding extracellular matrix
What is the function of the annulus of Zinn?
Origin of the 4 rectus muscles and medial rectus
What is the characteristic feature of the orbital layer in extraocular muscles?
Fewer muscle fibres and denser blood supply
What is the path of the superior oblique muscle?
Originate from lesser wing of sphenoid, course anteriorly, and pass through trochlea
What is the characteristic feature of the global layer in extraocular muscles?
Large myofibrils and slow tonic contraction
What is the characteristic feature of the tendon of the superior oblique muscle?
Longest tendon of all EOMs, starting ~1mm posterior to the trochlea
What is the characteristic feature of the inferior oblique muscle?
Inserts anterior to the equator, but inferolaterally
What is the characteristic feature of the spiral of Tillaux?
Imaginary spiral formed by the insertion of the rectus muscles
What is the characteristic feature of the rectus muscles?
Insert different distances from the limbus
What is the characteristic feature of the tendon of the extraocular muscles?
Collagen fibres enter superficial layers of the sclera
Which of the following muscles is responsible for abduction?
Lateral rectus
Which artery supplies the superior rectus and lateral rectus muscles?
Superior branch of the ophthalmic artery
What is the primary action of the superior oblique muscle?
Intorsion
Which muscle originates at the orbital apex with the rectus muscles?
Levator muscle
What is the function of Müller's muscle?
Increases the width of the palpebral aperture in fear or excitement
What is the name of the protein marker used to identify axons in Müller's muscle?
Peripherin
What is the primary function of the 6 extraocular muscles (EOMs)?
Moving the eyeball
What is the approach used by optometrists to identify the cause of an EOM dysfunction?
Isolating the affected EOM and working backwards to find the cause
What is the name of the muscle that is responsible for elevation and intorsion of the eyeball?
Superior rectus
What is the characteristic feature of striated muscle that allows for forceful contractions of short duration?
The arrangement of contractile proteins giving the histological appearance of prominent cross-striations
What is the primary function of cardiac muscle, and how does it differ from striated and smooth muscle?
Cardiac muscle provides continuous, rhythmic contraction of the heart, and its structural and functional characteristics are intermediate between striated and smooth muscle
What is the purpose of the perimysium in striated muscle, and how does it relate to the epimysium?
The perimysium is a connective tissue sheath that separates groups of muscle fibers into fascicles, and it is continuous with the epimysium
What is the primary difference between the structure and function of smooth muscle cells compared to striated muscle fibers?
Smooth muscle cells lack regular sarcomeres, and their contractile proteins are not organized into repeating units, resulting in a smooth, unstriated appearance
What is the function of gap junctions in smooth muscle cells, and how does it enable coordinated contraction?
Gap junctions allow electrical excitation to pass between smooth muscle cells, enabling coordinated waves of contraction
What is the significance of the endomysium in striated muscle, and how does it relate to the structure of muscle fibers?
The endomysium is a connective tissue sheath that surrounds individual muscle fibers, and it is composed of longitudinally aligned myofibrils made up of repeating sarcomeres
What is the difference between the dense plaques in tendons and the dense plaques in extraocular muscles?
In tendons, dense plaques attach cells to the surrounding extracellular matrix, whereas in extraocular muscles, dense plaques are involved in cell-cell attachment via desmosomes.
What are the two distinct regions of extraocular muscles, and how do they differ?
The two distinct regions of extraocular muscles are the outer orbital layer and the inner global layer. The outer orbital layer is adjacent to the periorbital and orbital bones, whereas the inner global layer is adjacent to the optic nerve and the eye.
What are the characteristic features of the fibre types in the orbital and global layers of extraocular muscles?
The orbital layer has fibres with high numbers of mitochondria, small myofibrils, and fast twitch, fatigue-resistant contraction. The global layer has red fibres with high myoglobulin, slow twitch, and fatigue-resistant contraction, and white fibres with less myoglobulin, fast twitch, and potentially fatiguable contraction.
What is the significance of the annulus of Zinn, and how does it relate to the extraocular muscles?
The annulus of Zinn is a dense, fibrous connective tissue ring located at the orbit apex, which serves as the origin for the four rectus muscles and also attaches to the dural sheath of the optic nerve.
What is the unique feature of the superior oblique muscle, and how does it differ from the inferior oblique muscle?
The superior oblique muscle has a long tendon that starts ~1mm posterior to the trochlea, whereas the inferior oblique muscle inserts posterior to the equator, but inferolaterally.
What is the pattern of insertion of the four rectus muscles, and how does it relate to the spiral of Tillaux?
The four rectus muscles insert at different distances from the limbus, with the medial rectus inserting closest to the limbus and the superior rectus inserting farthest. This pattern is described by the imaginary spiral of Tillaux.
What nerve is responsible for innervating the superior oblique muscle?
CN IV (Trochlear Nerve)
Which artery branch supplies the superior rectus and lateral rectus muscles?
Superior (lateral) branch of ophthalmic artery
What is the primary action of the inferior oblique muscle?
Exyclotorsion
What is the function of Müller's muscle?
Raising the upper lid
What is the significance of the 6 EOMs working in unison?
Coordinating eye movements
What is the primary action of the superior rectus muscle?
Elevation
Which muscle is responsible for adduction of the eye?
Medial rectus
What is the significance of the inferior branch of the ophthalmic artery?
Supplies the inferior rectus, medial rectus, and inferior oblique muscles
What is the main difference between the autonomic nervous system and the somatic nervous system?
The autonomic nervous system is involuntary, responsible for controlling smooth muscle, cardiac muscle, and glands, whereas the somatic nervous system is voluntary, responsible for controlling skeletal muscle.
What is the function of the enteric nervous system?
The enteric nervous system is responsible for controlling the gastrointestinal tract, often referred to as the 'little brain' of the gut.
What is the difference between afferent and efferent nerves in the somatic nervous system?
Afferent nerves are sensory nerves that transmit information from the periphery to the central nervous system, whereas efferent nerves are motor nerves that transmit information from the central nervous system to the periphery.
What is the function of the sympathetic nervous system?
The sympathetic nervous system is responsible for the 'fight-or-flight' response, mobilizing energy stores for increased activity.
What is the function of the cranial nerves?
The cranial nerves transmit sensory information from the head and neck to the brain and control the actions of the head and neck.
Through which structure does the nasociliary nerve pass?
Superior orbital fissure inside common tendinous ring.
What is the function of the lacrimal nerve?
Stimulates the lacrimal gland.
What is the destination of the supraorbital nerve?
Skin and conjunctiva of upper lid, and forehead.
What is the origin of the infratrochlear nerve?
Nasociliary nerve.
What is the function of the maxillary division of the trigeminal nerve?
Sensory for skin and conjunctiva of lower lid, cheek, and upper lip.
What is the function of the oculomotor nerve (CN III)?
Movement of eye, elevation of upper lid, pupillary constriction, and accommodation
Which cranial nerve is responsible for transmitting visual information from the retina to the brain?
Optic nerve (CN II)
What are the three branches of the trigeminal nerve (CN V)?
Ophthalmic, maxillary, and mandibular
What is the function of the trochlear nerve (CN IV)?
Movement of the superior oblique muscle
What is the origin of the olfactory nerve (CN I)?
Olfactory receptor cells in the nasal cavity
What is the main function of the abducens nucleus, and which muscle is innervated by it?
The main function of the abducens nucleus is to control lateral eye movement, and it innervates the lateral rectus muscle.
What is the difference between the sympathetic and parasympathetic nervous systems, and how do they relate to the autonomic nervous system?
The sympathetic nervous system is responsible for 'fight or flight' responses, while the parasympathetic nervous system is responsible for promoting rest and relaxation. The autonomic nervous system is a branch of the nervous system that controls involuntary actions, and it is divided into the sympathetic and parasympathetic nervous systems.
What is the function of the oculocardiac reflex, and which nerves are involved in this reflex?
The oculocardiac reflex is a reflex that decreases heart rate in response to pressure or traction on the extraocular muscles, and it involves the trigeminal and vagus nerves.
What is the main function of the vagus nerve, and which structures are innervated by it?
The main function of the vagus nerve is to control various involuntary functions, such as heart rate, digestion, and respiration, and it innervates structures such as the pharynx, larynx, trachea, esophagus, and thoracic and abdominal viscera.
What is the main function of the hypoglossal nerve, and which muscles are innervated by it?
The main function of the hypoglossal nerve is to control tongue movement, and it innervates the intrinsic and extrinsic muscles of the tongue.
Which branch of the ophthalmic nerve communicates with the infratrochlear branch of the nasociliary nerve?
Supratrochlear nerve
What is the primary function of the zygomatic nerve?
Stimulating the lacrimal gland
Which nerve enters the superior orbital fissure inside the common tendinous ring?
Ophthalmic – Nasociliary nerve
Which nerve is responsible for the sensory function of the skin and conjunctiva of the lower lid, cheek, and upper lip?
CN V – Maxillary division
What is the origin of the anterior ethmoidal nerve?
Ophthalmic – Nasociliary nerve
Which cranial nerve is responsible for sensation from the oropharynx, middle ear, carotid body, and carotid sinus?
CN IX - Glossopharyngeal nerve
Which of the following nerves is NOT directly involved in the sensation or control of the eye?
CN X - Vagus nerve
Which nerve is responsible for the parasympathetic control of the lacrimal gland and mucous membranes of the nasal and oral cavities?
CN VII - Facial nerve
Which cranial nerve is responsible for transmitting sensory information from the forehead, scalp, eyelids, nose, and eye?
Trigeminal nerve (CN V)
Which cranial nerve is responsible for the sensation of equilibrium and motion?
CN VIII - Vestibulocochlear nerve
Which cranial nerve is responsible for pupillary constriction and accommodation?
Oculomotor nerve (CN III)
Which nerve is responsible for the motor control of the intrinsic and extrinsic muscles of the tongue?
CN XII - Hypoglossal nerve
Which cranial nerve has a central connection to the lateral geniculate nucleus of the thalamus and the pretectal area of the midbrain?
Optic nerve (CN II)
Which cranial nerve has a superior division that innervates the superior rectus and levator palpebrae superioris muscles?
Oculomotor nerve (CN III)
Which cranial nerve has a central connection to the trigeminal ganglion and is responsible for transmitting sensory information from the anterior 2/3 of the tongue?
Trigeminal nerve (CN V)
What is the main function of the autonomic nervous system?
Control of involuntary actions, such as heart rate and digestion
What is the primary function of the somatic nervous system?
Regulation of voluntary movements, such as muscle contraction
What is the primary function of the 12 cranial nerves?
Transmission of sensory information from the head and neck
What is the main function of the central nervous system?
Processing and interpretation of sensory information
What is the main function of the peripheral nervous system?
Sending and receiving information between the CNS and the rest of the body
What is the terminal branch of the lacrimal artery that supplies the lacrimal sac and nose?
Sal nasal artery
What is the pathway by which the aqueous humour drains?
Conjunctival/Episcleral return, draining to the anterior ciliary veins, and then to the ophthalmic veins
What is the function of the vortex veins?
Drains the choroid
What is the normal range of vortex veins in an eye?
4 to 8
What is the pathway by which the retinal drainage occurs?
Central retinal vein → ophthalmic vein → cavernous sinus
What is the pathway by which the conjunctival/episcleral drainage occurs?
Anterior ciliary veins → ophthalmic veins → cavernous sinus
What is the pathway by which the uveal drainage occurs?
Vortex veins → superior ophthalmic vein → cavernous sinus or vortex veins → inferior ophthalmic vein → pterygoid plexus
What is the exit point of the superior ophthalmic vein?
Superior orbital fissure
What is the exit point of the inferior ophthalmic vein?
Inferior orbital fissure
What is the pathway by which the uveal drainage occurs in the superior ophthalmic vein?
Vortex veins → superior ophthalmic vein → cavernous sinus
What is the path of blood flow from the right atrium to the left eye?
Right atrium → right ventricle → pulmonary artery → lung → pulmonary vein → left atrium → left ventricle → aorta → internal carotid artery → ophthalmic artery → left eye
What is the first branch of the ophthalmic artery, and what does it supply?
The first branch of the ophthalmic artery is the central retinal artery, which supplies the inner retina.
What are the three main capillary plexuses in the inner retina, and what do they supply?
The three main capillary plexuses in the inner retina are the superficial vascular complex, intermediate capillary plexus, and deep capillary plexus, which supply the inner retina.
What are the two types of posterior ciliary arteries, and what do they supply?
The two types of posterior ciliary arteries are short and long posterior ciliary arteries, which supply the choroid and optic nerve.
What are the two muscular branches of the ophthalmic artery, and what do they supply?
The two muscular branches of the ophthalmic artery are the superior and inferior branches, which supply the extrinsic eye muscles.
What is the lacrimal artery, and what does it supply?
The lacrimal artery is a branch of the ophthalmic artery, which supplies the lacrimal gland and surrounding structures.
What is the central retinal vein, and where does it empty?
The central retinal vein is the main vein that drains the inner retina, and it empties into the superior ophthalmic vein or cavernous sinus.
What is the superficial vascular complex, and what does it supply?
The superficial vascular complex is a network of capillaries that supplies the inner retina.
What is the cilioretinal artery, and what does it supply?
The cilioretinal artery is a branch of the short posterior ciliary artery, which supplies the fovea.
What is the circle of Zinn-Haller, and what does it supply?
The circle of Zinn-Haller is a circular anastomosis of arteries that supplies the optic nerve.
Which artery is the first branch of the ophthalmic artery?
Central retinal artery
Which of the following vessels does NOT directly supply the optic nerve?
Long posterior ciliary arteries
What is the characteristic bend of the cilioretinal artery?
As it leaves the disk margin
What is the pathway of blood from the inner retina?
Post capillary venules → Branched retinal veins → Central retinal vein
What is the function of the superficial vascular complex?
To supply the inner retina
Which of the following arteries is NOT a branch of the muscular artery?
Lacrimal artery
What is the purpose of the circle of Zinn-Haller?
To supply the optic nerve
Which vessel does the central retinal vein empty into?
Both superior ophthalmic vein and cavernous sinus
What is the origin of the ophthalmic artery?
Internal carotid artery
What is the function of the short posterior ciliary arteries?
To supply the choroid
Which artery is responsible for supplying the lacrimal sac and nose?
Sal nasal artery
Which veins drain the aqueous humour?
Anterior ciliary veins
Where do some vortex veins drain into?
Superior ophthalmic vein
How many vortex veins are typically found in a normal eye?
4 to 8
Where do the vortex veins drain the choroid?
Inferior ophthalmic vein
What is the pathway of the retinal drainage?
Central retinal vein → ophthalmic vein → cavernous sinus
What is the pathway of the conjunctival/episcleral drainage?
Anterior ciliary vein → ophthalmic vein → cavernous sinus
What is the pathway of the uveal drainage?
Vortex vein → superior ophthalmic vein → cavernous sinus and vortex vein → inferior ophthalmic vein → pterygoid plexus
Where does the superior ophthalmic vein exit?
Superior orbital fissure
Where does the inferior ophthalmic vein exit?
Inferior orbital fissure
What is the primary source of blood supply to the inner retina?
Central retinal artery
Which artery bifurcates into the ophthalmic artery as it exits the cavernous sinus?
Internal carotid artery
What is the characteristic feature of the cilioretinal artery?
It makes a characteristic bend as it leaves the disk margin
Which structure do the short posterior ciliary arteries supply?
Choroid
What is the destination of the central retinal vein?
All of the above
Which artery is responsible for supplying the lacrimal gland?
Lacrimal artery
What is the function of the muscular arteries?
Supply the extraocular muscles
Which artery is the first branch of the ophthalmic artery?
Central retinal artery
What is the function of the radial peripapillary capillary plexus?
Part of the superficial vascular complex
What is the destination of the posterior ciliary arteries?
All of the above
Which artery is responsible for supplying the lacrimal sac and nose?
Sal nasal artery
Which veins drain the choroid?
Vortex veins
Where do the anterior ciliary veins drain into?
Cavernous sinus
How many vortex veins are typically present in a normal eye?
4-8
What is the route of drainage for the aqueous humour?
Conjunctival/episcleral route
Where does the inferior ophthalmic vein exit?
Inferior orbital fissure
What is the drainage route for the retinal veins?
Central retinal vein → ophthalmic vein → cavernous sinus
What is the route of drainage for the uveal veins?
Vortex vein → superior ophthalmic vein → cavernous sinus
What is the function of the conjunctival/episcleral route?
To drain the aqueous humour
Where do the superior ophthalmic veins drain into?
Cavernous sinus
What are the components of the lid?
skin, muscle, fibrous tissue, mucous membrane, meibomian glands, and cilia (eyelashes)
What is the function of Riolan's muscle?
Prevents lipid expression unless eyelids touch during blink
What is the purpose of Müller's muscle?
Maintains upper lid elevation
What is the term for the inability to completely open the eyelids?
Ptosis
What is the term for the outward turn of the eyelid margin?
Ectropion
What is the function of the marginal conjunctiva?
Spreads tear film during blinks
Where is the highest density of goblet cells found in humans?
Nasal region
What percentage of the tear volume is found in the tear meniscus?
75-95%
What nerve carries the efferent lacrimal nerve?
CN7
What type of secretion do goblet cells exhibit?
Apocrine secretion
What is the pathway of tears from the puncta?
Puncta → Canaliculi → Lacrimal sac → Nasolacrimal duct
What type of nerves can activate goblet cells?
Sympathetic or parasympathetic nerves
What is the purpose of the upper eyelid during a blink?
To draw up tears from the meniscus and move them towards the nasal puncta
What is the overall structure of the tear film?
Blended phase model
What is entropion and how does it affect the cornea?
Entropion is a condition where the lid is rotated inwards towards the globe, causing corneal abrasion via lashes. This occurs due to tendon laxity or atrophy of lower lid muscles and tarsal atrophy.
Describe the innervation of the eyelid, including the sensory and motor components.
The eyelid receives sensory innervation from the trigeminal nerve (ophthalmic and maxillary divisions) and motor innervation from the levator muscle (CNIII, superior division), orbicularis muscle (CNVII), and Muller's muscle (sympathetic nervous system, from the superior cervical ganglion).
What is the composition of the tarsal plate, and what is its role in the eyelid?
The tarsal plate is composed of dense connective tissue and is studded with meibomian glands. It provides rigidity and shape to the eyelid.
Describe the structure and function of the palpebral conjunctiva, including its epithelium and stroma.
The palpebral conjunctiva consists of a stratified columnar mucoepithelium, thickest at the lid wiper, and a loose vascular stroma with lymphoid structures. It produces mucin and provides immune defense.
What is the role of the meibomian glands in the eyelid, and how do they contribute to the tear film?
The meibomian glands are sebaceous glands that produce the lipid layer of the tear film, which slows evaporation and prevents sebum from the lashes from entering the tear film. They are embedded in the tarsal plate and have multiple openings on the eyelid margin.
Describe the three layers of the tear film, including their composition and functions.
The tear film consists of a lipid layer (50-100 nm thick, composed of lipids and proteins), an aqueous layer (bulk of the tear film, containing water, electrolytes, proteins, and antimicrobials), and a mucin layer (produced by goblet cells, binds tears to the ocular surface).
What is the functional significance of Riolan's muscle in the eyelid?
Prevents lipid expression unless eyelids touch during blink
What is the primary function of Müller's muscle (aka superior tarsal muscle) in the upper eyelid?
Maintains upper lid elevation
What is the significance of the mucocutaneous junction in the eyelid?
Transition point from skin to palpebral conjunctiva
What is the consequence of lid wiper epitheliopathy?
Increased friction between lid wiper and ocular/contact lens surface
What is the primary function of the levator muscle in the upper eyelid?
Elevates the upper eyelid
What is the consequence of ectropion?
Outward turn of the eyelid margin
Describe the innervation of the eyelid and identify the nerves responsible for sensory and motor functions.
Sensory innervation of the eyelid is provided by the trigeminal nerve (ophthalmic [V1] and maxillary [V2] division), while motor innervation is provided by the trochlear nerve (CNIV), superior division of CNIII (levator), CNVII (orbicularis), and the sympathetic nervous system (Muller's).
What is the structure and function of the tarsal plate, and how does it relate to the meibomian glands?
The tarsal plate is a dense connective tissue that gives the eyelid its rigidity and shape, and is studded with meibomian glands. The meibomian glands are sebaceous glands that produce the lipid layer of the tear film.
Describe the layers of the tear film and their functions.
The tear film consists of three layers: the lipid layer (prevents evaporation and provides a barrier), the aqueous layer (provides oxygen and nutrients to the cornea), and the mucin layer (binds the tear film to the ocular surface).
What are the functions of the lacrimal gland, and how does it contribute to the tear film?
The lacrimal gland produces basal, reflex, and emotional tears, contributing to the aqueous layer of the tear film.
Describe the characteristics and function of the papillae and follicles in the palpebral conjunctiva.
Papillae are small, flat elevations of the conjunctiva, while follicles are larger, dome-shaped elevations. Both are indicative of inflammation or infection.
What is entropion, and what are the consequences of entropion on the cornea?
Entropion is a condition where the eyelid is rotated inward, towards the globe, due to tendon laxity or atrophy of the lower lid muscles. This causes the eyelashes to rub against the cornea, leading to corneal abrasion and potential vision damage.
In which region of the human body is the highest density of goblet cells found?
Nasal region
What percentage of tear volume is found in the tear meniscus?
75-95%
Which nerves are responsible for activating aqueous production in the lacrimal gland?
Parasympathetic and sympathetic efferent nerves
What is the pathway of tearing from the puncta to the nasal region?
Puncta → Canaliculi → Lacrimal sac → Nasolacrimal duct
What type of secretion do goblet cells use to produce mucin?
Apocrine secretion
What is the role of the upper eyelid during the blinking process?
Draws up tear from meniscus during opening phase and moves tear towards nasal puncta during closing phase
What is the efferent pathway for innervation of goblet cells?
Can be sympathetic or parasympathetic, and can also be activated by local factors (i.e. histamine)
What is the current understanding of the tear film structure?
A blended phase model
What is the function of the meibomian glands?
To produce the lipid layer of the tear film
What is the purpose of the palpebral conjunctiva?
To secrete mucin
What is the innervation of the orbicularis oculi muscle?
CN VII
What is the characteristic of the tarsal plate?
It is a dense connective tissue
What is the function of the lipid layer of the tear film?
To regulate tear evaporation
What is the location of the accessory lacrimal glands?
In the conjunctival fornix
Where is the highest density of goblet cells found in humans?
Nasal region
What percentage of tears is found in the tear meniscus?
75-95%
Which nerve carries efferent lacrimal nerve signals?
CN7
What is the primary function of the efferent lacrimal nerve?
Innervation of the lacrimal gland
What is the pathway of tear drainage?
Puncta -> canaliculi -> lacrimal sac -> nasolacrimal duct
What is the mechanism of mucin secretion by goblet cells?
Apocrine secretion
What type of efferent nerves can innervate goblet cells?
Either sympathetic or parasympathetic nerves
What is the current model of the tear film?
Blended phase model
Which part of the eyelid is responsible for spreading the tear film during blinks?
Marginal conjunctiva
What is the primary function of Riolan's muscle in the eyelid?
To prevent lipid expression unless the eyelids touch during a blink
What is the term for the inability to completely open the eyelids?
Ptosis
What type of epithelial cells are found in the palpebral conjunctiva at the mucocutaneous junction?
Cuboidal epithelial cells
Which muscle is responsible for maintaining the upper eyelid's elevation?
Müller's muscle
What is the term for the outward turning of the eyelid margin?
Ectropion
What is the characteristic feature of uveitis and what is its clinical relevance?
Ciliary flush (perilimbal injection); Clinical relevance: Subconjunctival haemorrhage.
Describe the venous drainage of palpebral and forniceal conjunctiva.
Veins from conjunctiva to venous plexus of eye lids, then to superior/inferior ophthalmic veins, and finally to cavernous sinus.
What is the route of lymph drainage from the conjunctiva?
Lateral side drains to superficial parotid nodes, medial side passes to submandibular nodes.
Describe the sensory innervation of the bulbar conjunctiva and superior palpebral and forniceal conjunctiva.
Bulbar conjunctiva: long ciliary nerves; Superior palpebral and forniceal conjunctiva: frontal and lacrimal branches of ophthalmic division of trigeminal nerve.
What is the characteristic feature of the venous drainage of bulbar conjunctiva?
A circumcorneal zone of veins 5-6 mm from limbus, which drain to anterior ciliary veins and then to ophthalmic veins, finally to cavernous sinus.
What is the primary function of the marginal conjunctiva?
To provide a transitional zone from skin to conjunctiva
What is the primary route for venous drainage of the palpebral and forniceal conjunctiva?
Venous plexus of eyelids
Which of the following is NOT a function of the palpebral conjunctiva?
To provide nourishment to the cornea
What is the primary function of the goblet cells in the conjunctiva?
To produce mucin
What is the characteristic feature of a subconjunctival haemorrhage?
Painless and usually self-healing
What is the primary blood supply to the conjunctiva?
Palpebral arcades
What is the nerve supply to the bulbar conjunctiva?
Long ciliary nerves
What is the primary function of the conjunctival lymph drainage?
Drainage of clear fluid from the blood plasma
What is the purpose of the fornix in the bulbar conjunctiva?
To provide a pocket for contact lenses
What is the anatomical location of the venous drainage of the bulbar conjunctiva?
A circumcorneal zone of veins 5-6 mm from the limbus
What is the characteristic feature of the limbus?
It is the junction between the conjunctiva and cornea
What is the primary function of the Langerhans cells in the conjunctiva?
To regulate mucosal immunity
What is the nerve supply to the superior palpebral and forniceal conjunctiva?
Frontal and lacrimal branches of the ophthalmic division
What is the characteristic feature of the plica semilunaris?
It is a vestigial remnant of the third eyelid
What is the purpose of the venous plexus of the eyelids?
Venous drainage of the palpebral and forniceal conjunctiva
What is the purpose of the caruncle?
To produce oil and sweat
What is the characteristic feature of uveitis?
Ciliary flush (perilimbal injection)
What is the anatomical location of the lymph drainage of the conjunctiva?
Medial side to submandibular nodes
What is the characteristic feature of the bulbar conjunctiva?
It is the thinnest part of the conjunctiva
What is the purpose of the anterior ciliary veins?
Venous drainage of the bulbar conjunctiva
What is the approximate percentage of scleral dry weight composed of collagen?
Around 90%
What is the name of the layer regarded as part of the choroid by some, but separated from the choroid by perichoroidal space?
Lamina fusca
What is the function of fibroblasts in the sclera?
To synthesise collagen, elastic, and reticular fibres
What is the name of the protein that binds collagen, fibrin, heparin, cell membranes, and various macromolecules?
Fibronectin
What is the approximate percentage of scleral dry weight composed of proteoglycans and glycosaminoglycans?
Around 1%
What is the name of the type of collagen that is predominant in the sclera?
Type I
What is the function of myofibroblasts in the sclera?
To synthesise collagen, elastic, and reticular fibres, and express contractile proteins
What is the name of the glycoprotein that is part of the amorphous ground substance in the sclera?
Fibronectin
What is the name of the structure that forms a meshwork of polypeptide chains running parallel to collagen fibrils in the sclera?
Elastic fibres
What is the approximate percentage of scleral dry weight composed of elastin?
Around 2%
What is the main reason for the heterologous nature of fibrils in the sclera?
To enable type I collagen fibrillogenesis
What is the typical thickness of the sclera in the equatorial region?
0.3-0.4mm
What is the primary function of the sclera in terms of refractive stability?
To keep eye length stable during IOP and blood pressure changes
What is the function of the episcleral arterial circle?
To supply the limbal, anterior conjunctival, and anterior episcleral tissues
What is the approximate change in axial length required to produce a 0.50D change in refractive error?
170μm
What is the function of the sclera in relation to the extraocular muscles?
To provide stable anchorage for the extraocular muscles
What is the primary function of the sclera in the eye?
To provide a framework for the eye
What is the name of the structure that facilitates ocular drainage through the sclera?
Intrascleral venous plexus
What is the characteristic feature of the scleral stroma?
Irregularly arranged lamellae
What is the approximate size of the anterior scleral foramen?
11.6mm horizontal, 10.6mm vertical
What is the purpose of the fibroblasts in the episclera?
To produce collagen
What is the characteristic feature of the episclera?
Loosely arranged collagen bundles
What is the name of the structure that the scleral fibres turn 90° to form?
Meninges
What is the weakest part of the outer eye?
Lamina cribrosa
What is the function of the episcleral collecting veins?
To drain blood and aqueous humour
What is the main component of the sclera?
Dense, irregular connective tissue
What is the primary function of the scleral stroma?
To provide a framework for the eye
What is the function of the sclera in relation to the ciliary muscle?
To oppose the contractile forces of the ciliary muscle
What is the purpose of the type III collagen in the sclera?
To enable type I collagen fibrillogenesis
What is the purpose of the minor foramina in the sclera?
To allow for the passage of nerves and blood vessels
Study Notes
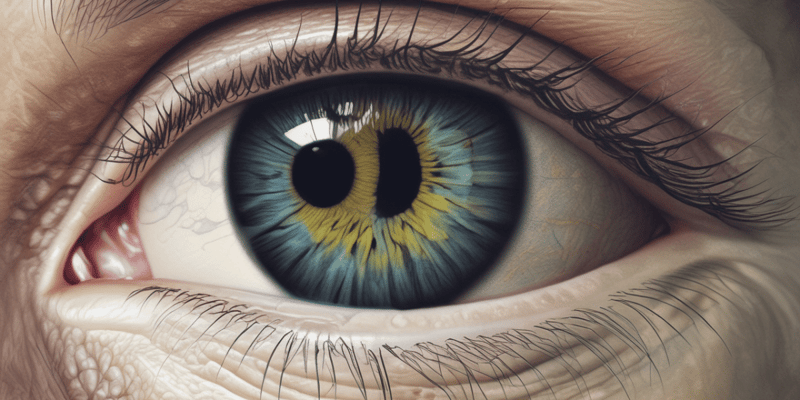
Anatomy of the Iris
- The iris is the most anterior component of the uvea (iris + ciliary body + choroid) and divides the anterior chamber from the posterior chamber.
- It is a highly vascularized, muscular diaphragm with a central opening (pupil) and is approximately 12 mm in diameter.
- The iris is composed of two zones: the peripheral ciliary zone (3-4 mm) that contains the dilator muscle, and the central pupillary zone (1-2 mm) that contains the sphincter muscle.
- The iris collarette is the meeting point between the two zones and is the thickest portion of the iris (~500 µm).
Pupil
- The pupil is a circular opening between the irises that dilates (enlarges) in low lighting conditions and constricts (narrows) in bright conditions.
- Pupil size tends to decrease with age and is symmetrical between the two eyes.
Iris Function
- The iris controls pupil size, modulating retinal illuminance to optimize vision.
- A small pupil minimizes aberrations and increases depth of focus.
- The iris blocks stray light and plays a role in social signaling, with constricted pupils when asleep and dilated pupils when excited.
Iris Histology
- The iris is composed of three layers: the anterior border layer, stroma, and pigmented epithelial layer (anterior and posterior).
- The anterior border layer is a modified stroma with a relatively dense network of fibroblasts, melanocytes, and collagen.
- The stroma is a loose collagenous matrix with fibroblasts, melanocytes, and large 'clump cells' that are phagocytes containing melanosomes.
- The pigmented epithelial layer is a single layer of lightly pigmented cells divided into apical and basal processes.
Iris Muscles
- The iris has two muscles: the sphincter (miosis) and dilator (mydriasis).
- The sphincter muscle is a flat annulus of smooth muscle at the pupil margin, 0.75-1 mm wide, and constricts the pupil.
- The dilator muscle is composed of radially oriented basal processes of anterior epithelial cells (myoepithelium) and dilates the pupil.
Iris Surface
- The anterior iris surface has thin, radial trabeculae (collagen columns) seen in light-colored irises and depressions or openings called crypts.
- The posterior iris surface is covered in melanocytes that prevent light from entering the eye other than through the pupil.
Iris Vasculature
- The iris receives its arterial supply from the major arterial circle via the long posterior and anterior ciliary arteries.
- Radial vessels in the iris stroma supply the iris and converge in a spiral pattern towards the pupil, forming radial ridges on the anterior iris surface.
- The vessels are non-fenestrated with tight junctions between endothelial cells, making them impermeable to macromolecules and conferring immune privilege.
Acknowledgement of Country
- The University of Western Australia acknowledges that its campus is situated on Noongar land, and that Noongar people remain the spiritual and cultural custodians of their land.
Anatomy of the Eye
The Globe
- The globe has 3 coats (tunics): outer (fibrous tunic), middle (vascular tunic/uvea), and inner (retina).
- Fluid layers maintain the globe's structure and function: tear film, aqueous humour, and vitreous humour.
- Four major tissue types in the globe: epithelial, connective, muscular, and neural tissues.
Cornea
- The cornea is 12 mm horizontally and 11 mm vertically, with a radius of curvature of approximately 8 mm.
- The cornea has 5 layers: non-keratinised stratified epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium.
Limbus
- The limbus is the junction between the cornea and sclera, approximately 1.75 mm wide.
- There is a sudden flattening of curvature at the limbus, forming the scleral sulcus.
Conjunctiva
- The conjunctiva is the outermost layer of the globe, covering the posterior surface of the lids.
- It is a loose mucous membrane containing blood vessels, nerves, lymphatics, and secretory glands.
- The conjunctiva has four components: forniceal, orbital, tarsal, and bulbar.
Tenon's Capsule
- Tenon's capsule is a dense connective tissue covering the eyeball (excluding the cornea) and extraocular muscles.
- It supports and protects the globe, forming a socket for the globe to move.
Episclera
- The episclera is a loose connective tissue beneath Tenon's capsule and above the sclera.
- It contains two vascular networks: the superficial plexus and the deep plexus, which provide nutrients to the sclera.
Sclera
- The sclera has three layers: episclera, scleral stroma, and lamina fusca.
- It is mainly composed of type I collagen and has a radius of curvature of approximately 12 mm.
- The sclera is the main load-bearing connective tissue, providing stable mechanical support.
Anterior Chamber
- The anterior chamber contains the cornea, iris, limbus, and drainage structures.
- The anterior chamber depth is approximately 3 mm, with an angle of 45°.
Anterior Chamber Angle
- The anterior chamber angle contains the trabecular meshwork, which facilitates drainage of the aqueous humour.
Iris
- The iris is the aperture of the eye, with a diameter of approximately 12 mm.
- The pupil ranges from 1-9 mm in diameter, and the iris has three layers: anterior border, stroma, and posterior epithelium.
Posterior Chamber
- The posterior chamber is located behind the iris, next to the ciliary body, and anterior to the lens.
- It contains aqueous humour produced by the ciliary processes and secreted into the posterior chamber.
Ciliary Body
- The ciliary body consists of two zones: the pars plicata (anterior) and the pars plana (posterior).
- The ciliary muscle is located in the ciliary stroma.
Lens
- The lens has three main structures: capsule, cortex, and nucleus.
- The lens epithelium is only present on the anterior surface, and produces lens fibres.
Posterior/Vitreous Chamber
- The posterior/vitreous chamber is located posterior to the lens and anterior to the retina, occupying approximately 80% of the globe's volume.
- It contains vitreous humour, which is enclosed by the vitreous/hyaloid membrane.
Retina
- The retina is a light-sensing film, approximately 0.5 mm thick, with a diameter of 30-40 mm.
- It is subdivided into inner and outer retina based on vascular supply.
Acknowledgement of Country
- The University of Western Australia acknowledges that its campus is situated on Noongar land, and that Noongar people remain the spiritual and cultural custodians of their land.
Anatomy of the Eye
The Globe
- The globe has 3 coats (tunics): outer (fibrous tunic), middle (vascular tunic/uvea), and inner (retina).
- Fluid layers maintain the globe's structure and function: tear film, aqueous humour, and vitreous humour.
- Four major tissue types in the globe: epithelial, connective, muscular, and neural tissues.
Cornea
- The cornea is 12 mm horizontally and 11 mm vertically, with a radius of curvature of approximately 8 mm.
- The cornea has 5 layers: non-keratinised stratified epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium.
Limbus
- The limbus is the junction between the cornea and sclera, approximately 1.75 mm wide.
- There is a sudden flattening of curvature at the limbus, forming the scleral sulcus.
Conjunctiva
- The conjunctiva is the outermost layer of the globe, covering the posterior surface of the lids.
- It is a loose mucous membrane containing blood vessels, nerves, lymphatics, and secretory glands.
- The conjunctiva has four components: forniceal, orbital, tarsal, and bulbar.
Tenon's Capsule
- Tenon's capsule is a dense connective tissue covering the eyeball (excluding the cornea) and extraocular muscles.
- It supports and protects the globe, forming a socket for the globe to move.
Episclera
- The episclera is a loose connective tissue beneath Tenon's capsule and above the sclera.
- It contains two vascular networks: the superficial plexus and the deep plexus, which provide nutrients to the sclera.
Sclera
- The sclera has three layers: episclera, scleral stroma, and lamina fusca.
- It is mainly composed of type I collagen and has a radius of curvature of approximately 12 mm.
- The sclera is the main load-bearing connective tissue, providing stable mechanical support.
Anterior Chamber
- The anterior chamber contains the cornea, iris, limbus, and drainage structures.
- The anterior chamber depth is approximately 3 mm, with an angle of 45°.
Anterior Chamber Angle
- The anterior chamber angle contains the trabecular meshwork, which facilitates drainage of the aqueous humour.
Iris
- The iris is the aperture of the eye, with a diameter of approximately 12 mm.
- The pupil ranges from 1-9 mm in diameter, and the iris has three layers: anterior border, stroma, and posterior epithelium.
Posterior Chamber
- The posterior chamber is located behind the iris, next to the ciliary body, and anterior to the lens.
- It contains aqueous humour produced by the ciliary processes and secreted into the posterior chamber.
Ciliary Body
- The ciliary body consists of two zones: the pars plicata (anterior) and the pars plana (posterior).
- The ciliary muscle is located in the ciliary stroma.
Lens
- The lens has three main structures: capsule, cortex, and nucleus.
- The lens epithelium is only present on the anterior surface, and produces lens fibres.
Posterior/Vitreous Chamber
- The posterior/vitreous chamber is located posterior to the lens and anterior to the retina, occupying approximately 80% of the globe's volume.
- It contains vitreous humour, which is enclosed by the vitreous/hyaloid membrane.
Retina
- The retina is a light-sensing film, approximately 0.5 mm thick, with a diameter of 30-40 mm.
- It is subdivided into inner and outer retina based on vascular supply.
Eyelid Anatomy and Function
- The eyelid is divided into three parts: orbital, preseptal, and pretarsal orbicularis muscles, which control eyelid movement and tear drainage.
- The orbicularis oculi muscle has three components: orbital orbicularis, preseptal orbicularis, and pretarsal orbicularis.
Muscles of the Eyelid
- The orbicularis oculi muscle is responsible for blinking, winking, and moving tears towards the drainage system.
- The muscle of Müller (superior tarsal muscle) is a smooth muscle that maintains upper eyelid elevation.
- The frontalis muscle is vertically orientated and draws the scalp forward, raising eyebrows.
- The corrugator muscle moves the brow medially, creating vertical furrows.
- The procerus muscle pulls the medial portion of the eyebrow inferiorly, producing horizontal furrows over the bridge of the nose.
Fascia and Fat
- Periorbita is a dense connective tissue and periosteum of the bony orbit.
- The capsule of Tenon is a fascial sheath surrounding the globe and optic nerve.
- Fat in the eyelids is composed of skin, muscle, fibrous tissue, fat, mucous membrane, meibomian glands, and cilia (eyelashes).
Tear Film
- The tear film is 7-10 µm thick and has three layers: mucin, water, and lipid.
- The functions of the tear film include ocular surface lubrication, debris removal, oxygen supply to the cornea, smooth refractive surface, antibacterial substances, and growth factors for repair.
- The lipid layer slows evaporation of the tear film, the aqueous layer provides protection with antibacterial molecules and growth factors, and the mucin layer binds the tear film to the ocular surface.
Tear Drainage
- Tear drainage occurs through the puncta, canaliculi, nasolacrimal sac, and nasolacrimal duct.
Muscle Histology
- Striated muscle:
- Named for the arrangement of contractile proteins giving a histological appearance of prominent cross-striations
- Specialized for forceful contractions of short duration
- Found in skeletal muscles and extraocular muscles
- Smooth muscle:
- Histological appearance does not show cross-striations
- Specialized for continuous contraction of relatively low force
- Found in blood vessels, ciliary muscle, and iris sphincter/dilator
- Cardiac muscle:
- Structural and functional characteristics intermediate between striated and smooth muscle
- Provides continuous, rhythmic contraction of the heart
Striated Muscle: Gross Anatomy
- Entire muscle enveloped in a connective tissue sheath, the epimysium
- Groups of muscle fibers arranged into fascicles separated by a connective tissue sheath, the perimysium
- Individual muscle fibers surrounded by endomysium
- Muscle fibers made up of longitudinally aligned myofibrils, which are composed of repeating sarcomeres
- Fibre: >1000 myofibril
- Sarcomere: alternating myosin + actin
- Tendon (dense, regular CT) attaches muscle to bone
Smooth Muscle
- Forms sheets/bundles/layers
- Contractile proteins not organized into regular sarcomeres, resulting in a smooth, unstriated appearance
- Smooth muscle cell, equivalent to striated muscle fibers
- Length: 12-200 µm
- Gap junction between cells allows electrical excitation to pass, producing coordinated waves of contraction
- Slow to contract and relax
- No tendon equivalent, dense plaques attach cell to the surrounding extracellular matrix/reticular layer
- Cell-cell attachment via desmosomes, formed by two adjacent dense plaques
Extraocular Muscles (EOM)
- 7 muscles: levator palpebrae, 2 obliques, and 4 recti
- Striated muscle, differing from skeletal muscle in fewer muscle fibers, denser blood supply, and more delicate connective tissue sheaths with more elastic fibers
- Two distinct regions: outer, orbital layer (40-60% myofibers) and inner, global layer
- Fiber types:
- Orbital layer: high number of mitochondria, small myofibrils, fast twitch, and fatigue-resistant
- Global layer: slow twitch, fatigue-resistant, and large myofibrils
- Insertion: differing distances from the limbus, with the medial rectus inserting closest and the superior rectus inserting farthest
- Innervation:
- CN III (Oculomotor Nerve): superior rectus, inferior rectus, medial rectus, and inferior oblique
- CN IV (Trochlear Nerve): superior oblique
- CN VI (Abducens Nerve): lateral rectus
- Blood supply:
- Superior (lateral) branch of ophthalmic artery: superior rectus, lateral rectus, and superior oblique
- Inferior (medial) branch of the ophthalmic artery: inferior rectus, medial rectus, and inferior oblique
- Actions:
- Medial rectus: adduction
- Lateral rectus: abduction
- Superior rectus: elevation, incyclotorsion, and adduction
- Inferior rectus: depression, excyclotorsion, and adduction
- Superior oblique: incyclotorsion, depression, and abduction
- Inferior oblique: excyclotorsion, elevation, and abduction
Other Muscles in the Orbit
- Levator muscle: responsible for raising the upper lid, originates at the orbital apex, and inserts into the upper lid posterior to the orbital septum and attaches to the anterior face of the superior tarsal plate
- Müller's muscle: smooth muscle that arises from the inferior surface of the levator muscle, inserts into the upper edge of the superior tarsal plate, and is responsible for increasing the width of the palpebral aperture during fear or excitement
Muscle Histology
- Striated muscle:
- Named for the arrangement of contractile proteins giving a histological appearance of prominent cross-striations
- Specialized for forceful contractions of short duration
- Found in skeletal muscles and extraocular muscles
- Smooth muscle:
- Histological appearance does not show cross-striations
- Specialized for continuous contraction of relatively low force
- Found in blood vessels, ciliary muscle, and iris sphincter/dilator
- Cardiac muscle:
- Structural and functional characteristics intermediate between striated and smooth muscle
- Provides continuous, rhythmic contraction of the heart
Striated Muscle: Gross Anatomy
- Entire muscle enveloped in a connective tissue sheath, the epimysium
- Groups of muscle fibers arranged into fascicles separated by a connective tissue sheath, the perimysium
- Individual muscle fibers surrounded by endomysium
- Muscle fibers made up of longitudinally aligned myofibrils, which are composed of repeating sarcomeres
- Fibre: >1000 myofibril
- Sarcomere: alternating myosin + actin
- Tendon (dense, regular CT) attaches muscle to bone
Smooth Muscle
- Forms sheets/bundles/layers
- Contractile proteins not organized into regular sarcomeres, resulting in a smooth, unstriated appearance
- Smooth muscle cell, equivalent to striated muscle fibers
- Length: 12-200 µm
- Gap junction between cells allows electrical excitation to pass, producing coordinated waves of contraction
- Slow to contract and relax
- No tendon equivalent, dense plaques attach cell to the surrounding extracellular matrix/reticular layer
- Cell-cell attachment via desmosomes, formed by two adjacent dense plaques
Extraocular Muscles (EOM)
- 7 muscles: levator palpebrae, 2 obliques, and 4 recti
- Striated muscle, differing from skeletal muscle in fewer muscle fibers, denser blood supply, and more delicate connective tissue sheaths with more elastic fibers
- Two distinct regions: outer, orbital layer (40-60% myofibers) and inner, global layer
- Fiber types:
- Orbital layer: high number of mitochondria, small myofibrils, fast twitch, and fatigue-resistant
- Global layer: slow twitch, fatigue-resistant, and large myofibrils
- Insertion: differing distances from the limbus, with the medial rectus inserting closest and the superior rectus inserting farthest
- Innervation:
- CN III (Oculomotor Nerve): superior rectus, inferior rectus, medial rectus, and inferior oblique
- CN IV (Trochlear Nerve): superior oblique
- CN VI (Abducens Nerve): lateral rectus
- Blood supply:
- Superior (lateral) branch of ophthalmic artery: superior rectus, lateral rectus, and superior oblique
- Inferior (medial) branch of the ophthalmic artery: inferior rectus, medial rectus, and inferior oblique
- Actions:
- Medial rectus: adduction
- Lateral rectus: abduction
- Superior rectus: elevation, incyclotorsion, and adduction
- Inferior rectus: depression, excyclotorsion, and adduction
- Superior oblique: incyclotorsion, depression, and abduction
- Inferior oblique: excyclotorsion, elevation, and abduction
Other Muscles in the Orbit
- Levator muscle: responsible for raising the upper lid, originates at the orbital apex, and inserts into the upper lid posterior to the orbital septum and attaches to the anterior face of the superior tarsal plate
- Müller's muscle: smooth muscle that arises from the inferior surface of the levator muscle, inserts into the upper edge of the superior tarsal plate, and is responsible for increasing the width of the palpebral aperture during fear or excitement
The Nervous System
- Divided into two sub-systems:
- Central nervous system (CNS): brain and spinal cord
- Peripheral nervous system (PNS): spinal and cranial nerves
- Responsible for sending, receiving, and interpreting messages from the body
- CNS: processing center, regulates complex functions throughout the body, assists the whole body to adapt quickly
Peripheral Nervous System (PNS)
- Sends and receives info to/from CNS
- Divided into two components:
- Autonomic nervous system (involuntary)
- Somatic nervous system (voluntary)
- Autonomic nervous system:
- Controls involuntary actions (e.g., heart rate, digestion)
- Divided into three parts:
- Sympathetic nervous system: mobilization of energy stores for increased activity (fight-or-flight)
- Parasympathetic nervous system: conservation of energy stores
- Enteric nervous system: neurons intrinsic to the gastrointestinal tract
- Somatic nervous system:
- Controls voluntary motor fibers to skeletal muscle
- Afferent/sensory nerves and efferent/motor nerves
Cranial Nerves
- 12 pairs of cranial nerves
- Transmit sensory information from the head and neck to the brain
- Control the actions of the head and neck
- Organization:
- Motor and/or sensory nerves
- Comprise a central nucleus in the brain and a peripheral nerve fiber
Cranial Nerve Functions
- CN I – Olfactory nerve: olfaction (sensory)
- CN II – Optic nerve: vision (sensory)
- CN III – Oculomotor nerve: movement of eye, elevation of upper lid (motor), pupillary constriction and accommodation (parasympathetic)
- CN IV – Trochlear nerve: movement of eye (motor)
- CN V – Trigeminal nerve:
- Ophthalmic branch: sensation from forehead, scalp, eyelids, nose, and eye (cornea and conjunctiva)
- Maxillary branch: sensation from skin of anterior temporal and upper cheek, palate, teeth, maxillary sinus
- Mandibular branch: motor to masticatory muscles, sensory to anterior 2/3 of tongue, skin posterior temporal, cheek, chin, teeth, lower jaw
- ... (functions of remaining cranial nerves)
Additional Important Concepts
- Oculocardiac reflex: decrease in heart rate following globe pressure or traction of extraocular muscles, causing dizziness and fainting, notable in strabismus surgery
The Nervous System
- Divided into two sub-systems:
- Central nervous system (CNS): brain and spinal cord
- Peripheral nervous system (PNS): spinal and cranial nerves
- Responsible for sending, receiving, and interpreting messages from the body
- CNS: processing center, regulates complex functions throughout the body, assists the whole body to adapt quickly
Peripheral Nervous System (PNS)
- Sends and receives info to/from CNS
- Divided into two components:
- Autonomic nervous system (involuntary)
- Somatic nervous system (voluntary)
- Autonomic nervous system:
- Controls involuntary actions (e.g., heart rate, digestion)
- Divided into three parts:
- Sympathetic nervous system: mobilization of energy stores for increased activity (fight-or-flight)
- Parasympathetic nervous system: conservation of energy stores
- Enteric nervous system: neurons intrinsic to the gastrointestinal tract
- Somatic nervous system:
- Controls voluntary motor fibers to skeletal muscle
- Afferent/sensory nerves and efferent/motor nerves
Cranial Nerves
- 12 pairs of cranial nerves
- Transmit sensory information from the head and neck to the brain
- Control the actions of the head and neck
- Organization:
- Motor and/or sensory nerves
- Comprise a central nucleus in the brain and a peripheral nerve fiber
Cranial Nerve Functions
- CN I – Olfactory nerve: olfaction (sensory)
- CN II – Optic nerve: vision (sensory)
- CN III – Oculomotor nerve: movement of eye, elevation of upper lid (motor), pupillary constriction and accommodation (parasympathetic)
- CN IV – Trochlear nerve: movement of eye (motor)
- CN V – Trigeminal nerve:
- Ophthalmic branch: sensation from forehead, scalp, eyelids, nose, and eye (cornea and conjunctiva)
- Maxillary branch: sensation from skin of anterior temporal and upper cheek, palate, teeth, maxillary sinus
- Mandibular branch: motor to masticatory muscles, sensory to anterior 2/3 of tongue, skin posterior temporal, cheek, chin, teeth, lower jaw
- ... (functions of remaining cranial nerves)
Additional Important Concepts
- Oculocardiac reflex: decrease in heart rate following globe pressure or traction of extraocular muscles, causing dizziness and fainting, notable in strabismus surgery
Blood Supply to the Eye
- Blood to the eye comes from the right atrium, through the pulmonary artery, lung, pulmonary vein, left atrium, left ventricle, and aorta.
- The right and left internal carotid arteries supply the right and left eyes, respectively.
- The internal carotid artery runs through the neck, enters the cranial vault via the carotid canal, and then into the cavernous sinus.
- It bifurcates into the ophthalmic artery as it exits the cavernous sinus.
Ophthalmic Artery
- The ophthalmic artery enters the orbit via the optic canal (along with the optic nerve) and bifurcates into multiple arteries.
- The central retinal artery is the first branch of the ophthalmic artery.
- It pierces the dura ~ 1 cm from the globe and enters the optic nerve.
- The central retinal artery has many collateral branches that serve the optic nerve fibers prior to the optic nerve head.
- It exits the optic nerve and is visible when viewing the fundus.
Inner Retinal Supply
- The inner retina has a dual blood supply: short posterior choroid and anterior optic nerve, and long posterior choroid and ciliary body.
- The cilioretinal artery arises from the short posterior ciliary artery and makes a characteristic bend as it leaves the disk margin.
- It is present in ~30% of the population and supplies the fovea.
Superficial Vascular Complex
- The superficial vascular complex consists of the radial peripapillary capillary plexus, superficial vascular plexus, intermediate capillary plexus, and deep capillary plexus.
Inner Retinal Venous Return
- The post-capillary venules drain into the branched retinal veins, which then drain into the central retinal vein.
- The central retinal vein empties into the superior ophthalmic vein or cavernous sinus (different between people).
Short Posterior Ciliary Arteries
- The short posterior ciliary arteries pierce the sclera in an annulus around the optic nerve head and supply the choroid.
- Other branches form the circle of Zinn Haller to supply the optic nerve.
Long Posterior Ciliary Arteries
- The long posterior ciliary arteries pierce the posterior sclera to supply the choroid.
- They then join the major circle of the iris to supply the ciliary body and iris.
Muscular Arteries
- The muscular arteries arise from the ophthalmic artery and have two branches:
- Superior branch, which runs laterally and supplies the levator, superior rectus, superior oblique, and partially lateral rectus.
- Inferior branch, which runs medially and supplies the inferior rectus, inferior oblique, and anterior ciliary arteries.
Anterior Ciliary Arteries
- The anterior ciliary arteries branch from the muscular arteries.
- One branch joins the major circle of the iris, while the other branch supplies the episclera and conjunctiva.
Lateral Branches
- The lacrimal artery is the 2nd branch off the ophthalmic artery and runs along the orbital wall with the lateral rectus.
- It has three branches:
- Muscular branch, which supplies the lateral and superior rectus muscle.
- Glandular branch, which supplies the lacrimal gland.
- Recurrent branch, which anastomoses with the meninges.
Zygomatic Artery
- The zygomatic artery is a branch off the lacrimal artery before the lacrimal gland.
- It supplies the orbicularis and other facial muscles.
Lateral Palpebral Artery
- The lateral palpebral artery is the terminal branch of the lacrimal artery.
- It supplies the lower and upper lids.
- It anastomoses with the medial palpebral artery.
Medial Branches
- The supraorbital artery arises from the ophthalmic artery and supplies the periosteum of the frontal bone, skin of the forehead, superior rectus, and palpebrae superioris.
- The supratrochlear artery arises from the ophthalmic artery and supplies the forehead and scalp.
- The dorsal nasal artery is the terminal branch of the lacrimal artery and supplies the lacrimal sac and nose.
Conjunctival/Episcleral Return
- The conjunctival/episcleral return drains to the anterior ciliary veins, which then drain into the ophthalmic veins.
- Aqueous humor also drains via this route.
Vortex/Vorticose Veins
- The vortex veins drain the choroid.
- Some vortex veins drain into the superior ophthalmic vein, while others drain into the inferior ophthalmic vein.
- The superior ophthalmic vein exits via the superior orbital fissure and drains into the cavernous sinus.
- The inferior ophthalmic vein exits via the inferior orbital fissure and drains into the pterygoid plexus.
- A normal eye has 4 to 8 vortex veins, at least 1 vein in each quadrant.
Summary
- Retinal drainage: central retinal vein → ophthalmic vein → cavernous sinus.
- Conjunctival/episcleral drainage: anterior ciliary vein → cavernous sinus.
- Uveal drainage: vortex vein → superior ophthalmic vein → cavernous sinus or vortex vein → inferior ophthalmic vein → pterygoid plexus.
Blood Supply to the Eye
- Blood to the eye comes from the right atrium, through the pulmonary artery, lung, pulmonary vein, left atrium, left ventricle, and aorta.
- The right and left internal carotid arteries supply the right and left eyes, respectively.
- The internal carotid artery runs through the neck, enters the cranial vault via the carotid canal, and then into the cavernous sinus.
- It bifurcates into the ophthalmic artery as it exits the cavernous sinus.
Ophthalmic Artery
- The ophthalmic artery enters the orbit via the optic canal (along with the optic nerve) and bifurcates into multiple arteries.
- The central retinal artery is the first branch of the ophthalmic artery.
- It pierces the dura ~ 1 cm from the globe and enters the optic nerve.
- The central retinal artery has many collateral branches that serve the optic nerve fibers prior to the optic nerve head.
- It exits the optic nerve and is visible when viewing the fundus.
Inner Retinal Supply
- The inner retina has a dual blood supply: short posterior choroid and anterior optic nerve, and long posterior choroid and ciliary body.
- The cilioretinal artery arises from the short posterior ciliary artery and makes a characteristic bend as it leaves the disk margin.
- It is present in ~30% of the population and supplies the fovea.
Superficial Vascular Complex
- The superficial vascular complex consists of the radial peripapillary capillary plexus, superficial vascular plexus, intermediate capillary plexus, and deep capillary plexus.
Inner Retinal Venous Return
- The post-capillary venules drain into the branched retinal veins, which then drain into the central retinal vein.
- The central retinal vein empties into the superior ophthalmic vein or cavernous sinus (different between people).
Short Posterior Ciliary Arteries
- The short posterior ciliary arteries pierce the sclera in an annulus around the optic nerve head and supply the choroid.
- Other branches form the circle of Zinn Haller to supply the optic nerve.
Long Posterior Ciliary Arteries
- The long posterior ciliary arteries pierce the posterior sclera to supply the choroid.
- They then join the major circle of the iris to supply the ciliary body and iris.
Muscular Arteries
- The muscular arteries arise from the ophthalmic artery and have two branches:
- Superior branch, which runs laterally and supplies the levator, superior rectus, superior oblique, and partially lateral rectus.
- Inferior branch, which runs medially and supplies the inferior rectus, inferior oblique, and anterior ciliary arteries.
Anterior Ciliary Arteries
- The anterior ciliary arteries branch from the muscular arteries.
- One branch joins the major circle of the iris, while the other branch supplies the episclera and conjunctiva.
Lateral Branches
- The lacrimal artery is the 2nd branch off the ophthalmic artery and runs along the orbital wall with the lateral rectus.
- It has three branches:
- Muscular branch, which supplies the lateral and superior rectus muscle.
- Glandular branch, which supplies the lacrimal gland.
- Recurrent branch, which anastomoses with the meninges.
Zygomatic Artery
- The zygomatic artery is a branch off the lacrimal artery before the lacrimal gland.
- It supplies the orbicularis and other facial muscles.
Lateral Palpebral Artery
- The lateral palpebral artery is the terminal branch of the lacrimal artery.
- It supplies the lower and upper lids.
- It anastomoses with the medial palpebral artery.
Medial Branches
- The supraorbital artery arises from the ophthalmic artery and supplies the periosteum of the frontal bone, skin of the forehead, superior rectus, and palpebrae superioris.
- The supratrochlear artery arises from the ophthalmic artery and supplies the forehead and scalp.
- The dorsal nasal artery is the terminal branch of the lacrimal artery and supplies the lacrimal sac and nose.
Conjunctival/Episcleral Return
- The conjunctival/episcleral return drains to the anterior ciliary veins, which then drain into the ophthalmic veins.
- Aqueous humor also drains via this route.
Vortex/Vorticose Veins
- The vortex veins drain the choroid.
- Some vortex veins drain into the superior ophthalmic vein, while others drain into the inferior ophthalmic vein.
- The superior ophthalmic vein exits via the superior orbital fissure and drains into the cavernous sinus.
- The inferior ophthalmic vein exits via the inferior orbital fissure and drains into the pterygoid plexus.
- A normal eye has 4 to 8 vortex veins, at least 1 vein in each quadrant.
Summary
- Retinal drainage: central retinal vein → ophthalmic vein → cavernous sinus.
- Conjunctival/episcleral drainage: anterior ciliary vein → cavernous sinus.
- Uveal drainage: vortex vein → superior ophthalmic vein → cavernous sinus or vortex vein → inferior ophthalmic vein → pterygoid plexus.
Blood Supply to the Eye
- Blood to the eye comes from the right atrium, through the pulmonary artery, lung, pulmonary vein, left atrium, left ventricle, and aorta.
- The right and left internal carotid arteries supply the right and left eyes, respectively.
- The internal carotid artery runs through the neck, enters the cranial vault via the carotid canal, and then into the cavernous sinus.
- It bifurcates into the ophthalmic artery as it exits the cavernous sinus.
Ophthalmic Artery
- The ophthalmic artery enters the orbit via the optic canal (along with the optic nerve) and bifurcates into multiple arteries.
- The central retinal artery is the first branch of the ophthalmic artery.
- It pierces the dura ~ 1 cm from the globe and enters the optic nerve.
- The central retinal artery has many collateral branches that serve the optic nerve fibers prior to the optic nerve head.
- It exits the optic nerve and is visible when viewing the fundus.
Inner Retinal Supply
- The inner retina has a dual blood supply: short posterior choroid and anterior optic nerve, and long posterior choroid and ciliary body.
- The cilioretinal artery arises from the short posterior ciliary artery and makes a characteristic bend as it leaves the disk margin.
- It is present in ~30% of the population and supplies the fovea.
Superficial Vascular Complex
- The superficial vascular complex consists of the radial peripapillary capillary plexus, superficial vascular plexus, intermediate capillary plexus, and deep capillary plexus.
Inner Retinal Venous Return
- The post-capillary venules drain into the branched retinal veins, which then drain into the central retinal vein.
- The central retinal vein empties into the superior ophthalmic vein or cavernous sinus (different between people).
Short Posterior Ciliary Arteries
- The short posterior ciliary arteries pierce the sclera in an annulus around the optic nerve head and supply the choroid.
- Other branches form the circle of Zinn Haller to supply the optic nerve.
Long Posterior Ciliary Arteries
- The long posterior ciliary arteries pierce the posterior sclera to supply the choroid.
- They then join the major circle of the iris to supply the ciliary body and iris.
Muscular Arteries
- The muscular arteries arise from the ophthalmic artery and have two branches:
- Superior branch, which runs laterally and supplies the levator, superior rectus, superior oblique, and partially lateral rectus.
- Inferior branch, which runs medially and supplies the inferior rectus, inferior oblique, and anterior ciliary arteries.
Anterior Ciliary Arteries
- The anterior ciliary arteries branch from the muscular arteries.
- One branch joins the major circle of the iris, while the other branch supplies the episclera and conjunctiva.
Lateral Branches
- The lacrimal artery is the 2nd branch off the ophthalmic artery and runs along the orbital wall with the lateral rectus.
- It has three branches:
- Muscular branch, which supplies the lateral and superior rectus muscle.
- Glandular branch, which supplies the lacrimal gland.
- Recurrent branch, which anastomoses with the meninges.
Zygomatic Artery
- The zygomatic artery is a branch off the lacrimal artery before the lacrimal gland.
- It supplies the orbicularis and other facial muscles.
Lateral Palpebral Artery
- The lateral palpebral artery is the terminal branch of the lacrimal artery.
- It supplies the lower and upper lids.
- It anastomoses with the medial palpebral artery.
Medial Branches
- The supraorbital artery arises from the ophthalmic artery and supplies the periosteum of the frontal bone, skin of the forehead, superior rectus, and palpebrae superioris.
- The supratrochlear artery arises from the ophthalmic artery and supplies the forehead and scalp.
- The dorsal nasal artery is the terminal branch of the lacrimal artery and supplies the lacrimal sac and nose.
Conjunctival/Episcleral Return
- The conjunctival/episcleral return drains to the anterior ciliary veins, which then drain into the ophthalmic veins.
- Aqueous humor also drains via this route.
Vortex/Vorticose Veins
- The vortex veins drain the choroid.
- Some vortex veins drain into the superior ophthalmic vein, while others drain into the inferior ophthalmic vein.
- The superior ophthalmic vein exits via the superior orbital fissure and drains into the cavernous sinus.
- The inferior ophthalmic vein exits via the inferior orbital fissure and drains into the pterygoid plexus.
- A normal eye has 4 to 8 vortex veins, at least 1 vein in each quadrant.
Summary
- Retinal drainage: central retinal vein → ophthalmic vein → cavernous sinus.
- Conjunctival/episcleral drainage: anterior ciliary vein → cavernous sinus.
- Uveal drainage: vortex vein → superior ophthalmic vein → cavernous sinus or vortex vein → inferior ophthalmic vein → pterygoid plexus.
Lid Anatomy
- Comprised of skin, muscle, fibrous tissue, mucous membrane, meibomian glands, and cilia (eyelashes)
- Skin: stratified squamous keratinized epithelium, transitions to cuboidal epithelial cells of the palpebral conjunctiva at the mucocutaneous junction
- Lid wiper epitheliopathy: increased friction between lid wiper and ocular/contact lens surface
Muscles of the Lid
- Orbicularis oculi: most anterior muscle group, consists of palpebral (preseptal, pretarsal) and orbital portions
- Riolan's muscle: prevents lipid expression unless eyelids touch during blink
- Levator: elevates upper eyelid
- Müller's muscle (aka superior tarsal muscle): smooth muscle, sympathetic innervation, maintains upper lid elevation
- Upper lid responsible for most of the palpebral opening
Ligaments and Tendons
- Lids muscles attached laterally and medially to tendons
- Transverse ligaments within the lids (affects eyelid apposition if becomes tight/loose)
Innervation
- Sensory: trigeminal (ophthalmic [V1] and maxillary [V2] division)
- Motor:
- Levator: CNIII, superior division
- Orbicularis: CNVII
- Müller's: sympathetic nervous system, from superior cervical ganglion
Tarsal Plate
- Dense connective tissue
- Gives lid rigidity and shape
- Studded with meibomian glands
Vessels in the Tarsal Conj
- Highly vascularized, supply from lateral and medial palpebral arteries
- Clinically, inflamed tarsal conj presents as papillae/follicles
Palpebral Conjunctiva
- Consists of epithelium + stroma
- Epithelium: stratified columnar mucoepithelium, thickest at lid wiper
- Stroma: loose vascular tissue with lymphoid structures
Glands of the Lid
- Lacrimal gland:
- Produces basal + reflex + emotional tears
- Glands of Moll & Zeis:
- Zeis: sebaceous gland, exact function unknown
- Moll: apocrine gland, immune defense
- Meibomian glands:
- Sebaceous glands producing lipid layer (oil) of tear film
- Embedded in the tarsal plate
- Long & multilobed
- Openings on eyelid margin
- Upper lid: 30-40
- Lower lid: 20-30
- Accessory lacrimal glands:
- Contribute to 5% of water component
- Similar functions, differ in location
- Krause: conjunctival fornix
- Wolfring: border of tarsal plate
- Produce basal tears
Tear Film
- Layers:
- Lipid layer:
- Thinnest layer
- Slows evaporation of the tear film
- Aqueous layer:
- Main bulk of tear film
- Protection: antibacterial molecules & growth factor
- Mucin layer:
- Binds tears film to ocular surface
- Lipid layer:
- The distinct, three-layered structure is superseded by multiple blended-phase (i.e. lipid layer, aqueous layer with graded concentration of mucin)
Lipid Layer/Meibum
- 50 – 100 nm thick
- Complex mixture of lipids and proteins
- Most stored in the meibomian gland ducts
- Released onto ocular surface with each blink
- Prevents evaporation of aqueous layer/prevents sebum from lashes entering tear film
Aqueous Layer
- Bulk of the tears
- Complex mixture of water, electrolytes, proteins, and antimicrobials
- Provides O2 and nutrients to the cornea
- Note that there is a GRADED concentration of mucin within the aqueous layer, not separate aqueous and mucin layers
Mucin Layer
- Produced by goblet cells in the conjunctiva
- Distribution varies amongst species
- In humans, highest density in nasal region
- Goblet cells secrete mucin via apocrine secretion
Lid Anatomy
- Comprised of skin, muscle, fibrous tissue, mucous membrane, meibomian glands, and cilia (eyelashes)
- Skin: stratified squamous keratinized epithelium, transitions to cuboidal epithelial cells of the palpebral conjunctiva at the mucocutaneous junction
- Lid wiper epitheliopathy: increased friction between lid wiper and ocular/contact lens surface
Muscles of the Lid
- Orbicularis oculi: most anterior muscle group, consists of palpebral (preseptal, pretarsal) and orbital portions
- Riolan's muscle: prevents lipid expression unless eyelids touch during blink
- Levator: elevates upper eyelid
- Müller's muscle (aka superior tarsal muscle): smooth muscle, sympathetic innervation, maintains upper lid elevation
- Upper lid responsible for most of the palpebral opening
Ligaments and Tendons
- Lids muscles attached laterally and medially to tendons
- Transverse ligaments within the lids (affects eyelid apposition if becomes tight/loose)
Innervation
- Sensory: trigeminal (ophthalmic [V1] and maxillary [V2] division)
- Motor:
- Levator: CNIII, superior division
- Orbicularis: CNVII
- Müller's: sympathetic nervous system, from superior cervical ganglion
Tarsal Plate
- Dense connective tissue
- Gives lid rigidity and shape
- Studded with meibomian glands
Vessels in the Tarsal Conj
- Highly vascularized, supply from lateral and medial palpebral arteries
- Clinically, inflamed tarsal conj presents as papillae/follicles
Palpebral Conjunctiva
- Consists of epithelium + stroma
- Epithelium: stratified columnar mucoepithelium, thickest at lid wiper
- Stroma: loose vascular tissue with lymphoid structures
Glands of the Lid
- Lacrimal gland:
- Produces basal + reflex + emotional tears
- Glands of Moll & Zeis:
- Zeis: sebaceous gland, exact function unknown
- Moll: apocrine gland, immune defense
- Meibomian glands:
- Sebaceous glands producing lipid layer (oil) of tear film
- Embedded in the tarsal plate
- Long & multilobed
- Openings on eyelid margin
- Upper lid: 30-40
- Lower lid: 20-30
- Accessory lacrimal glands:
- Contribute to 5% of water component
- Similar functions, differ in location
- Krause: conjunctival fornix
- Wolfring: border of tarsal plate
- Produce basal tears
Tear Film
- Layers:
- Lipid layer:
- Thinnest layer
- Slows evaporation of the tear film
- Aqueous layer:
- Main bulk of tear film
- Protection: antibacterial molecules & growth factor
- Mucin layer:
- Binds tears film to ocular surface
- Lipid layer:
- The distinct, three-layered structure is superseded by multiple blended-phase (i.e. lipid layer, aqueous layer with graded concentration of mucin)
Lipid Layer/Meibum
- 50 – 100 nm thick
- Complex mixture of lipids and proteins
- Most stored in the meibomian gland ducts
- Released onto ocular surface with each blink
- Prevents evaporation of aqueous layer/prevents sebum from lashes entering tear film
Aqueous Layer
- Bulk of the tears
- Complex mixture of water, electrolytes, proteins, and antimicrobials
- Provides O2 and nutrients to the cornea
- Note that there is a GRADED concentration of mucin within the aqueous layer, not separate aqueous and mucin layers
Mucin Layer
- Produced by goblet cells in the conjunctiva
- Distribution varies amongst species
- In humans, highest density in nasal region
- Goblet cells secrete mucin via apocrine secretion
Lid Anatomy
- Comprised of skin, muscle, fibrous tissue, mucous membrane, meibomian glands, and cilia (eyelashes)
- Skin: stratified squamous keratinized epithelium, transitions to cuboidal epithelial cells of the palpebral conjunctiva at the mucocutaneous junction
- Lid wiper epitheliopathy: increased friction between lid wiper and ocular/contact lens surface
Muscles of the Lid
- Orbicularis oculi: most anterior muscle group, consists of palpebral (preseptal, pretarsal) and orbital portions
- Riolan's muscle: prevents lipid expression unless eyelids touch during blink
- Levator: elevates upper eyelid
- Müller's muscle (aka superior tarsal muscle): smooth muscle, sympathetic innervation, maintains upper lid elevation
- Upper lid responsible for most of the palpebral opening
Ligaments and Tendons
- Lids muscles attached laterally and medially to tendons
- Transverse ligaments within the lids (affects eyelid apposition if becomes tight/loose)
Innervation
- Sensory: trigeminal (ophthalmic [V1] and maxillary [V2] division)
- Motor:
- Levator: CNIII, superior division
- Orbicularis: CNVII
- Müller's: sympathetic nervous system, from superior cervical ganglion
Tarsal Plate
- Dense connective tissue
- Gives lid rigidity and shape
- Studded with meibomian glands
Vessels in the Tarsal Conj
- Highly vascularized, supply from lateral and medial palpebral arteries
- Clinically, inflamed tarsal conj presents as papillae/follicles
Palpebral Conjunctiva
- Consists of epithelium + stroma
- Epithelium: stratified columnar mucoepithelium, thickest at lid wiper
- Stroma: loose vascular tissue with lymphoid structures
Glands of the Lid
- Lacrimal gland:
- Produces basal + reflex + emotional tears
- Glands of Moll & Zeis:
- Zeis: sebaceous gland, exact function unknown
- Moll: apocrine gland, immune defense
- Meibomian glands:
- Sebaceous glands producing lipid layer (oil) of tear film
- Embedded in the tarsal plate
- Long & multilobed
- Openings on eyelid margin
- Upper lid: 30-40
- Lower lid: 20-30
- Accessory lacrimal glands:
- Contribute to 5% of water component
- Similar functions, differ in location
- Krause: conjunctival fornix
- Wolfring: border of tarsal plate
- Produce basal tears
Tear Film
- Layers:
- Lipid layer:
- Thinnest layer
- Slows evaporation of the tear film
- Aqueous layer:
- Main bulk of tear film
- Protection: antibacterial molecules & growth factor
- Mucin layer:
- Binds tears film to ocular surface
- Lipid layer:
- The distinct, three-layered structure is superseded by multiple blended-phase (i.e. lipid layer, aqueous layer with graded concentration of mucin)
Lipid Layer/Meibum
- 50 – 100 nm thick
- Complex mixture of lipids and proteins
- Most stored in the meibomian gland ducts
- Released onto ocular surface with each blink
- Prevents evaporation of aqueous layer/prevents sebum from lashes entering tear film
Aqueous Layer
- Bulk of the tears
- Complex mixture of water, electrolytes, proteins, and antimicrobials
- Provides O2 and nutrients to the cornea
- Note that there is a GRADED concentration of mucin within the aqueous layer, not separate aqueous and mucin layers
Mucin Layer
- Produced by goblet cells in the conjunctiva
- Distribution varies amongst species
- In humans, highest density in nasal region
- Goblet cells secrete mucin via apocrine secretion
Structure of the Conjunctiva
- The conjunctiva consists of 2 layers: epithelium and stroma.
- Epithelium: 2-7 cell layers thick, depending on location, and contains goblet cells.
- Stroma: a connective tissue layer beneath the epithelium, housing blood vessels, nerves, and specialized cells.
Types of Conjunctiva
- Marginal conjunctiva: a transition zone from skin to conjunctiva, consisting of 5-7 layers of non-keratinized stratified squamous epithelium.
- Palpebral conjunctiva: firmly attached to the inner surface of eyelids, consisting of 2 layers: superficial columnar and deep cuboidal.
- Palpebral conjunctiva (orbital component): a transition zone between tarsal conjunctiva and forniceal conjunctiva, with an increase in loose submucosal tissue and containing a large number of mucosa-associated lymphoid tissue.
- Forniceal conjunctiva: a very loose tissue forming a pocket, with 3 layers of stratified squamous epithelium and containing a high number of goblet cells.
- Bulbar conjunctiva: the thinnest stroma of all conjunctiva, almost transparent, with 3 layers of stratified epithelium and loosely attached to the sclera.
- Limbus: the junction between conjunctiva and cornea, fusing with corneal epithelium, with ~10 layers of squamous epithelium and containing a capillary network that feeds the avascular cornea.
Specialized Cells in the Conjunctiva
- Goblet cells: secrete mucin.
- Langerhans cells: immune cells, with high density in tarsal, forniceal, and bulbar conjunctiva.
Blood Supply to the Conjunctiva
- The conjunctiva has 2 different sources of blood supply: palpebral arcades and conjunctival arteries.
- Palpebral arcades: supply most of the conjunctiva, with 2 arcades: marginal tarsal arcades and peripheral tarsal arcades.
- Conjunctival arteries: branch of the anterior ciliary artery, supplying the bulbar conjunctiva in the limbal area.
Clinical Relevance
- Conjunctival inflammation: engorged superficial vessels, bulbar conjunctiva hyperaemic, and characteristic ciliary flush (perilimbal injection).
- Subconjunctival haemorrhage (ecchymosis): caused by multiple blood vessels within the conjunctiva, bleeding between the conjunctiva and sclera.
Venous Drainage
- Palpebral and forniceal conjunctiva: veins from the conjunctiva drain into the venous plexus of the eyelids, then into the superior/inferior ophthalmic veins, and finally into the cavernous sinus.
- Bulbar conjunctiva: veins from the bulbar conjunctiva drain into the circumcorneal zone of veins, then into the anterior ciliary veins, ophthalmic veins, and finally into the cavernous sinus.
Conjunctival Lymph Drainage
- Lymph drains laterally to the superficial parotid nodes and medially to the submandibular nodes.
Conjunctival Sensory Innervation
- Bulbar conjunctiva: innervated by long ciliary nerves.
- Superior palpebral and forniceal conjunctiva: innervated by the frontal and lacrimal branches of the ophthalmic division of the trigeminal nerve.
- Inferior palpebral and forniceal conjunctiva: innervated by the lacrimal branch of the ophthalmic division and the infraorbital branch of the maxillary division.
Structure of the Conjunctiva
- The conjunctiva consists of 2 layers: epithelium and stroma.
- Epithelium: 2-7 cell layers thick, depending on location, and contains goblet cells.
- Stroma: a connective tissue layer beneath the epithelium, housing blood vessels, nerves, and specialized cells.
Types of Conjunctiva
- Marginal conjunctiva: a transition zone from skin to conjunctiva, consisting of 5-7 layers of non-keratinized stratified squamous epithelium.
- Palpebral conjunctiva: firmly attached to the inner surface of eyelids, consisting of 2 layers: superficial columnar and deep cuboidal.
- Palpebral conjunctiva (orbital component): a transition zone between tarsal conjunctiva and forniceal conjunctiva, with an increase in loose submucosal tissue and containing a large number of mucosa-associated lymphoid tissue.
- Forniceal conjunctiva: a very loose tissue forming a pocket, with 3 layers of stratified squamous epithelium and containing a high number of goblet cells.
- Bulbar conjunctiva: the thinnest stroma of all conjunctiva, almost transparent, with 3 layers of stratified epithelium and loosely attached to the sclera.
- Limbus: the junction between conjunctiva and cornea, fusing with corneal epithelium, with ~10 layers of squamous epithelium and containing a capillary network that feeds the avascular cornea.
Specialized Cells in the Conjunctiva
- Goblet cells: secrete mucin.
- Langerhans cells: immune cells, with high density in tarsal, forniceal, and bulbar conjunctiva.
Blood Supply to the Conjunctiva
- The conjunctiva has 2 different sources of blood supply: palpebral arcades and conjunctival arteries.
- Palpebral arcades: supply most of the conjunctiva, with 2 arcades: marginal tarsal arcades and peripheral tarsal arcades.
- Conjunctival arteries: branch of the anterior ciliary artery, supplying the bulbar conjunctiva in the limbal area.
Clinical Relevance
- Conjunctival inflammation: engorged superficial vessels, bulbar conjunctiva hyperaemic, and characteristic ciliary flush (perilimbal injection).
- Subconjunctival haemorrhage (ecchymosis): caused by multiple blood vessels within the conjunctiva, bleeding between the conjunctiva and sclera.
Venous Drainage
- Palpebral and forniceal conjunctiva: veins from the conjunctiva drain into the venous plexus of the eyelids, then into the superior/inferior ophthalmic veins, and finally into the cavernous sinus.
- Bulbar conjunctiva: veins from the bulbar conjunctiva drain into the circumcorneal zone of veins, then into the anterior ciliary veins, ophthalmic veins, and finally into the cavernous sinus.
Conjunctival Lymph Drainage
- Lymph drains laterally to the superficial parotid nodes and medially to the submandibular nodes.
Conjunctival Sensory Innervation
- Bulbar conjunctiva: innervated by long ciliary nerves.
- Superior palpebral and forniceal conjunctiva: innervated by the frontal and lacrimal branches of the ophthalmic division of the trigeminal nerve.
- Inferior palpebral and forniceal conjunctiva: innervated by the lacrimal branch of the ophthalmic division and the infraorbital branch of the maxillary division.
Sclera
- Whish outer coat of the eye
- Derived from Greek "skleros" meaning hard
- Dense, irregular connective tissue (CT)
Functions of Sclera
- Protection: tough barrier separating intraocular structures from orbital walls and the outside world
- Refractive stability: keeps eye length stable during changes in intraocular pressure and blood pressure, and during eye movements and accommodation
- Conduit for nerves and vessels: allows nerve and vessel access to underlying ocular structures
- Anchor for extraocular muscles: provides stable anchorage for extraocular muscle tendons, contributing to stability of torsional movements
- Anchor for ciliary muscle: opposes contractile forces of ciliary muscle, allowing stable accommodation
- Facilitates ocular drainage: majority of aqueous outflow through intrascleral venous plexus to the episcleral plexus
Openings in the Sclera
- Minor foramina: allow blood vessels and nerves to pierce the eyeball
- Two major foramina: anterior scleral foramen (cornea) and posterior scleral foramen (scleral canal)
Layers of the Sclera
- Episclera: outermost layer, merges with the underlying scleral stroma
- Scleral stroma: dense, irregular CT
- Lamina fusca: innermost layer, regarded as part of choroid by some, but separated from choroid by perichoroidal space
Biochemical Composition of the Sclera
- Collagen (around 90% of scleral dry weight, predominantly type I)
- Proteoglycans and glycosaminoglycans (around 1% of dry weight)
- Glycoproteins (e.g. fibronectin)
- Fibroblasts, myofibroblasts, and some melanocytes
- Non-collagenous proteins (e.g. elastin, proteases, etc.)
- Water
Scleral Cells
- Fibroblasts: synthesise collagen, elastic, and reticular fibres, reside close to collagen matrices
- Myofibroblasts: modified fibroblasts, synthesise collagen, express contractile proteins (e.g. α-smooth muscle actin), present in mammals, including humans
Scleral Collagens
- Structural unit: tropocollagen/collagen (~3 intertwined polypeptide chains, rich in amino acids proline and hydroxyproline)
- Staggered collagen molecules assemble into a fibril
Scleral Proteoglycans
- ~0.7-0.9% of the total scleral dry weight
- Modulate collagen fibril assembly and arrangement
- Aggrecan, biglycan, and decorin: sequester water within the scleral ECM, highest concentration in the posterior sclera, possibly maintaining posterior pole flexibility
Learn about the structure and function of the iris, including its size, zones, and muscles. Discover how it relates to the pupil and the eye's anatomy.
Make Your Own Quizzes and Flashcards
Convert your notes into interactive study material.
Get started for free