Podcast
Questions and Answers
What condition results from a decrease in respiratory rate and leads to an increase in PCO2 in the blood?
What condition results from a decrease in respiratory rate and leads to an increase in PCO2 in the blood?
- Respiratory Acidosis (correct)
- Metabolic Acidosis
- Respiratory Alkalosis
- Metabolic Alkalosis
Which compensatory mechanism do the kidneys employ in response to respiratory acidosis?
Which compensatory mechanism do the kidneys employ in response to respiratory acidosis?
- Decreasing blood volume to lower CO2 levels
- Increasing urine output of CO2
- Secreting more HCO3- and reabsorbing H+ ions
- Reabsorbing HCO3- and excreting more H+ ions (correct)
What effect does hyperventilation have on PCO2 and H+ ion concentration in the blood?
What effect does hyperventilation have on PCO2 and H+ ion concentration in the blood?
- Increases both PCO2 and H+ concentration
- Decreases PCO2 and increases H+ concentration
- Increases PCO2 and decreases H+ concentration
- Decreases both PCO2 and H+ concentration (correct)
Which of the following conditions can lead to respiratory alkalosis?
Which of the following conditions can lead to respiratory alkalosis?
What is a potential consequence of prolonged respiratory alkalosis if not effectively treated?
What is a potential consequence of prolonged respiratory alkalosis if not effectively treated?
What condition is indicated by a decrease in blood pH?
What condition is indicated by a decrease in blood pH?
In which situation would peripheral vein sampling most likely result in misleading acid-base status?
In which situation would peripheral vein sampling most likely result in misleading acid-base status?
What does a Base Excess/Deficit (BE) of -4.8 indicate?
What does a Base Excess/Deficit (BE) of -4.8 indicate?
What is the primary disturbance in the case of a blood gas result showing a pH of 7.48, PaCO2 of 25.9 mmHg, and HCO3 of 18.8 mEq/L?
What is the primary disturbance in the case of a blood gas result showing a pH of 7.48, PaCO2 of 25.9 mmHg, and HCO3 of 18.8 mEq/L?
Which statement accurately describes compensation for acid-base status changes?
Which statement accurately describes compensation for acid-base status changes?
What is assessed first when interpreting blood gas results?
What is assessed first when interpreting blood gas results?
What does the ROME acronym stand for in blood gas analysis?
What does the ROME acronym stand for in blood gas analysis?
If a blood gas sample is exposed to air, what is likely to be affected?
If a blood gas sample is exposed to air, what is likely to be affected?
Which condition is associated with a primary gain in acid or a loss of base?
Which condition is associated with a primary gain in acid or a loss of base?
What is a direct consequence of renal compensation in metabolic alkalosis?
What is a direct consequence of renal compensation in metabolic alkalosis?
What causes respiratory acidosis?
What causes respiratory acidosis?
Which of the following is a possible cause of metabolic alkalosis?
Which of the following is a possible cause of metabolic alkalosis?
What physiological response occurs during respiratory compensation for metabolic alkalosis?
What physiological response occurs during respiratory compensation for metabolic alkalosis?
Which values are critical for assessing a patient’s acid-base status?
Which values are critical for assessing a patient’s acid-base status?
Which of the following statements about metabolic acidosis is correct?
Which of the following statements about metabolic acidosis is correct?
What does a high PaCO2 level indicate?
What does a high PaCO2 level indicate?
Which condition is primarily caused by an increase in ventilation that exceeds CO2 production?
Which condition is primarily caused by an increase in ventilation that exceeds CO2 production?
Which of the following contributes to metabolic acidosis through a loss of bicarbonate?
Which of the following contributes to metabolic acidosis through a loss of bicarbonate?
What causes Metabolic Acidosis?
What causes Metabolic Acidosis?
How does the body typically respond to Metabolic Acidosis?
How does the body typically respond to Metabolic Acidosis?
What defines Metabolic Alkalosis?
What defines Metabolic Alkalosis?
Which of the following conditions is NOT a potential cause of Metabolic Alkalosis?
Which of the following conditions is NOT a potential cause of Metabolic Alkalosis?
What is a hallmark of Respiratory Acidosis?
What is a hallmark of Respiratory Acidosis?
What condition develops more gradually in response to hypoxemia?
What condition develops more gradually in response to hypoxemia?
When is rebreathing CO2 typically employed as a treatment?
When is rebreathing CO2 typically employed as a treatment?
What is a common cause of bicarbonate retention in Metabolic Alkalosis?
What is a common cause of bicarbonate retention in Metabolic Alkalosis?
Which condition is characterized by a decrease in HCO3- levels without respiratory contribution?
Which condition is characterized by a decrease in HCO3- levels without respiratory contribution?
Which metabolic disturbance is most likely to occur after significant fluid loss due to diarrhea?
Which metabolic disturbance is most likely to occur after significant fluid loss due to diarrhea?
Flashcards
PVCO2 Measurement
PVCO2 Measurement
Measurement of partial pressure of carbon dioxide in venous blood, reflecting the patient's ventilation ability.
Base Excess/Deficit (BE)
Base Excess/Deficit (BE)
Calculated value estimating the base needed to achieve a normal pH at a standard temperature.
Acidemia
Acidemia
Lowering of blood pH.
Alkalemia
Alkalemia
Signup and view all the flashcards
ROME
ROME
Signup and view all the flashcards
Blood Gas Interpretation Steps (1)
Blood Gas Interpretation Steps (1)
Signup and view all the flashcards
Blood Gas Interpretation Steps (2)
Blood Gas Interpretation Steps (2)
Signup and view all the flashcards
Blood Gas Interpretation Steps (3)
Blood Gas Interpretation Steps (3)
Signup and view all the flashcards
Metabolic Acidosis
Metabolic Acidosis
Signup and view all the flashcards
Metabolic Alkalosis
Metabolic Alkalosis
Signup and view all the flashcards
Respiratory Acidosis
Respiratory Acidosis
Signup and view all the flashcards
Respiratory Alkalosis
Respiratory Alkalosis
Signup and view all the flashcards
PaO2
PaO2
Signup and view all the flashcards
PaCO2
PaCO2
Signup and view all the flashcards
Renal Compensation
Renal Compensation
Signup and view all the flashcards
DKA
DKA
Signup and view all the flashcards
Starvation
Starvation
Signup and view all the flashcards
Lactic Acidosis
Lactic Acidosis
Signup and view all the flashcards
Hypercapnia
Hypercapnia
Signup and view all the flashcards
Hypocapnia
Hypocapnia
Signup and view all the flashcards
Compensation (kidney)
Compensation (kidney)
Signup and view all the flashcards
Causes of Metabolic Acidosis
Causes of Metabolic Acidosis
Signup and view all the flashcards
Causes of Metabolic Alkalosis
Causes of Metabolic Alkalosis
Signup and view all the flashcards
Respiratory Compensation
Respiratory Compensation
Signup and view all the flashcards
Alkalosis Causes
Alkalosis Causes
Signup and view all the flashcards
Alkalosis Treatment
Alkalosis Treatment
Signup and view all the flashcards
Hyperventilation
Hyperventilation
Signup and view all the flashcards
HCO3-
HCO3-
Signup and view all the flashcards
Study Notes
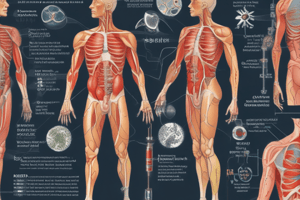
Acid-Base Balance
- Refers to the steady state of the pH of the body
- Normal metabolic processes continually generate acids
- Normal pH range is 7.35 to 7.45
- If pH falls out of this range, proteins are diminished or destroyed
- Below 7.3 = acidosis (excess H+) = causes acidemia
- Above 7.4 = alkalosis (low H+) = causes alkalemia
Importance of pH
- Normal blood pH is between 7.35 and 7.45
- Blood pH below 7.35 is known as acidemia
- Blood pH above 7.45 is known as alkalemia
- Values less than 6.8 or greater than 7.8 often result in death
- The body's pH influences the function of enzymes, speed of cellular reactions, cell permeability, and the integrity of cell structure
Effects of pH Changes on the Body
- Effect of Acidosis
- ↓ blood pH (acidemia)
- Depression of the CNS - disoriented/comatose
- Effect of Alkalosis
- ↑ blood pH (alkaemia)
- Hyperexcitability of the nervous system - able to generate impulses without normal stimuli
- Spasms/tetanic contractions
- Death with severe alkalemia is due to spasms of muscles of respiration
Regulatory Systems for Acid-Base Balance
- Chemical buffers
- 1st line of defense
- React in seconds
- 3 main systems: bicarbonate, protein, phosphate
- Respiratory system (lungs)
- 2nd line of defense
- React in minutes
- Renal system (kidneys)
- 3rd line of defense
- React in hours to days
- Most powerful and lasts the longest
Chemical Buffers: Review
- Acid
- Substance that gives up/donates a proton (hydrogen ion, H⁺)
- Base
- Substance that accepts/binds a proton (hydrogen ion, H⁺)
- Buffer
- Compound that can accept or donate a proton (H⁺)
- Buffers are usually weak acids with their corresponding salts.
Chemical Buffer Systems
- Work to counteract H⁺ imbalance created by metabolic processes
- Buffers
- Substances that alter the H⁺ concentration
- If H⁺ are added, the buffer combines with the extra H⁺ ions to help maintain the pH
- If H⁺ are lost, the buffer releases H⁺ ions to combine with the base to help maintain the pH
- Work both intracellularly and extracellularly
- 3 main systems
- Bicarbonate Buffer
- Protein Buffer
- Phosphate Buffer
Bicarbonate (HCO₃⁻) Buffer
- Remember: CO₂ is produced as a waste product during aerobic cellular respiration
- CO₂ combines with H₂O to form carbonic acid (H₂CO₃)
- Most of which rapidly dissociates to form H⁺ and bicarbonate (HCO₃⁻)
- CO₂ acts like an acid because it combines with water to form carbonic acid
- H⁺ acts as an acid, and HCO₃⁻ acts as a base
- Any disturbance of the system will be compensated by a shift in the chemical equilibrium by the law of mass action.
Importance of Blood Gases
- Allow for assessment of patient's oxygenation, ventilation, and acid-base status
- BG, electrolytes, iCa²⁺, and lactate levels
- Can help in diagnosis, monitoring, and treatment of disease processes directly related to metabolic or respiratory dysfunction
4 Basic Types of Acid-Base Disturbances
- Metabolic acidosis
- Primary gain in acid or loss of base
- Metabolic alkalosis
- Primary gain in base or loss of acid
- Respiratory acidosis
- Retention of CO₂ due to CO₂ production outpacing alveolar ventilation
- Respiratory alkalosis
- Removal of CO₂ by ventilation which outpaces CO₂ production
Clarification of Terms
- PaO₂
- Partial pressure of oxygen dissolved in arterial blood.
- A measure of oxygenation not ventilation
- PaCO₂
- Partial pressure of carbon dioxide dissolved in arterial blood.
- Provided the best measurement of patients ability to ventilate
- Determines whether resp. acidosis or resp. alkalosis is present.
- PCO₂
- Partial pressure of carbon dioxide dissolved in venous blood.
- When obtained properly it is a measure of the patients ability to ventilate.
- Base Excess/Deficit (BE)
- Calculated value that estimates how much base needs to be added/subtracted to achieve a normal pH @ a normal temperature
- Reflects the metabolic portion of acid balance
- Evaluates for metabolic acidosis or alkalosis
Potential Sampling Errors
- Peripheral vein sampling in patients with poor perfusion
- Sample may reflect acid-base status of limb and not of whole body
- Prolonged occlusion of sampled limb vein
- Sample may reflect lactic acidosis specific only to that limb
- Sample not immediately evaluated or placed on ice
- Continued cellular metabolism by RBCs will continue to use O₂ and produce CO₂
- Exposing sample to air
- Oxygen from atmosphere will diffuse into sample and CO₂ will diffuse out altering PaO₂, PaCO₂, and pH
- Thus causing error in calculated values (HCO₃ & BE)
The Four Primary Acid-Base Disorders and Their Compensatory Changes
- Conditions / Primary Disorder / Compensation
- ↓pH and ↓HCO₃ (↓BEecf) / Metabolic acidosis/ ↓PCO₂
- ↑pH and ↑HCO3 (↑BEecf) / Metabolic alkalosis/ ↑PCO₂
- ↓pH and ↑Pco₂ / Respiratory acidosis/ ↑HCO₃ (↑BEecf)
- ↑pH and ↓Pco₂ / Respiratory alkalosis/ ↓HCO₃ (↓BEecf)
Steps in Interpreting Blood Gas Results
- Venous or Arterial Sample?
- Is there an acidemia or alkalemia present?
- Acidemia = decrease in blood pH
- Alkalemia = increase in blood pH
- Determine Primary Disturbance
- ROME
- Respiratory Opposite
- Metabolic Equal
- ROME
Steps in Interpreting Blood Gas Results Continued
- Assess Oxygenation if arterial sample
- F₁O₂ of room air is 21%
- PaO₂ - should equal 5x F₁O₂
- Determine if compensatory changes have occurred
- A change in the resp. or metabolic component of the acid-base status normally induces an opposite compensatory response in effort to normalize pH.
- Absence or degree of compensation can provide some insight into chronicity of the disturbance.
- Overcompensation does not occur.
Case Studies (Examples)
Example 1
- pH: 7.22
- PaCO₂: 65 mm Hg
- PaO₂: 45 mm Hg
- HCO₃⁻: 26 mEq/L
- BE(ecf): +4 mEq/L
Example 2
- pH: 7.48
- PaO₂: 63 mmHg
- PaCO₂: 25.9 mmHg
- HCO₃⁻: 18.8 mEq/L
- BE: -4.8
###Metabolic Acidosis
- Rise in H⁺ due to either an increase in production or a decrease in excretion
- Starvation
- DKA; Lactic acidosis; Depletion of HCO3- reserve either due to decreased resorption or excess loss
- Renal failure
- Diarrhea
###Metabolic Alkalosis
- Caused by a decrease or loss of metabolic acids or an increase in bicarbonate concentration not due to respiratory problems
- Loss of H⁺ (vomiting)
- Gain of HCO₃⁻ (abnormal retention of HCO₃⁻ by kidneys in response to dehydration due to vomiting/gastric retention of fluids)
- Excessive ingestion of antacids (increase in -HCO₃⁻)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
This quiz explores the critical concepts surrounding acid-base balance in the human body. You will learn about the importance of pH levels, what defines acidemia and alkalemia, and the effects of pH changes on bodily functions, including the nervous system and overall health. Test your understanding of these essential physiological processes.