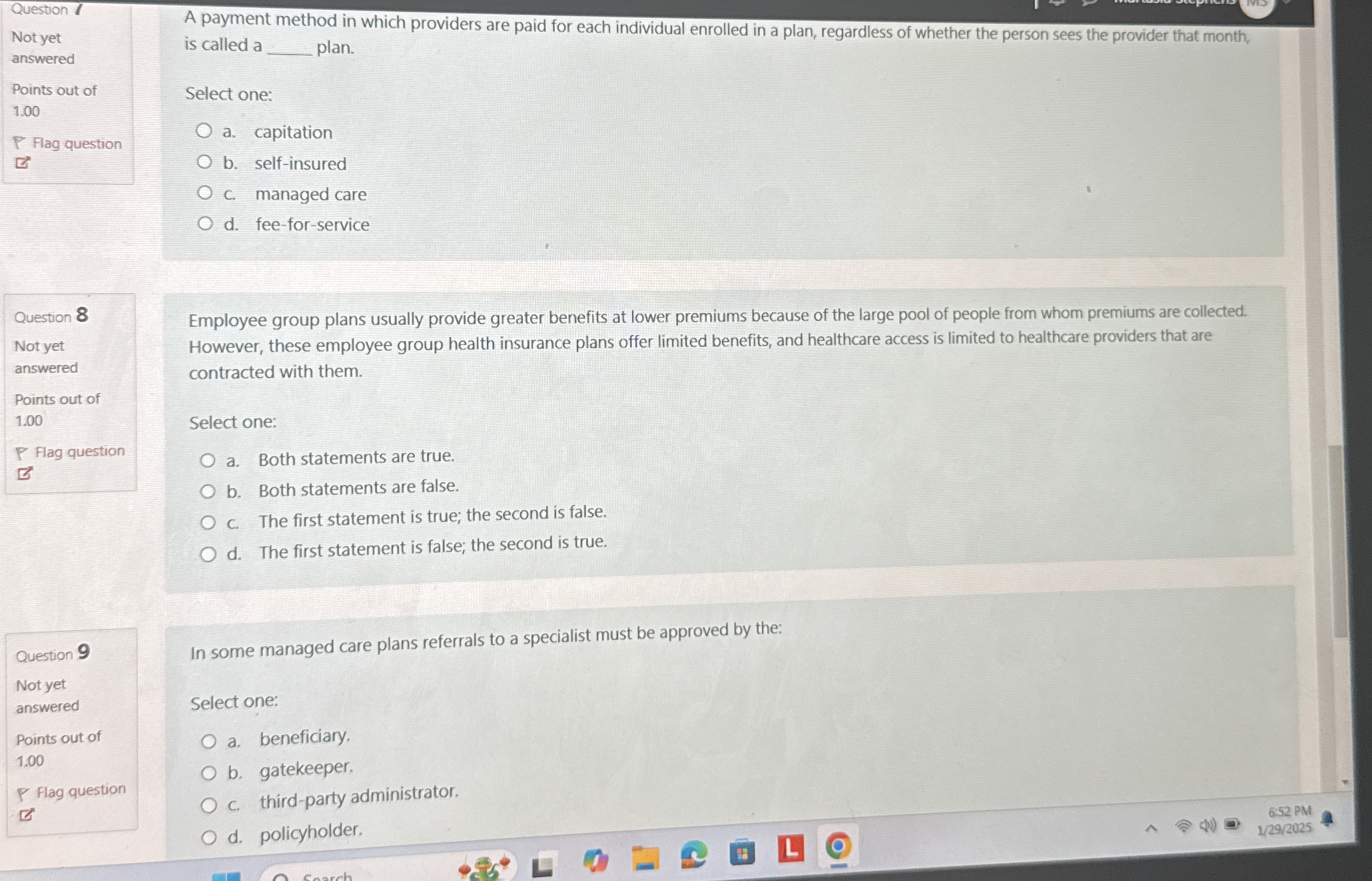
A payment method in which providers are paid for each individual enrolled in a plan, regardless of whether the person sees the provider that month, is called a __ plan? Employee gr... A payment method in which providers are paid for each individual enrolled in a plan, regardless of whether the person sees the provider that month, is called a __ plan? Employee group plans usually provide greater benefits at lower premiums because of the large pool of people from whom premiums are collected. However, these employee group health insurance plans offer limited benefits, and healthcare access is limited to healthcare providers that are contracted with them. In some managed care plans, referrals to a specialist must be approved by the:
Understand the Problem
The questions are related to health insurance plans and their characteristics. The first question asks for the type of payment method used for health services. The second question requires evaluating statements about employee group plans, and the third question inquires about who must approve referrals in managed care plans.
Answer
Capitation plan, true, gatekeeper.
The final answer is capitation plan, both statements are true, and gatekeeper.
Answer for screen readers
The final answer is capitation plan, both statements are true, and gatekeeper.
More Information
A capitation plan involves paying providers a set fee per patient regardless of actual visits. Employee group plans typically offer greater benefits due to economies of scale. In managed care, a gatekeeper often approves specialist referrals.
Tips
Confusing capitation with fee-for-service, which pays per visit. Misunderstanding employee group plans benefits and costs.
Sources
AI-generated content may contain errors. Please verify critical information