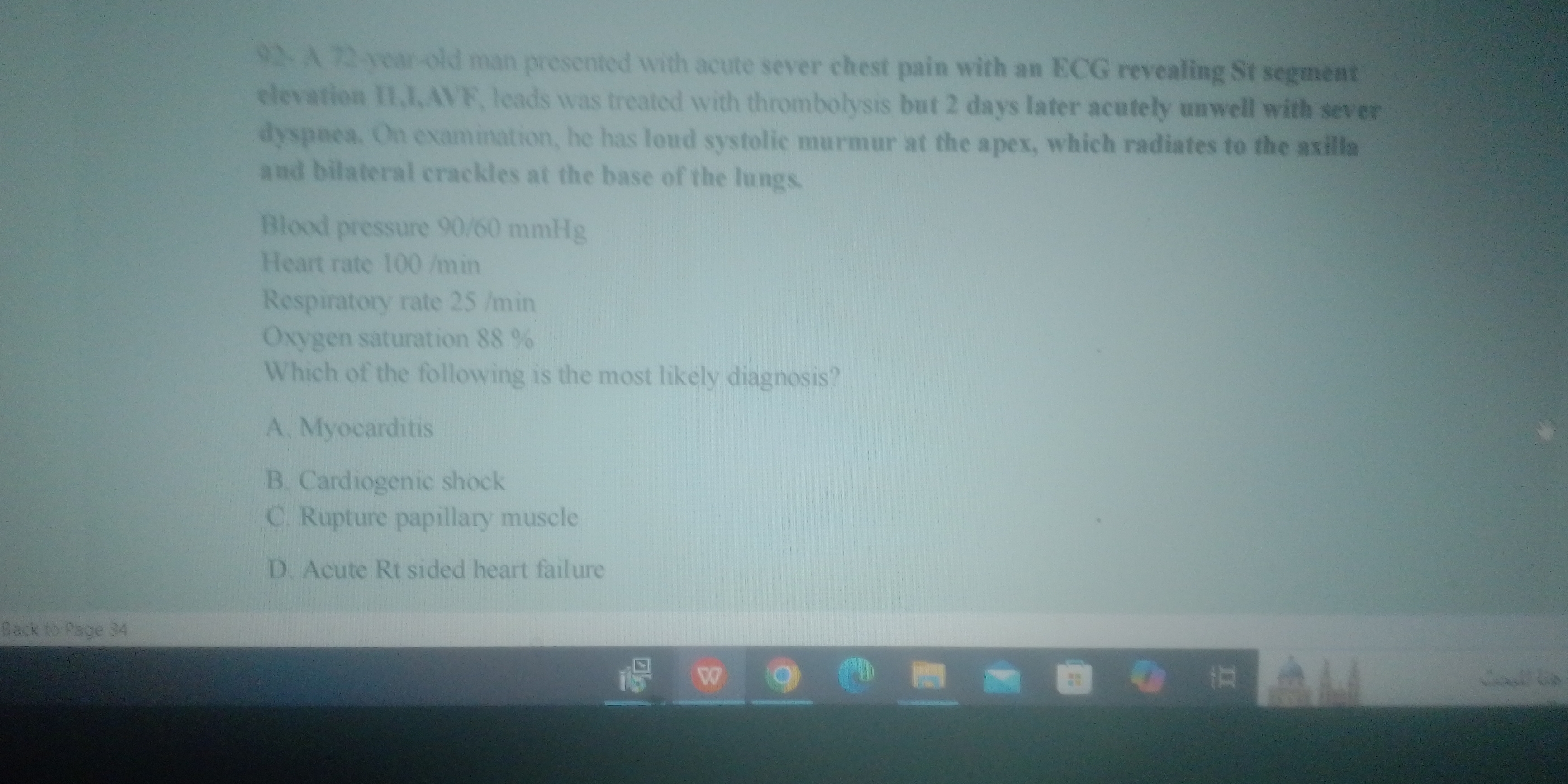
A 75 year old man presented with acute severe chest pain with an ECG revealing St segment elevation II, AVF; leads was treated with thrombolysis but 2 days later acutely unwell wit... A 75 year old man presented with acute severe chest pain with an ECG revealing St segment elevation II, AVF; leads was treated with thrombolysis but 2 days later acutely unwell with sever dyspnea. On examination, he has loud systolic murmur at the apex, which radiates to the axilla. Blood pressure 90/60 mmHg, Heart rate 100/min, Respiratory rate 25/min, Oxygen saturation 88%. Which of the following is the most likely diagnosis? A. Myocarditis B. Cardiogenic shock C. Rupture papillary muscle D. Acute Rt sided heart failure
Understand the Problem
The question is presenting a clinical scenario involving a 75-year-old man with specific symptoms and asking for the most likely diagnosis based on the provided clinical details.
Answer
Rupture papillary muscle
The final answer is C. Rupture papillary muscle
Answer for screen readers
The final answer is C. Rupture papillary muscle
More Information
The loud systolic murmur radiating to the axilla and the hemodynamic instability are classic indicators of papillary muscle rupture, especially after an inferior myocardial infarction.
Tips
A common mistake is not considering the timing of new symptoms post-MI, which can indicate mechanical complications like papillary muscle rupture.
Sources
- ST-Segment Elevation Myocardial Infarction (STEMI) - empendium.com
- Acute Myocardial Infarction (MI) - Cardiovascular Disorders - merckmanuals.com
AI-generated content may contain errors. Please verify critical information