Podcast
Questions and Answers
How is a ''wound'' best defined in the context of tissue injury?
How is a ''wound'' best defined in the context of tissue injury?
- An involuntary contraction of muscle tissue.
- A disruption of normal anatomic relationships resulting from an injurious process. (correct)
- A psychological response to physical trauma.
- A superficial abrasion that does not penetrate the dermis.
What is the initial phase of wound healing primarily focused on?
What is the initial phase of wound healing primarily focused on?
- Hemostasis (correct)
- Collagen synthesis
- Granulation tissue formation
- Epithelialization
Which of the following is a cardinal sign of inflammation?
Which of the following is a cardinal sign of inflammation?
- Pallor
- Rubor (redness) (correct)
- Jaundice
- Cyanosis
What is the primary role of Platelet-Derived Growth Factor (PDGF) in wound healing?
What is the primary role of Platelet-Derived Growth Factor (PDGF) in wound healing?
Which process is associated with the release of arachidonic acid (AA) and its derivatives during inflammation?
Which process is associated with the release of arachidonic acid (AA) and its derivatives during inflammation?
During which phase of wound healing do leukocytes begin to stick to vessel walls and migrate towards the injury site?
During which phase of wound healing do leukocytes begin to stick to vessel walls and migrate towards the injury site?
What is the main characteristic of the substrate phase of wound healing?
What is the main characteristic of the substrate phase of wound healing?
What role do macrophages play during the substrate phase of wound healing?
What role do macrophages play during the substrate phase of wound healing?
Which cell type is primarily responsible for collagen production in the proliferative phase of wound healing?
Which cell type is primarily responsible for collagen production in the proliferative phase of wound healing?
During the proliferative phase of wound healing, what process describes the production of amino acid chains?
During the proliferative phase of wound healing, what process describes the production of amino acid chains?
What characterizes the maturation phase of wound healing?
What characterizes the maturation phase of wound healing?
What is the predominant activity during the maturation phase of wound healing?
What is the predominant activity during the maturation phase of wound healing?
What is the primary mechanism of wound closure in secondary healing?
What is the primary mechanism of wound closure in secondary healing?
What generates the centripetal force that characterizes wound contraction in secondary healing?
What generates the centripetal force that characterizes wound contraction in secondary healing?
What is a key characteristic of tertiary wound healing?
What is a key characteristic of tertiary wound healing?
What is most important when deciding to perform delayed closure in tertiary wound healing?
What is most important when deciding to perform delayed closure in tertiary wound healing?
In assessing the goal of wound closure, what is considered most important?
In assessing the goal of wound closure, what is considered most important?
How does the amount of tissue trauma affect wound healing?
How does the amount of tissue trauma affect wound healing?
Why is a hematoma detrimental to wound healing?
Why is a hematoma detrimental to wound healing?
How does bacterial contamination generally affect wound closure?
How does bacterial contamination generally affect wound closure?
What level of bacterial contamination can a wound typically tolerate without developing a clinical infection?
What level of bacterial contamination can a wound typically tolerate without developing a clinical infection?
Which specific bacteria, regardless of quantity, is a contraindication for wound closure?
Which specific bacteria, regardless of quantity, is a contraindication for wound closure?
What is the most effective strategy for tetanus prophylaxis in wound management?
What is the most effective strategy for tetanus prophylaxis in wound management?
What is the primary function of wound dressings?
What is the primary function of wound dressings?
During the proliferative phase of primary wound healing, what approximate timeframe does collagen production begin after wounding?
During the proliferative phase of primary wound healing, what approximate timeframe does collagen production begin after wounding?
What is the term for the sign of inflammation identified by heat?
What is the term for the sign of inflammation identified by heat?
Around how long does a maturation process require to take place in an adult?
Around how long does a maturation process require to take place in an adult?
Which stage of wound healing may also be divided by the terms inflammatory, lag phase, or exudative phase?
Which stage of wound healing may also be divided by the terms inflammatory, lag phase, or exudative phase?
Following a wounding, how long do PMNs remain the predominant cell?
Following a wounding, how long do PMNs remain the predominant cell?
Following a wound, how long does it take Monocytes enter the wound and reach maximum numbers?
Following a wound, how long does it take Monocytes enter the wound and reach maximum numbers?
The degradation of AA into which derivatives elicits a number of responses associated with the inflammatory response?
The degradation of AA into which derivatives elicits a number of responses associated with the inflammatory response?
Closure of a wound by active means after a delay of days to weeks is what type of wound healing?
Closure of a wound by active means after a delay of days to weeks is what type of wound healing?
A laceration with a knife is damaging mostly to which area?
A laceration with a knife is damaging mostly to which area?
Why are the phases of proliferation and maturation of the wound healing process divided into categories?
Why are the phases of proliferation and maturation of the wound healing process divided into categories?
In primary healing, how is the wound closed?
In primary healing, how is the wound closed?
The substrate phase of wound healing can also be called the exudative phase. Main cells involved that process are PMN, which stands for what?
The substrate phase of wound healing can also be called the exudative phase. Main cells involved that process are PMN, which stands for what?
When collagen is not a consist event, what phase demonstrates a rapid spurt after it begins?
When collagen is not a consist event, what phase demonstrates a rapid spurt after it begins?
At the same time that biochemical events are developing in the wounds process, also venules and what else are being affected?
At the same time that biochemical events are developing in the wounds process, also venules and what else are being affected?
In the middle of an open wound that is healing by secondary intention, what phase continues unabated?
In the middle of an open wound that is healing by secondary intention, what phase continues unabated?
In order, list the first two names of the wound healing processes:
In order, list the first two names of the wound healing processes:
According to the presentation, what contributes to loss of function during inflammation
According to the presentation, what contributes to loss of function during inflammation
What characterizes the nature of biochemical and physiologic processes in wound healing, regardless of the cause of injury?
What characterizes the nature of biochemical and physiologic processes in wound healing, regardless of the cause of injury?
How are the three distinct types of wound healing classified?
How are the three distinct types of wound healing classified?
Which of the following represents an alternate name for the substrate phase of wound healing?
Which of the following represents an alternate name for the substrate phase of wound healing?
What is the primary purpose of hemostasis in the context of wound healing?
What is the primary purpose of hemostasis in the context of wound healing?
What triggers the activation of chemoattractants and mitogens during the biochemical aspect of wound healing?
What triggers the activation of chemoattractants and mitogens during the biochemical aspect of wound healing?
What role does platelet-derived growth factor (PDGF) play in wound healing?
What role does platelet-derived growth factor (PDGF) play in wound healing?
How does the degradation of arachidonic acid (AA) contribute to the inflammatory response during wound healing?
How does the degradation of arachidonic acid (AA) contribute to the inflammatory response during wound healing?
What cellular activity characterizes the physiologic events occurring alongside biochemical changes in wound healing?
What cellular activity characterizes the physiologic events occurring alongside biochemical changes in wound healing?
Which cells are predominant during the initial phase (approximately 48 hours) of the substrate phase of wound healing?
Which cells are predominant during the initial phase (approximately 48 hours) of the substrate phase of wound healing?
What is the role of macrophages that evolve from monocytes in the substrate phase of wound healing?
What is the role of macrophages that evolve from monocytes in the substrate phase of wound healing?
What substances do macrophages secrete to stimulate fibroblast replication and angiogenesis during the substrate phase?
What substances do macrophages secrete to stimulate fibroblast replication and angiogenesis during the substrate phase?
How does the duration of the substrate phase differ between primary and secondary wound healing?
How does the duration of the substrate phase differ between primary and secondary wound healing?
Which characteristic defines the appearance of a wound during the proliferative phase?
Which characteristic defines the appearance of a wound during the proliferative phase?
What cell type is primarily responsible for collagen production during the proliferative phase?
What cell type is primarily responsible for collagen production during the proliferative phase?
What is the initial biochemical event that begins the process of collagen synthesis within fibroblasts during the proliferative phase?
What is the initial biochemical event that begins the process of collagen synthesis within fibroblasts during the proliferative phase?
How does collagen production change over time during the proliferative phase in a primary wound?
How does collagen production change over time during the proliferative phase in a primary wound?
What physiological change primarily characterizes the maturation phase of wound healing?
What physiological change primarily characterizes the maturation phase of wound healing?
During the maturation phase, what change is typically observed in the appearance of the wound scar?
During the maturation phase, what change is typically observed in the appearance of the wound scar?
What is a key characteristic of the metabolic activity during the maturation phase of wound healing?
What is a key characteristic of the metabolic activity during the maturation phase of wound healing?
Approximately how long does the maturation process of wound healing typically take in adults?
Approximately how long does the maturation process of wound healing typically take in adults?
Why are the proliferative and maturation phases divided into categories?
Why are the proliferative and maturation phases divided into categories?
What is the hallmark of primary wound healing?
What is the hallmark of primary wound healing?
How is secondary wound healing characterized?
How is secondary wound healing characterized?
What force primarily drives wound contraction in secondary healing?
What force primarily drives wound contraction in secondary healing?
What is a potential undesirable outcome associated with wound contraction in secondary healing?
What is a potential undesirable outcome associated with wound contraction in secondary healing?
In the context of secondary wound healing, what constitutes 'proud flesh'?
In the context of secondary wound healing, what constitutes 'proud flesh'?
What characterizes tertiary wound healing?
What characterizes tertiary wound healing?
What is a primary consideration before performing delayed closure in tertiary wound healing?
What is a primary consideration before performing delayed closure in tertiary wound healing?
What is the overarching goal in all wound closures?
What is the overarching goal in all wound closures?
How does the amount of tissue trauma typically affect wound healing?
How does the amount of tissue trauma typically affect wound healing?
How does a hematoma impede wound healing?
How does a hematoma impede wound healing?
What is the general effect of bacterial contamination on wound closure?
What is the general effect of bacterial contamination on wound closure?
What approach is considered the most important for preventing tetanus in wound management?
What approach is considered the most important for preventing tetanus in wound management?
Flashcards
What is a wound?
What is a wound?
A disruption of normal anatomic relationships as the result of an injurious process, either intentional or accidental.
Distinct Wound Types
Distinct Wound Types
Primary, secondary, and tertiary, based on the timing of epithelium replacement.
Wound Healing Stages
Wound Healing Stages
Hemorrhagic, substrate, proliferative, and remodeling phases.
Hemorrhagic Phase
Hemorrhagic Phase
Signup and view all the flashcards
Signs of Inflammation
Signs of Inflammation
Signup and view all the flashcards
Trauma's Cascade Effect
Trauma's Cascade Effect
Signup and view all the flashcards
Platelet-Derived Growth Factor (PDGF)
Platelet-Derived Growth Factor (PDGF)
Signup and view all the flashcards
Substrate Phase
Substrate Phase
Signup and view all the flashcards
Macrophages Role
Macrophages Role
Signup and view all the flashcards
Proliferative Phase
Proliferative Phase
Signup and view all the flashcards
Collagen
Collagen
Signup and view all the flashcards
Maturation or Remodeling Phase
Maturation or Remodeling Phase
Signup and view all the flashcards
Primary Wound Healing
Primary Wound Healing
Signup and view all the flashcards
Secondary Wound Healing
Secondary Wound Healing
Signup and view all the flashcards
Tertiary Wound Healing
Tertiary Wound Healing
Signup and view all the flashcards
Goal of Wound Closure
Goal of Wound Closure
Signup and view all the flashcards
Hematoma's Effect
Hematoma's Effect
Signup and view all the flashcards
Bacterial Balance
Bacterial Balance
Signup and view all the flashcards
Tetanus Prophylaxis
Tetanus Prophylaxis
Signup and view all the flashcards
Dressing Functions
Dressing Functions
Signup and view all the flashcards
Study Notes
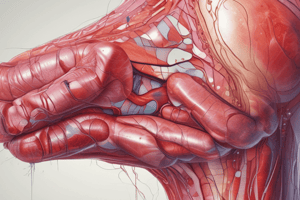
Wounds and Wound Healing
- A wound is a disruption of normal anatomic relationships resulting from an injurious process
- The injury may be intentional, like a surgical incision, or accidental after trauma.
- Biochemical and physiologic healing processes are identical regardless of the cause
Wound Types
- There are three distinct types of wounds, based on the timing of epithelium replacement: primary, secondary, and tertiary
Wound Healing Stages/Phases
- Wound healing can be divided into stages, based on the physiologic process
- The stages are: Hemorrhagic, Substrate, Proliferative, and Remodeling
Hemorrhagic Phase (Hemostasis)
- The first stage of wound healing involves stopping the bleeding
- Hemostasis and clotting occur within seconds to minutes of suffering a wound
- The body activates its emergency repair system to block drainage and prevent blood loss by forming a dam
- Clotting helps close and heal the wound, making a scab
Inflammation
- Inflammation is a basic physiologic process common to all wounds
- Redness (rubor), heat (calor), swelling (tumor), pain (dolor), and loss of function are cardinal signs of inflammation
- These signs can also be seen in wound infections, potentially leading to wound disruption
- The physiology underlying clinical signs is a complex mix of biochemical and cellular events
Biochemical Aspects
- Trauma activates a cascade of chemoattractants and mitogens to recruit phagocytes, fibroblasts, and endothelial cells
- Chemoattractants are produced during blood clotting, degradation of surrounding tissue, and entering cells
- Platelet-derived growth factor (PDGF) is a primary factor released only at the injury site
- PDGF has chemotactic and mitogenic activity toward fibroblasts and smooth muscle cells, appearing as a wound hormone
- Arachidonic acid (AA) is in cell walls and released when cells are injured
- Degradation of AA into prostanoid derivatives like Prostaglandins and thromboxanes triggers inflammatory responses, like vasodilation (rubor), swelling (tumor), and pain (dolor)
Physiologic Aspects
- Leukocytes marginate, stick to vessel walls, and move toward the injury site as biochemical events develop
- Venules dilate, and lymphatics are blocked
Substrate Phase
- The second phase of wound healing is also known as the inflammatory, lag, or exudative phase
- Polymorphonuclear leukocytes (PMN) and macrophages are the primary cells involved
- PMNs appear shortly after wounding and remain predominant for about 48 hours
- Small numbers of bacteria are handled by the macrophages present
- Large numbers of bacteria cannot be controlled, and a neutropenic state leads to a clinical wound infection
- Macrophages are crucial for normal wound healing, not neutrophils
- Monocytes enter the wound after PMNs, reaching maximum numbers about 24 hours later, and evolve into macrophages for wound debridement
- Macrophages secrete substances that cause fibroblasts to replicate (macrophage-derived growth factor (MDGF)) and blood vessels to approach the wound (wound angiogenesis factor (WAF))
- The clot, debris, and bacteria are removed, and substrates for collagen synthesis are arranged
- The process occurs over approximately a 4-day period in primary wound healing
- The wound appears edematous and erythematous, which may be difficult to distinguish from early signs of wound infection
- Healing by secondary or tertiary intention indefinitely continues this phase until the wound surface is closed by ectodermal elements
Proliferative Phase
- The wound appears less edematous and inflamed, but the scar itself may appear raised, red, and hard
- Collagen production in the wound characterizes this phase
- Fibroblasts, which makes the collagen, are the main cells in this phase
- Collagen is the principal structural protein of the body and is ubiquitous through all tissues
- Collagen synthesis begins with amino acid chain production in the cytoplasm
- In the primary wound, collagen production begins about day 7 and continues until approximately day 60
- Collagen production is not constant; slow at first, then a rapid spurt from day 18 to approximately day 50 occurs
- Increased collagen proliferation reflects a rapid gain in tensile strength during this period
Maturation Phase
- The fourth and final phase of wound healing is the remodeling or maturation phase
- Collagen maturation with intermolecular cross-linking characterizes it
- The wound scar gradually flattens, becomes less prominent, paler, and more supple
- Metabolic activity remains high, although there is no net collagen production
- Maturation corresponds clinically to scar flattening and requires approximately 9 months in the adult
- Phases are divided into categories to describe the predominant physiologic process
Classification of Healing Wounds: Primary
- In primary healing (healing by first intention), the wound is closed by direct approximation of the wound edges
- Larger defects use pedicled flaps or skin grafts that still result in primary wound healing via immediate coverage with epithelial elements
Classification of Healing Wounds: Secondary
- Secondary healing (spontaneous wound closure) heals spontaneously by leaving the wound open
- Spontaneous wound closure occurs by wound contraction and epithelialization
- Contraction occurs by a centripetal force in the margin of the wound that is generated by myofibroblasts
- Contraction is a normal process
- Contracture, pathological deformity caused by contraction of scar, is not desirable
- Epithelialization is another component of healing by secondary intention
- The inflammatory phase continues unabated in the middle of the open wound
- Granulation tissue is the product of prolonged inflammatory process
- Granulation tissue, consisting of inflammatory cells and capillary proliferation, is the "proud flesh" that was viewed as a sign of healthy wound healing in the past
Classification of Healing Wounds: Tertiary
- Tertiary wound healing (healing by third intention) involves closing a wound by active means after a delay of days to weeks
- This occurs when a granulating, open wound is closed with sutures or sterile tape before it heals
- Closing the wound interrupts the secondary healing process
- Delayed closure should only be performed in wounds with bacterial balance
Factors Affecting Wound Healing
- The goal of all wound closure is expedient, precise, and definitive tissue approximation
- The goal is to also prevent infection, fibrosis, and secondary deformities (wound contracture)
- The amount of tissue trauma that the wound has sustained is extremely important
- A laceration with a knife is minimally damaging, while crush or avulsion injuries are harder to evaluate and manage
- In a crush, large areas of tissue adjacent to the wound are tenuous and difficult to assess for ultimate viability
- Hematoma impedes wound healing, as the collection of clot in the wound does not allow for orderly removal of debris or collagen laying
- Hematoma acts a perfect medium for bacterial proliferation possibly fostering clinical wound infection
- Bacterial contamination and wound infection are factors of extreme importance in local control of wound and proper closure
- All wounds contain varying amounts of bacteria with a biologic balance (or equilibrium)
- Factors that affect equilibrium: blood supply to wound, necrotic debris, local wound care, and use of systemic or topical antimicrobial agents
- Wounds can tolerate 100,000 (10^5) organisms per gram of tissue to be closed successfully
- If more than 100,000 bacteria/g are present, closure leads to clinical wound infection
- Streptococci are the only exception to this and its presence in any quantity is a contraindication to wound closure
- Tetanus prophylaxis is an important consideration
- Prevention focuses on toxoid immunization, thorough cleansing, and debridement
Dressings
- Functions of dressings:
- Protect the wound
- Immobilize the area
- Compress the area evenly
- Absorb secretions
- Be aesthetically acceptable
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.