Podcast
Questions and Answers
What is the first stage of wound healing?
What is the first stage of wound healing?
- Proliferation
- Haemostasis (correct)
- Matrix remodelling
- Inflammation
Which step is NOT part of the inflammatory response?
Which step is NOT part of the inflammatory response?
- Vasodilation
- Recruitment of leukocytes
- Recognition of the injurious agent
- Promotion of apoptosis (correct)
Which of the following is NOT a hallmark of acute inflammation?
Which of the following is NOT a hallmark of acute inflammation?
- Increased blood flow
- Vascular permeability
- Necrosis of tissues (correct)
- Accumulation of leukocytes
What is the role of primary haemostasis in wound healing?
What is the role of primary haemostasis in wound healing?
During the inflammatory response, which of the following steps involves controlling the body's reaction?
During the inflammatory response, which of the following steps involves controlling the body's reaction?
Which phase follows inflammation in the wound healing process?
Which phase follows inflammation in the wound healing process?
What is the primary function of leukocytes during the inflammatory process?
What is the primary function of leukocytes during the inflammatory process?
Which step is the final stage in the 5 R's of inflammation?
Which step is the final stage in the 5 R's of inflammation?
What is the characteristic feature of chronic inflammation in the lung?
What is the characteristic feature of chronic inflammation in the lung?
Which of the following cytokines is primarily involved in angiogenesis?
Which of the following cytokines is primarily involved in angiogenesis?
What role do platelets and leucocytes play in the healing process?
What role do platelets and leucocytes play in the healing process?
What distinguishes purulent inflammation from other types of inflammation?
What distinguishes purulent inflammation from other types of inflammation?
Which statement accurately describes angiogenesis?
Which statement accurately describes angiogenesis?
Which characteristic is NOT associated with acute inflammation of the lung?
Which characteristic is NOT associated with acute inflammation of the lung?
What histological feature distinguishes serous inflammation?
What histological feature distinguishes serous inflammation?
What is the role of pericytes during angiogenesis?
What is the role of pericytes during angiogenesis?
Which growth factor is primarily involved in the formation of new blood vessels during wound healing?
Which growth factor is primarily involved in the formation of new blood vessels during wound healing?
What is the major cell type responsible for remodelling the extracellular matrix during wound healing?
What is the major cell type responsible for remodelling the extracellular matrix during wound healing?
In the wound healing process, which phase follows inflammation?
In the wound healing process, which phase follows inflammation?
Which type of collagen is predominantly found in granulation tissue?
Which type of collagen is predominantly found in granulation tissue?
What is a characteristic of scar tissue compared to uninjured skin?
What is a characteristic of scar tissue compared to uninjured skin?
What is the first phase of wound healing that involves vasoconstriction?
What is the first phase of wound healing that involves vasoconstriction?
During the healing process, which ECM protein is NOT associated with fibroblasts' role in remodelling?
During the healing process, which ECM protein is NOT associated with fibroblasts' role in remodelling?
What is the main consequence of replacing collagen type III with type I during healing?
What is the main consequence of replacing collagen type III with type I during healing?
Flashcards
Haemostasis
Haemostasis
The first stage of wound healing, stopping bleeding after vascular damage. This involves vasoconstriction, primary haemostasis, and secondary haemostasis.
Inflammation
Inflammation
A protective response to injury or infection, involving vascular dilation, leukocyte accumulation, and fluid in tissues. It's essential for fighting invaders and promoting healing.
Proliferation/Angiogenesis
Proliferation/Angiogenesis
The stage of wound healing where new tissue is formed, including blood vessels (angiogenesis) and cells that build the new tissue.
Matrix Remodelling
Matrix Remodelling
Signup and view all the flashcards
What are the steps involved in haemostasis?
What are the steps involved in haemostasis?
Signup and view all the flashcards
What are the steps involved in inflammation?
What are the steps involved in inflammation?
Signup and view all the flashcards
Acute Inflammation
Acute Inflammation
Signup and view all the flashcards
Chronic Inflammation
Chronic Inflammation
Signup and view all the flashcards
Serous inflammation
Serous inflammation
Signup and view all the flashcards
Fibrinous inflammation
Fibrinous inflammation
Signup and view all the flashcards
Purulent inflammation
Purulent inflammation
Signup and view all the flashcards
Angiogenesis
Angiogenesis
Signup and view all the flashcards
Proliferation
Proliferation
Signup and view all the flashcards
Cellular mediators of tissue repair
Cellular mediators of tissue repair
Signup and view all the flashcards
Collagen Types in Wound Healing
Collagen Types in Wound Healing
Signup and view all the flashcards
Fibroblast Role in Wound Healing
Fibroblast Role in Wound Healing
Signup and view all the flashcards
Scar Tissue
Scar Tissue
Signup and view all the flashcards
Inflammation in Wound Healing
Inflammation in Wound Healing
Signup and view all the flashcards
Proliferation During Wound Healing
Proliferation During Wound Healing
Signup and view all the flashcards
Study Notes
Wound Healing 2
- Wound healing involves four key steps: haemostasis, inflammation, proliferation/angiogenesis, and matrix remodelling.
Haemostasis
- The first stage of wound healing
- Stops bleeding after vascular damage
- Three main steps:
- Vasoconstriction
- Primary haemostasis
- Secondary haemostasis
Inflammation
- The primary defence against pathogenic wound invasion
- A response of vascular tissues to infections and tissue damage, bringing necessary cells and molecules to the affected area.
- Characterised by dilation of small blood vessels and accumulation of leukocytes and fluid in the extravascular tissue.
- Morphologic hallmarks: oedema, redness, warmth, and swelling; pain
- Key players: neutrophils, macrophages, mast cells, monocytes
- Steps of inflammation (5 R's):
- Recognition of the injurious agent
- Recruitment of leucocytes
- Removal of the agent
- Regulation (control) of the response
- Resolution (repair)
- Types of inflammation:
- Acute (e.g., injury, infection):
- Resolution: clearance of stimuli, inflammatory cells, and injured cells
- Progression to chronic if not resolved (e.g., persistent injury, autoimmune)
- Potential for pus formation (abscess)
- Chronic (e.g., chronic infections, autoimmune):
- Persistent inflammation, mononuclear cell infiltrate, and fibrosis (scar)
- Acute (e.g., injury, infection):
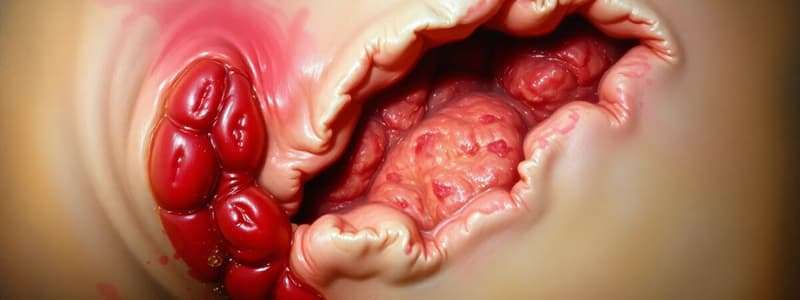
- Forms of inflammation
- Serous: fluid leakage into tissues
- Fibrinous: fibrin-rich exudate
- Purulent: pus-forming (Images included in the slides show examples.)
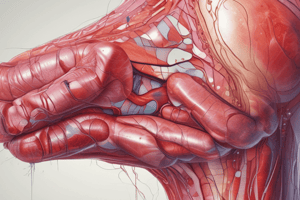
Proliferation and Angiogenesis
- Occurs after inflammation subsides
- Angiogenesis: involves endothelial cell proliferation, migration, and branching to form new blood vessels.
- Pericytes provide structural integrity to endothelial cells.
- Growth factors (e.g., Fibroblasts Growth Factor (FGF), Transforming Growth Factor beta (TGF-β), Platelet-derived Growth Factor (PDGF), Vascular endothelial growth factor (VEGF),Keratinocyte growth factor (KGF), Insulin Growth factor (IGF)) are crucial.
- Growth factors produced by platelets and leukocytes drive the subsequent healing phases.
- Needed for tissue repair and wound closure
Matrix Remodelling
- The rebuilding of the ECM (extracellular matrix) part of the injury response
- Fibroblasts are dominant cells in this process—replacing the initial fibrin clot with components such as hyaluronan, fibronectin, and proteoglycans.
- The formation of mature collagen fibres leads to the formation of a scar.
- ECM never fully returns to that of unwounded skin.
- The granulation tissue (type III collagen-rich) is eventually replaced primarily by collagen type I, increasing tensile strength of the scar.
Summary
- Wound healing involves four essential phases: haemostasis (the initial step), inflammation (defence mechanism), proliferation/angiogenesis (building new tissue and vessels), and matrix remodelling (regenerating the extracellular matrix, scarring).
- Growth factors are important elements throughout each phase.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.