Podcast
Questions and Answers
What is the primary role of neutrophils in the wound healing process?
What is the primary role of neutrophils in the wound healing process?
- Phagocytosis of bacteria and tissue debris (correct)
- Recruitment and activation of fibroblasts
- Synthesis of extracellular matrix
- Release of platelet-derived growth factor
Which of the following is NOT a key player in the hemostasis phase?
Which of the following is NOT a key player in the hemostasis phase?
- Platelets
- Platelet-derived growth factor
- Clotting factors
- Macrophages (correct)
What is the final product of the hemostasis phase?
What is the final product of the hemostasis phase?
- Fibrin mesh (correct)
- Platelet plug
- Granular tissue
- Vascular bed
During which phase of wound healing do macrophages appear in the wound site?
During which phase of wound healing do macrophages appear in the wound site?
What is the primary function of platelet-derived growth factor?
What is the primary function of platelet-derived growth factor?
Which phase of wound healing involves the formation of a new vascular bed?
Which phase of wound healing involves the formation of a new vascular bed?
What is the role of serotonin in wound healing?
What is the role of serotonin in wound healing?
What is the primary function of macrophages in the inflammatory phase?
What is the primary function of macrophages in the inflammatory phase?
What is the primary function of cytokines and growth factors in wound healing?
What is the primary function of cytokines and growth factors in wound healing?
Which type of protein is involved in the formation of granulation tissue?
Which type of protein is involved in the formation of granulation tissue?
What is the primary purpose of the remodeling phase of wound healing?
What is the primary purpose of the remodeling phase of wound healing?
What is the role of myofibroblasts in the remodeling phase of wound healing?
What is the role of myofibroblasts in the remodeling phase of wound healing?
What is the effect of pressure on wound healing?
What is the effect of pressure on wound healing?
What is the importance of vitamin C in wound healing?
What is the importance of vitamin C in wound healing?
What is the characteristic of primary intention wound healing?
What is the characteristic of primary intention wound healing?
What is the role of myofibroblasts in secondary intention wound healing?
What is the role of myofibroblasts in secondary intention wound healing?
Flashcards are hidden until you start studying
Study Notes
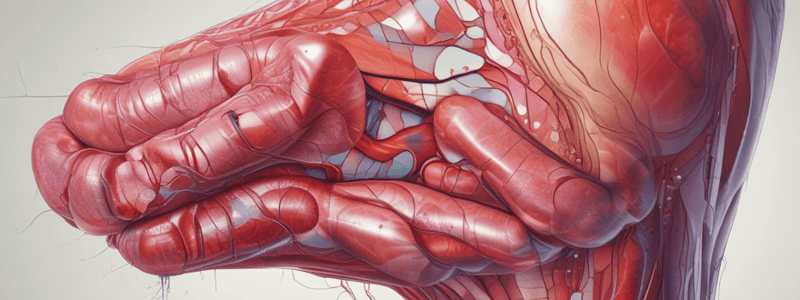
Wound Healing Process
- Wound healing is a complex process involving four overlapping phases: hemostasis, inflammation, proliferation, and remodeling.
- Hemostasis is the first phase, which is initiated by an injury or wound, and involves vasospasm, vessel constriction, platelet plug formation, and activation of the coagulation system.
- The final product of hemostasis is a fibrin mesh, which serves as scaffolding for the migration of inflammatory cells.
Hemostasis Phase
- Key players in the hemostasis phase are platelets and clotting factors, which normally circulate in the blood.
- Platelets release substances that help initiate wound repair, such as platelet-derived growth factor, transforming growth factor beta, platelet activating factor, and fibronectin.
- Platelets also release serotonin, which facilitates cell migration by increasing vascular permeability.
Inflammation Phase
- The inflammatory response is the second phase of wound healing, and involves an increase in adhesion molecules, cytokines, and vasodilation.
- Key players in the inflammation phase are neutrophils and macrophages.
- Neutrophils infiltrate the wound site 24-48 hours after injury, and their primary role is phagocytosis of bacteria and tissue debris.
- Macrophages appear in the wound site 72 hours after injury, and play many roles, including phagocytosis, recruitment and activation of fibroblasts, endothelial cells, and more inflammatory cells, as well as promoting extracellular matrix synthesis.
Proliferation Phase
- The proliferative phase is the third phase of wound healing, and involves the formation of a new vascular bed and the filling of the wound with granular tissue.
- Key players in the proliferation phase are cells that have been recruited and proliferated thanks to the cytokines released by macrophages during the inflammatory phase.
- The proliferation phase can be subdivided into three major processes: angiogenesis, granulation, and re-epithelialization.
- Angiogenesis is the formation of new blood vessels, promoted by cytokines and growth factors such as tumor necrosis factor alpha, transforming growth factor beta, and vascular endothelial growth factor.
- Granulation involves the attraction of fibroblasts to the wound by growth factors, and the formation of a matrix consisting of adhesive proteins, proteoglycans, and glycosaminoglycan gel, as well as fibrous proteins such as collagen and elastin.
- Re-epithelialization involves the proliferation and migration of keratinocytes to re-establish barrier function.
Remodeling Phase
- The remodeling phase is the final phase of wound healing, and involves the formation of new epithelium and scar tissue.
- The primary purpose of the remodeling phase is to achieve a balance of matrix accumulation and breakdown, leading to the formation of scar tissue.
- Key players in the remodeling phase are fibroblasts and their evolution, myofibroblasts.
- Myofibroblasts are capable of contracting and altering the extracellular matrix, producing scar tissue.
Factors Affecting Wound Healing
- Impaired wound healing can be caused by local factors, such as wound type, size, and location, pressure, edema, dehydration, blood supply, underlying infection, and foreign material.
- Systemic factors that can affect wound healing include age, medications, comorbidities, and nutritional deficiencies.
- Vitamin C is a specific nutrient that is important for wound healing.
Types of Wound Healing
- There are two main types of wound healing: primary intention and secondary intention.
- Primary intention is where the edges of the wound are sutured or stapled close, and the wound heals quickly with minimal tissue loss.
- Secondary intention is where the sides of the wound are not opposed, and healing occurs from the bottom of the wound upwards, involving granulation tissue formation and re-epithelialization.
- Myofibroblasts play a major role in secondary intention wound healing.
Wound Healing Process
- Wound healing involves four overlapping phases: hemostasis, inflammation, proliferation, and remodeling.
Hemostasis Phase
- Initiated by injury, hemostasis involves vasospasm, vessel constriction, platelet plug formation, and coagulation activation.
- Platelets release substances like platelet-derived growth factor, transforming growth factor beta, and fibronectin to initiate wound repair.
- Platelets also release serotonin, which facilitates cell migration by increasing vascular permeability.
Inflammation Phase
- The inflammatory response involves increased adhesion molecules, cytokines, and vasodilation.
- Neutrophils infiltrate the wound site 24-48 hours after injury, primarily phagocytosing bacteria and tissue debris.
- Macrophages appear 72 hours after injury, playing roles in phagocytosis, cell recruitment, and extracellular matrix synthesis.
Proliferation Phase
- This phase involves forming a new vascular bed and filling the wound with granular tissue.
- Key cells include those recruited and proliferated due to macrophage-released cytokines during inflammation.
- The phase has three main processes: angiogenesis, granulation, and re-epithelialization.
- Angiogenesis involves forming new blood vessels promoted by cytokines and growth factors like tumor necrosis factor alpha and vascular endothelial growth factor.
- Granulation involves fibroblast attraction and formation of a matrix with adhesive proteins, proteoglycans, and glycosaminoglycan gel.
- Re-epithelialization involves keratinocyte proliferation and migration to re-establish barrier function.
Remodeling Phase
- This final phase involves forming new epithelium and scar tissue.
- The primary purpose is achieving a balance of matrix accumulation and breakdown for scar tissue formation.
- Key players include fibroblasts and their evolution, myofibroblasts, which contract and alter the extracellular matrix.
Factors Affecting Wound Healing
- Local factors affecting wound healing include wound type, size, location, pressure, edema, dehydration, blood supply, underlying infection, and foreign material.
- Systemic factors include age, medications, comorbidities, and nutritional deficiencies.
- Vitamin C is essential for wound healing.
Types of Wound Healing
- There are two main types: primary intention and secondary intention.
- Primary intention involves suturing or stapling, resulting in quick healing with minimal tissue loss.
- Secondary intention involves granulation tissue formation and re-epithelialization, with myofibroblasts playing a major role.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.