Podcast
Questions and Answers
What does a positive dipstick test for blood indicate?
What does a positive dipstick test for blood indicate?
- Normal erythrocyte levels
- Presence of haem pigment (correct)
- Renal parenchymal disease
- Presence of red blood cells
What type of casts indicate renal parenchymal disease?
What type of casts indicate renal parenchymal disease?
- Granular casts (correct)
- Hyaline casts
- Mucous casts
- Fatty casts
What does 'active' sediment typically indicate?
What does 'active' sediment typically indicate?
- Renal inflammation and/or cell necrosis (correct)
- No inflammation
- Normal cellular health
- Increased urine concentration
What should be noted about the examination of urine samples?
What should be noted about the examination of urine samples?
How many erythrocytes do healthy individuals pass on average per day?
How many erythrocytes do healthy individuals pass on average per day?
What is typically true about the appearance of erythrocytes in urine?
What is typically true about the appearance of erythrocytes in urine?
What is a characteristic of hyaline casts?
What is a characteristic of hyaline casts?
What does a normal urinary blood report usually indicate?
What does a normal urinary blood report usually indicate?
What is a key factor contributing to renal impairment in glomerular disease?
What is a key factor contributing to renal impairment in glomerular disease?
Which of the following is NOT a consequence of glomerular disease?
Which of the following is NOT a consequence of glomerular disease?
What causes hypertension in acute nephritis?
What causes hypertension in acute nephritis?
How is the diagnosis of glomerular disease established?
How is the diagnosis of glomerular disease established?
What is indicated by a low serum concentration of the third complement component (C3)?
What is indicated by a low serum concentration of the third complement component (C3)?
Which pathophysiological feature underlies proteinuria in glomerular disease?
Which pathophysiological feature underlies proteinuria in glomerular disease?
What contributes to the structural damage in renal impairment associated with glomerular disease?
What contributes to the structural damage in renal impairment associated with glomerular disease?
What role does the renin-angiotensin system play in glomerular disease?
What role does the renin-angiotensin system play in glomerular disease?
Which serological test result is primarily associated with post-streptococcal glomerulonephritis (GN)?
Which serological test result is primarily associated with post-streptococcal glomerulonephritis (GN)?
What does a low serum complement level, specifically low C3, indicate?
What does a low serum complement level, specifically low C3, indicate?
Which antibody is crucial for diagnosing systemic lupus erythematosus?
Which antibody is crucial for diagnosing systemic lupus erythematosus?
The term 'microscopic polyangiitis' is associated with which antibody?
The term 'microscopic polyangiitis' is associated with which antibody?
In the context of renal lesions, what is the role of a renal biopsy?
In the context of renal lesions, what is the role of a renal biopsy?
Which serological marker is typically elevated in hepatitis C infections?
Which serological marker is typically elevated in hepatitis C infections?
What is a primary cause of acute glomerulonephritis as described in the content?
What is a primary cause of acute glomerulonephritis as described in the content?
Which disease is associated with low serum complement levels (both C3 and C4)?
Which disease is associated with low serum complement levels (both C3 and C4)?
What is a common presentation of IgA disease?
What is a common presentation of IgA disease?
Which statement accurately differentiates post-streptococcal glomerulonephritis (GN) from IgA disease?
Which statement accurately differentiates post-streptococcal glomerulonephritis (GN) from IgA disease?
What is the prognosis associated with IgA disease?
What is the prognosis associated with IgA disease?
What type of kidney biopsy finding is characteristic of IgA disease?
What type of kidney biopsy finding is characteristic of IgA disease?
What condition is characterized by its absence of recurrence?
What condition is characterized by its absence of recurrence?
When does acute nephritis commonly present in IgA disease?
When does acute nephritis commonly present in IgA disease?
What serological finding is typically associated with post-streptococcal GN?
What serological finding is typically associated with post-streptococcal GN?
What key clinical feature distinguishes IgA disease from post-streptococcal GN?
What key clinical feature distinguishes IgA disease from post-streptococcal GN?
What is the most common form of glomerulonephritis (GN) worldwide?
What is the most common form of glomerulonephritis (GN) worldwide?
Which condition is NOT an important cause of acute nephritic syndrome?
Which condition is NOT an important cause of acute nephritic syndrome?
Which presentation is RARELY associated with IgA disease?
Which presentation is RARELY associated with IgA disease?
What type of distribution is observed in immunofluorescence for IgA disease?
What type of distribution is observed in immunofluorescence for IgA disease?
Which of the following conditions is characterized by rapidly progressive renal failure?
Which of the following conditions is characterized by rapidly progressive renal failure?
What is the second most frequent condition causing end-stage kidney disease?
What is the second most frequent condition causing end-stage kidney disease?
Which of the following describes a possible systemic presentation of IgA disease?
Which of the following describes a possible systemic presentation of IgA disease?
Which of these conditions is primarily associated with systemic diseases and can lead to acute nephritic syndrome?
Which of these conditions is primarily associated with systemic diseases and can lead to acute nephritic syndrome?
Flashcards are hidden until you start studying
Study Notes
Urine Analysis
- Dipstick testing detects haem pigments but microscopy is required to confirm the presence of red blood cells
- Urinary casts can be formed from cells in the tubular lumen, indicating renal disease
- Hyaline casts are formed from Tamm-Horsfall protein and are usually non-specific
- A urine sample should be examined fresh as casts may break down within 1-2h
Red Blood Cells in Urine
- Healthy individuals pass up to 2 million erythrocytes in their urine per day
- These cells generally come from the kidney and are dysmorphic
- Dipstick tests are very sensitive and generally do not detect normal levels of erythrocytes
Urinary Casts
- Hyaline casts are non-specific
- Cellular casts (epithelial, red or white blood cells) are associated with renal parenchymal disease
- Granular casts are associated with renal parenchymal disease
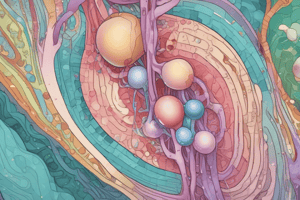
Glomerular Disease
- Proteinuria is caused by impaired filtration barrier function of the glomerular capillary wall
- Haematuria can be caused by leakage across the glomerular capillary wall and into the tubular lumen
- Renal impairment can result from structural and/or functional damage to the glomeruli and tubulointerstitium
- Hypertension is caused by salt and water retention, glomerular capillary and arteriole scarring, and activation of the renin-angiotensin system
Post-Streptococcal Glomerulonephritis
- It is often caused by a streptococcal throat infection occurring 2 weeks before the onset of GN
- Serum antistreptococcal titres are elevated
- Complement activation is indicated by a reduced concentration of the C3 component
- The renal lesions are caused by an immunological reaction to nephritogenic antigens
Glomerulonephritis
- Diagnosis of glomerulonephritis can be made by clinical features, serological tests and renal biopsy
- Important serological tests include:
- serum complement (C3 and C4)
- antinuclear antibodies (ANA)
- anti-double stranded DNA antibodies
- anti-neutrophil cytoplasmic antibodies (ANCA)
- anti-glomerular basement membrane antibody (anti-GBM)
- antistreptococcal titres (ASOT)
- hepatitis B surface antigen (HBsAg)
- hepatitis C antibody (anti-HCV)
- HIV antibody
- Venereal Disease Research Laboratory (VDRL)
- anti-phospholipase A2 receptor
- Renal biopsy is also essential to make a definitive diagnosis, which includes light microscopy, electron microscopy, and immunofluorescence microscopy
IgA Disease
- Common type of GN characterized by acute nephritis and macroscopic haematuria
- Occurs at the time or within a few days of a viral sore throat
- Can be distinguished from post-streptococcal GN by its shorter prodrome, frequently recurrent nature and lack of elevated ASOT and reduced C3 levels
- It is the most common form of GN worldwide
- It can range from isolated microscopic haematuria to rapidly progressive GN
- Patients with IgA disease are at increased risk of developing end-stage kidney disease
- It often presents with macroscopic haematuria (a common feature not seen in post-streptococcal GN)
- The prognosis is highly variable but often better than post-streptococcal GN
Acute Nephritic Syndrome
- Can occur in several conditions that are restricted to the kidney or involve multiple organs
- Important causes include:
- Post-streptococcal glomerulonephritis
- Post-infectious glomerulonephritis
- IgA disease
- Mesangiocapillary (membranoproliferative) glomerulonephritis
- Crescentic glomerulonephritis
- Systemic lupus erythematosus
- Microscopic polyangiitis
- Granulomatosis with polyangiitis
- Rapidly progressive GN, in which renal failure develops over a period of days to weeks, is characteristic of several of these conditions
Henoch-Schönlein Purpura
- Can occur in association with IgA nephritis
- It causes a systemic vasculitis with skin, joint, gastrointestinal, and renal involvement
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.