Podcast
Questions and Answers
What is a risk factor for developing osteoporosis?
What is a risk factor for developing osteoporosis?
- Young age
- High estrogen levels
- Regular Vitamin D intake
- Alcohol consumption (correct)
Osteoporosis is often diagnosed before a fracture occurs.
Osteoporosis is often diagnosed before a fracture occurs.
False (B)
What is the primary treatment approach for osteoporosis?
What is the primary treatment approach for osteoporosis?
Prevention, muscle strengthening, calcium and Vitamin D supplements, bisphosphonates (such as Fosamax and Boniva), and Raloxifene (Evista)
_____ is the removal of plasma or substances from plasma, often used to treat autoimmune diseases.
_____ is the removal of plasma or substances from plasma, often used to treat autoimmune diseases.
Match the following neurological assessment scales with their purposes:
Match the following neurological assessment scales with their purposes:
Flashcards are hidden until you start studying
Study Notes
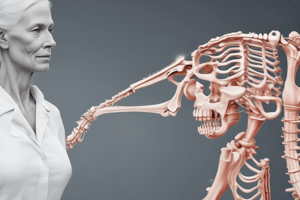
Osteoporosis
- Chronic condition characterized by bone deterioration leading to fractures
- Results from an imbalance between osteoclasts (break down bone) and osteoblasts (build bone)
- Silent disease, often diagnosed after a fracture occurs
- Risk factors include alcohol consumption, Vitamin D deficiency, caffeine, and age (post-menopausal women with decreased estrogen)
- Diagnosis: Bone mineral density test (T score: -1 and above is normal, -1 to -2.5 indicates low bone density, -2.5 and below indicates osteoporosis)
- Treatment: Prevention is key, muscle strengthening, Calcium and Vitamin D supplements, bisphosphonates (impede bone resorption), and estrogen antagonists (help with bone remodeling)
Meningococcal Meningitis
- Inflammation of the meninges caused by N. meningitidis bacteria
- Transmission: Inhaled through the respiratory tract
- Symptoms: Fever, headache, altered mental status, nuchal rigidity, and petechial rash
- Diagnosis: CSF exam via lumbar puncture
- Treatment: Broad-spectrum antibiotics for 14-21 days, droplet precautions
- Complications: Decreased calcium levels, urticarial rash (hives), bacterial infection
Meningitis (Viral)
- Inflammation of the meninges caused by a viral infection
- Symptoms: Fever, headache, altered mental status, nuchal rigidity
- Diagnosis: CSF with viral infection will be clear, with increased protein and normal glucose levels
- Cerebrospinal fluid: Clear fluid found in the brain and spinal cord, assessed in neurological conditions
Alzheimer's Disease
- Gradual progression of brain function loss
- Affects memory, thinking, and behavior
- Symptoms: Forgetfulness, language difficulty, short-term memory loss, personality changes, difficulty with problem-solving
- Diagnosis: Autopsy, symptoms
- Treatment: Medications to help with progression (Aricept, Namenda), nursing care (reorient patient, engage in activities, use gestures, validate feelings)
Parkinson's Disease
- Progressive neurodegenerative disease affecting motor function
- Symptoms: Resting tremors, muscle rigidity, slowness or loss of movement, postural instability (falls), mask-like face
- Treatment: Anticholinergics (reduce tremors), dopamine receptor agonists, nursing care (smaller meals, increased head of bed, promote independence)
Epilepsy
- Chronic disorder characterized by two or more seizures within 24 hours
- Symptoms: Sensory disturbance, loss of LOC, convulsions
- Treatment: Anticonvulsants, brain surgery, nursing care (IV access, suction at bedside, side rails up)
Seizures and Related Pharmacology
- Sudden, uncontrolled, excessive discharge of electrical activity from the brain
- Symptoms: Behavior changes, convulsions, loss of LOC
- Types: Partial and generalized seizures
- Diagnosis: CT, MRI
- Treatment: Anticonvulsants, status epilepticus emergency management
Spinal Cord Injury
- Damage to the spinal cord resulting in functional loss of mobility or sensation
- Causes: Concussion, contusion, compression, tearing, laceration, transection, or ischemia of the spinal cord
- Symptoms: Depend on the level of injury (cervical, thoracic, lumbar, sacral)
- Treatment: No reversal of spinal cord damage, assess/maintain airway, breathing, and circulation, manage complications
Increased Intracranial Pressure
- Increased pressure in the skull due to brain tissue, blood, or CSF
- Symptoms: Changes in VS (bradycardia, decreased respirations, temperature, hypertension), projectile vomiting, decerebrate posturing, aphasia, dilated pupils, widened pulse pressure
- Treatment: Decrease pressure with medications, raising head of bed, maintaining airway, surgical procedure
MRI
- Magnetic resonance imaging, used to assess for diseases or organs
- Gives a 3D image, patients should not have metal on them, can return to normal activities after the procedure
Osteomalacia
- Softening of the bones due to Vitamin D deficiency
- Can lead to osteoporosis
- Treatment: Vitamin D supplements or sun exposure
Bacterial Meningitis
- Inflammation of the meninges caused by bacteria
- Symptoms: Fever, nuchal rigidity, altered mental status, headache
- Diagnosis: CSF lumbar puncture, wait for C&S
- Treatment: Broad-spectrum antibiotics IV, droplet precautions
Traumatic Brain Injury
- Disruption to normal brain function due to trauma (blow, bump)
- Types: Fractures, hematomas, contusions, penetrating injury
- Treatment: Anticholinergics, dopamine receptor agonists, nursing care (increased head of bed, promote independence, suction at bedside)
Concussion
- Blunt force to the head causing the brain to hit the inside of the skull
- Symptoms: Memory problems, headache, N/V
- Treatment: Rest, do not let patients drive home after having a concussion
Stroke
- Disruption of blood flow in the brain
- Causes: Blood vessel blockage (ischemic stroke) or bleeding into the brain (hemorrhagic stroke)
- Symptoms: Weakness, trouble speaking, severe headache, dizziness
- Treatment: Depends on type (ischemic tPA, hemorrhagic surgical interventions)
- Nursing care: Ask when symptoms started, keep patient supine
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.