Podcast
Questions and Answers
What is the half-life of Icodec, one of the new Once Weekly Insulins?
What is the half-life of Icodec, one of the new Once Weekly Insulins?
- 7-8 days (correct)
- 10-11 days
- 15-16 days
- 5-6 days
Which of the following statements about Teplizumab is correct?
Which of the following statements about Teplizumab is correct?
- It is used to treat all stages of Type 1 Diabetes.
- It is the first FDA-approved medication for immediate T1D treatment.
- It can delay the onset of T1D for approximately 2 years. (correct)
- It is the only medication approved for diabetes management.
What additional supplies are necessary for managing Type 1 Diabetes?
What additional supplies are necessary for managing Type 1 Diabetes?
- A yearly health plan and a new insulin delivery device.
- Alcohol preps and supplements for insulin degradation.
- Only insulin syringes and testing strips.
- Blood glucose monitoring devices and a medical alert ID. (correct)
Which medications are being studied for their potential use in Type 1 Diabetes management?
Which medications are being studied for their potential use in Type 1 Diabetes management?
What is a critical requirement for a patient to receive Teplizumab?
What is a critical requirement for a patient to receive Teplizumab?
What is the primary cause of Type 1 Diabetes (T1D) as indicated in the overview?
What is the primary cause of Type 1 Diabetes (T1D) as indicated in the overview?
Which combination of factors is acknowledged as contributing to the etiology of T1D?
Which combination of factors is acknowledged as contributing to the etiology of T1D?
What percentage of diabetes cases does Type 1 Diabetes account for in the United States?
What percentage of diabetes cases does Type 1 Diabetes account for in the United States?
What diagnostic tests are employed for the laboratory diagnosis of T1D?
What diagnostic tests are employed for the laboratory diagnosis of T1D?
During which years was a 21% increase in the incidence of T1D observed?
During which years was a 21% increase in the incidence of T1D observed?
Which viral agent has historical autopsy evidence linked to the onset of T1D?
Which viral agent has historical autopsy evidence linked to the onset of T1D?
What has been identified as a potential environmental trigger for T1D related to infant diet?
What has been identified as a potential environmental trigger for T1D related to infant diet?
What is considered the gold standard treatment for managing T1D?
What is considered the gold standard treatment for managing T1D?
What is the fasting plasma glucose (FPG) threshold for diagnosing diabetes?
What is the fasting plasma glucose (FPG) threshold for diagnosing diabetes?
What does a C-Peptide level of < 0.2 nmol/L indicate?
What does a C-Peptide level of < 0.2 nmol/L indicate?
What is the target range for self-monitoring blood glucose?
What is the target range for self-monitoring blood glucose?
Why is continuous glucose monitoring (CGM) advantageous compared to self-monitoring?
Why is continuous glucose monitoring (CGM) advantageous compared to self-monitoring?
What is the A1C target for reducing microvascular complications?
What is the A1C target for reducing microvascular complications?
How often should blood glucose be checked when using self-monitoring methods?
How often should blood glucose be checked when using self-monitoring methods?
What is one of the main disadvantages of using continuous glucose monitors?
What is one of the main disadvantages of using continuous glucose monitors?
What indicates a positive result for diabetes-related antibodies?
What indicates a positive result for diabetes-related antibodies?
What is the primary mechanism by which diabetic ketoacidosis (DKA) develops?
What is the primary mechanism by which diabetic ketoacidosis (DKA) develops?
Which of the following is a common sign of diabetic ketoacidosis?
Which of the following is a common sign of diabetic ketoacidosis?
What is the typical starting dose of Symlin (Pramlintide) for an adult?
What is the typical starting dose of Symlin (Pramlintide) for an adult?
What is the primary adverse effect associated with SGLT1/2 inhibitors?
What is the primary adverse effect associated with SGLT1/2 inhibitors?
In patients with DKA, which treatment is typically initiated first?
In patients with DKA, which treatment is typically initiated first?
Why are SGLT1 inhibitors primarily used in Type 1 diabetes patients with caution?
Why are SGLT1 inhibitors primarily used in Type 1 diabetes patients with caution?
What is the expected hourly fluid replacement for treating DKA?
What is the expected hourly fluid replacement for treating DKA?
Which condition is likely to require higher doses of insulin treatment?
Which condition is likely to require higher doses of insulin treatment?
What is the general goal for fasting plasma glucose (FPG) during pregnancy to prevent complications?
What is the general goal for fasting plasma glucose (FPG) during pregnancy to prevent complications?
Which of the following is NOT a recommended medication for improving sensation in patients with neuropathy?
Which of the following is NOT a recommended medication for improving sensation in patients with neuropathy?
What annual assessments are recommended for patients to monitor kidney function during pregnancy?
What annual assessments are recommended for patients to monitor kidney function during pregnancy?
How often should patients be screened for distal symmetric polyneuropathy (DPN) after being diagnosed with type 2 diabetes?
How often should patients be screened for distal symmetric polyneuropathy (DPN) after being diagnosed with type 2 diabetes?
What is a potential consequence of neuropathy combined with poor perfusion in diabetic patients?
What is a potential consequence of neuropathy combined with poor perfusion in diabetic patients?
What is the primary reason for the increase in autoimmune destruction of beta cells in Type 1 Diabetes?
What is the primary reason for the increase in autoimmune destruction of beta cells in Type 1 Diabetes?
What percentage of diabetes cases does Type 1 Diabetes account for in the United States?
What percentage of diabetes cases does Type 1 Diabetes account for in the United States?
Which environmental factor is linked to the onset of Type 1 Diabetes according to historical evidence?
Which environmental factor is linked to the onset of Type 1 Diabetes according to historical evidence?
What is a common diagnostic marker indicating autoimmune activity in Type 1 Diabetes?
What is a common diagnostic marker indicating autoimmune activity in Type 1 Diabetes?
What treatment modality is considered the gold standard for managing Type 1 Diabetes?
What treatment modality is considered the gold standard for managing Type 1 Diabetes?
What is one of the key anatomical changes observed in the pancreas during the progression of Type 1 Diabetes?
What is one of the key anatomical changes observed in the pancreas during the progression of Type 1 Diabetes?
Which laboratory diagnostic test is NOT commonly used for diagnosing Type 1 Diabetes?
Which laboratory diagnostic test is NOT commonly used for diagnosing Type 1 Diabetes?
What is the relationship between the incidence of Type 1 Diabetes and the years between 2001 and 2009?
What is the relationship between the incidence of Type 1 Diabetes and the years between 2001 and 2009?
What is a key goal for fasting plasma glucose (FPG) levels during pregnancy to prevent complications?
What is a key goal for fasting plasma glucose (FPG) levels during pregnancy to prevent complications?
Which medication is NOT considered helpful for improving sensation in diabetic neuropathy?
Which medication is NOT considered helpful for improving sensation in diabetic neuropathy?
What is the recommended frequency for screening patients for distal symmetric polyneuropathy (DPN) after being diagnosed with type 1 diabetes?
What is the recommended frequency for screening patients for distal symmetric polyneuropathy (DPN) after being diagnosed with type 1 diabetes?
Which treatment is recommended if a patient's GFR is found to be less than 30?
Which treatment is recommended if a patient's GFR is found to be less than 30?
What is the significance of Teplizumab in the treatment of Type 1 Diabetes?
What is the significance of Teplizumab in the treatment of Type 1 Diabetes?
What annual measurements are suggested to monitor kidney function during pregnancy?
What annual measurements are suggested to monitor kidney function during pregnancy?
Which of the following is NOT required for managing Type 1 Diabetes according to the content?
Which of the following is NOT required for managing Type 1 Diabetes according to the content?
What is the duration of delay in onset achieved by Teplizumab?
What is the duration of delay in onset achieved by Teplizumab?
Which two new insulins were highlighted for their potential benefits in Type 2 diabetes treatment?
Which two new insulins were highlighted for their potential benefits in Type 2 diabetes treatment?
Which of the following statements about the management of Type 1 Diabetes is accurate?
Which of the following statements about the management of Type 1 Diabetes is accurate?
What is the diagnostic threshold for fasting plasma glucose (FPG) for diagnosing diabetes?
What is the diagnostic threshold for fasting plasma glucose (FPG) for diagnosing diabetes?
Which of the following A1C results indicates a need for further evaluation of diabetes?
Which of the following A1C results indicates a need for further evaluation of diabetes?
What is the minimum frequency recommended for self-monitoring blood glucose (SMBG) in patients with diabetes?
What is the minimum frequency recommended for self-monitoring blood glucose (SMBG) in patients with diabetes?
What is one disadvantage of continuous glucose monitoring (CGM)?
What is one disadvantage of continuous glucose monitoring (CGM)?
Which of the following antibodies indicates a positive result for diabetes-related autoimmunity?
Which of the following antibodies indicates a positive result for diabetes-related autoimmunity?
What is the target range for blood glucose levels in diabetes management?
What is the target range for blood glucose levels in diabetes management?
What does a C-Peptide level of < 0.2 nmol/L indicate?
What does a C-Peptide level of < 0.2 nmol/L indicate?
What is the A1C target for reducing microvascular complications in diabetes?
What is the A1C target for reducing microvascular complications in diabetes?
What is the recommended frequency for patients with Type 1 Diabetes to be seen by a healthcare provider?
What is the recommended frequency for patients with Type 1 Diabetes to be seen by a healthcare provider?
Which of the following is considered a 'quick' carbohydrate source for managing hypoglycemia?
Which of the following is considered a 'quick' carbohydrate source for managing hypoglycemia?
What must be avoided when administering quick carbs for hypoglycemia?
What must be avoided when administering quick carbs for hypoglycemia?
What could be a possible reason for elevated blood glucose levels in a patient with Type 1 Diabetes?
What could be a possible reason for elevated blood glucose levels in a patient with Type 1 Diabetes?
If a patient's blood glucose level is 250 mg/dL with a target of 150 mg/dL, what formula should be applied to determine the correction dose?
If a patient's blood glucose level is 250 mg/dL with a target of 150 mg/dL, what formula should be applied to determine the correction dose?
What is a common symptom of hyperglycemia?
What is a common symptom of hyperglycemia?
What is a critical component of immediate treatment for a patient with hyperglycemia above 250 mg/dL?
What is a critical component of immediate treatment for a patient with hyperglycemia above 250 mg/dL?
What is a general goal for fasting plasma glucose (FPG) during pregnancy to prevent complications?
What is a general goal for fasting plasma glucose (FPG) during pregnancy to prevent complications?
Which medication can help improve sensation in patients with neuropathy?
Which medication can help improve sensation in patients with neuropathy?
How often should patients be screened for distal symmetric polyneuropathy (DPN) after being diagnosed with type 2 diabetes?
How often should patients be screened for distal symmetric polyneuropathy (DPN) after being diagnosed with type 2 diabetes?
What is a recommended action if a patient's GFR is found to be less than 30?
What is a recommended action if a patient's GFR is found to be less than 30?
What is a potential complication of neuropathy combined with poor perfusion in diabetic patients?
What is a potential complication of neuropathy combined with poor perfusion in diabetic patients?
What is the primary benefit of the newly introduced Once Weekly Insulins in studies?
What is the primary benefit of the newly introduced Once Weekly Insulins in studies?
For whom is Teplizumab approved for use in delaying type 1 diabetes onset?
For whom is Teplizumab approved for use in delaying type 1 diabetes onset?
Which of the following is a necessary requirement for every individual with type 1 diabetes?
Which of the following is a necessary requirement for every individual with type 1 diabetes?
What effect do Metformin and GLP-1 Agonists have in the study for managing Type 1 Diabetes?
What effect do Metformin and GLP-1 Agonists have in the study for managing Type 1 Diabetes?
Which statement best describes the financial aspect of Teplizumab treatment?
Which statement best describes the financial aspect of Teplizumab treatment?
How often are patients with Type 1 Diabetes (T1D) typically seen for check-ups?
How often are patients with Type 1 Diabetes (T1D) typically seen for check-ups?
What is a common mistake when administering quick carbohydrates during hypoglycemia?
What is a common mistake when administering quick carbohydrates during hypoglycemia?
What is the primary indicator that warrants checking blood glucose levels more frequently?
What is the primary indicator that warrants checking blood glucose levels more frequently?
What should be done before giving another dose of insulin when treating hyperglycemia?
What should be done before giving another dose of insulin when treating hyperglycemia?
What is the treatment option available for severe hypoglycemia in patients with T1D?
What is the treatment option available for severe hypoglycemia in patients with T1D?
If a patient's blood glucose is 250 mg/dL with a target of 150 mg/dL, how would you calculate the correction dose?
If a patient's blood glucose is 250 mg/dL with a target of 150 mg/dL, how would you calculate the correction dose?
What symptom is commonly associated with hyperglycemia?
What symptom is commonly associated with hyperglycemia?
During an acute illness, what factor may contribute to higher blood glucose levels in T1D patients?
During an acute illness, what factor may contribute to higher blood glucose levels in T1D patients?
What is the primary mechanism by which autoimmune destruction occurs in Type 1 Diabetes?
What is the primary mechanism by which autoimmune destruction occurs in Type 1 Diabetes?
Which factor is considered an environmental trigger for the development of Type 1 Diabetes?
Which factor is considered an environmental trigger for the development of Type 1 Diabetes?
What is a significant anatomical change observed in the pancreas during the progression of Type 1 Diabetes?
What is a significant anatomical change observed in the pancreas during the progression of Type 1 Diabetes?
What percentage of all diabetes cases does Type 1 Diabetes represent in the United States?
What percentage of all diabetes cases does Type 1 Diabetes represent in the United States?
Which laboratory diagnostic test is commonly used to help diagnose Type 1 Diabetes?
Which laboratory diagnostic test is commonly used to help diagnose Type 1 Diabetes?
What does the presence of autoantibodies indicate in the context of Type 1 Diabetes?
What does the presence of autoantibodies indicate in the context of Type 1 Diabetes?
What was the percentage increase in the incidence of Type 1 Diabetes observed between 2001 and 2009?
What was the percentage increase in the incidence of Type 1 Diabetes observed between 2001 and 2009?
What is the gold standard treatment method for managing Type 1 Diabetes?
What is the gold standard treatment method for managing Type 1 Diabetes?
What is the mechanism of action for Symlin (Pramlintide)?
What is the mechanism of action for Symlin (Pramlintide)?
Which of the following signs is commonly associated with diabetic ketoacidosis (DKA)?
Which of the following signs is commonly associated with diabetic ketoacidosis (DKA)?
Which treatment is typically initiated first in managing DKA?
Which treatment is typically initiated first in managing DKA?
What is a common side effect associated with SGLT1 inhibitors?
What is a common side effect associated with SGLT1 inhibitors?
What is the initial insulin drip rate for treating DKA?
What is the initial insulin drip rate for treating DKA?
Which factor is most likely to cause DKA?
Which factor is most likely to cause DKA?
What should be monitored closely in patients using Symlin (Pramlintide)?
What should be monitored closely in patients using Symlin (Pramlintide)?
In what form is Symlin (Pramlintide) administered?
In what form is Symlin (Pramlintide) administered?
What is identified as a primary contributor to the pathophysiology of Type 1 Diabetes?
What is identified as a primary contributor to the pathophysiology of Type 1 Diabetes?
The increase in incidence of Type 1 Diabetes between 2001 and 2009 was reported at what percentage?
The increase in incidence of Type 1 Diabetes between 2001 and 2009 was reported at what percentage?
Which environmental factor has been associated with an increased risk of developing Type 1 Diabetes according to historical evidence?
Which environmental factor has been associated with an increased risk of developing Type 1 Diabetes according to historical evidence?
What is the significance of autoantibodies in the context of Type 1 Diabetes diagnosis?
What is the significance of autoantibodies in the context of Type 1 Diabetes diagnosis?
In Type 1 Diabetes, what anatomical change is often observed in the pancreas?
In Type 1 Diabetes, what anatomical change is often observed in the pancreas?
What is a key factor that combines with genetic predisposition to contribute to the etiology of Type 1 Diabetes?
What is a key factor that combines with genetic predisposition to contribute to the etiology of Type 1 Diabetes?
Which laboratory diagnostic marker is relevant for the diagnosis of Type 1 Diabetes?
Which laboratory diagnostic marker is relevant for the diagnosis of Type 1 Diabetes?
What primary treatment modality is considered the gold standard for individuals diagnosed with Type 1 Diabetes?
What primary treatment modality is considered the gold standard for individuals diagnosed with Type 1 Diabetes?
What is a common mistake when consuming quick carbohydrates for managing low blood sugar?
What is a common mistake when consuming quick carbohydrates for managing low blood sugar?
When should patients with Type 1 Diabetes typically have their blood glucose monitored?
When should patients with Type 1 Diabetes typically have their blood glucose monitored?
What can commonly cause high blood glucose levels in a Type 1 Diabetes patient?
What can commonly cause high blood glucose levels in a Type 1 Diabetes patient?
In case of hyperglycemia, what is the most appropriate waiting period before administering another dose of insulin?
In case of hyperglycemia, what is the most appropriate waiting period before administering another dose of insulin?
What should be monitored when blood glucose levels exceed 250 mg/dL?
What should be monitored when blood glucose levels exceed 250 mg/dL?
What type of carbohydrate should NOT be consumed before a quick carbohydrate to effectively raise blood sugar levels?
What type of carbohydrate should NOT be consumed before a quick carbohydrate to effectively raise blood sugar levels?
What is the most critical symptom of hyperglycemia?
What is the most critical symptom of hyperglycemia?
What type of injection might a friend of a Type 1 Diabetes patient have received that provided rapid relief from symptoms?
What type of injection might a friend of a Type 1 Diabetes patient have received that provided rapid relief from symptoms?
What is a common consequence of untreated diabetic ketoacidosis (DKA)?
What is a common consequence of untreated diabetic ketoacidosis (DKA)?
Which of the following treatments is initially recommended for managing DKA?
Which of the following treatments is initially recommended for managing DKA?
What is a potential side effect of SGLT1/2 inhibitors in Type 1 diabetes patients?
What is a potential side effect of SGLT1/2 inhibitors in Type 1 diabetes patients?
What is the starting dose of Symlin (Pramlintide) when used as an adjunct therapy?
What is the starting dose of Symlin (Pramlintide) when used as an adjunct therapy?
Which breath odor is characteristic of diabetic ketoacidosis?
Which breath odor is characteristic of diabetic ketoacidosis?
In patients requiring more than 200 units of insulin daily, which type of insulin should be considered?
In patients requiring more than 200 units of insulin daily, which type of insulin should be considered?
What condition is indicated by a decreased bicarbonate level during DKA?
What condition is indicated by a decreased bicarbonate level during DKA?
What adverse effect may occur as a result of taking amylin drugs like Symlin?
What adverse effect may occur as a result of taking amylin drugs like Symlin?
What is the general goal for fasting plasma glucose (FPG) levels during pregnancy to prevent complications?
What is the general goal for fasting plasma glucose (FPG) levels during pregnancy to prevent complications?
Which annual assessments are recommended to monitor kidney function during pregnancy?
Which annual assessments are recommended to monitor kidney function during pregnancy?
What is a recommended action if a patient's GFR is found to be less than 30?
What is a recommended action if a patient's GFR is found to be less than 30?
What tests are recommended to screen for distal symmetric polyneuropathy (DPN) at diagnosis?
What tests are recommended to screen for distal symmetric polyneuropathy (DPN) at diagnosis?
Which medication may help with sensation in patients suffering from neuropathy?
Which medication may help with sensation in patients suffering from neuropathy?
What is the primary benefit of the new Once Weekly Insulins Icodec and Efsitora as indicated in the information shared?
What is the primary benefit of the new Once Weekly Insulins Icodec and Efsitora as indicated in the information shared?
What is a requirement for a patient to be eligible for the treatment with Teplizumab?
What is a requirement for a patient to be eligible for the treatment with Teplizumab?
What is a distinctive feature of Teplizumab in the context of Type 1 Diabetes treatment?
What is a distinctive feature of Teplizumab in the context of Type 1 Diabetes treatment?
Which of the following best describes the role of Metformin and GLP-1 Agonists in Type 1 Diabetes management as stated?
Which of the following best describes the role of Metformin and GLP-1 Agonists in Type 1 Diabetes management as stated?
What necessary component is specifically mentioned as important for all individuals with Type 1 Diabetes?
What necessary component is specifically mentioned as important for all individuals with Type 1 Diabetes?
Flashcards are hidden until you start studying
Study Notes
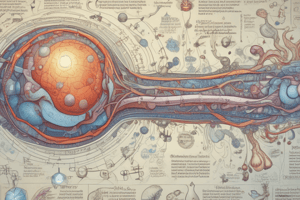
T1D Overview & Pathophysiology
- Autoimmune Destruction: T1D is caused by the immune system attacking and destroying beta cells in the pancreas, which are responsible for producing insulin.
- Genetic Predisposition: Individuals with T1D often have a genetic predisposition, with specific HLA genes (HLA-DQ and HLA-DR) being associated with increased risk.
- Environmental Triggers: Environmental factors, such as exposure to viruses (like Coxsackie B4), autoimmune triggers, and early introduction of cow's milk, may play a role in triggering the autoimmune response.
T1D Epidemiology & Prevalence
- Prevalence in the US: Approximately 1.25 million Americans have T1D, representing only 5-10% of all diabetes cases.
- Increasing Incidence: The incidence of T1D has increased by 21% between 2001 and 2009.
T1D Diagnosis & Treatment
- Diagnostic Tests: Diagnostic tests include:
- HbA1c: reflects average blood sugar levels over 2-3 months.
- Fasting Plasma Glucose (FPG): measures blood sugar after an overnight fast.
- Random Plasma Glucose (RPG): measures blood sugar at any time.
- Antibodies: tests for the presence of autoantibodies (IAA, GADA, IA-2A, ICA).
- C-Peptide: measures the amount of insulin produced by the pancreas.
- Treatment Gold Standard: The gold standard treatment for T1D is insulin therapy, administered through multiple daily injections (MDI) or a continuous insulin pump (CI), along with self-monitoring of blood glucose (SMBG) or continuous glucose monitoring (CGM).
T1D Management & Monitoring
- SMBG: Self-monitoring of blood glucose (SMBG) involves using a finger prick to test blood sugar levels several times a day. The target blood glucose range is typically 80-120 mg/dL.
- CGM: Continuous glucose monitoring (CGM) uses a sensor under the skin to continuously measure blood sugar levels, providing more frequent data and alerts for high or low blood sugar.
T1D Complications
- Diabetic Ketoacidosis (DKA): A life-threatening condition that occurs when the body produces ketones as an alternative energy source due to a lack of insulin. Symptoms include:
- Fruity breath
- Kussmaul respirations
- Nausea and vomiting
- Abdominal pain
- Dehydration
- Fatigue
- Neuropathy: Damage to nerves, often affecting the feet and hands. Symptoms include:
- Numbness
- Tingling
- Pain
- Loss of sensation
- Nephropathy: Kidney damage, often leading to kidney failure. Signs include:
- Increased creatinine levels
- Albuminuria (protein in the urine)
- Increased blood pressure
- Retinopathy: Damage to blood vessels in the retina of the eye, leading to vision loss.
- Cardiovascular Disease: T1D increases the risk of heart attacks, strokes, and other cardiovascular problems.
New Treatments & Research
- Once Weekly Insulins: New insulin analogs with longer-acting formulations, like Icodec and Efsitora, are being investigated for improved blood sugar control and reduced hypoglycemia.
- Teplizumab: An FDA-approved drug that can delay the onset of T1D for about two years in individuals with detectable autoantibodies and without seroconversion to T1D.
- T2DM Medications for T1D: Research is exploring the use of medications originally developed for T2DM, such as metformin and GLP-1 agonists, in the treatment of T1D.
Essential Supplies & Management
- T1D Medical Alert ID: People with T1D should wear an ID bracelet or necklace indicating their condition for emergency situations.
- Insulin: A constant supply of insulin is essential, delivered through injections or an insulin pump.
- Blood Glucose Monitoring Equipment: Frequent monitoring is necessary to manage blood sugar levels.
- Glucagon: Glucagon is a life-saving hormone used to treat a severe low blood sugar episode (hypoglycemia).
- Other Supplies: Additional supplies may include:
- Needles
- Skin adhesive patches
- Blood glucose testing strips
- Alcohol preps
- Extra insulin
- Supplies for low blood sugar
- Regular Healthcare: People with T1D should have regular medical checkups with their healthcare provider, including A1C monitoring, neuro/podiatry assessments, yearly eye exams, and proactive management of complications.
T1D Overview
- Type 1 Diabetes (T1D) is an autoimmune disease characterized by the destruction of beta cells in the pancreas, which are responsible for producing insulin.
- T1D is characterized by a lack of insulin production, leading to hyperglycemia.
- T1D affects roughly 1.25 million Americans, representing 5-10% of all diabetes cases.
- The incidence of T1D has increased by 21% between 2001 and 2009.
T1D Pathophysiology
- T1D develops due to a combination of genetic predisposition (especially HLA-DQ and HLA-DR genes) and environmental triggers.
- Pancreatic tissue samples from individuals with T1D show signs of chronic inflammation in the endocrine regions, with evidence of inflammatory markers.
- The progressive autoimmune process results in a decrease in pancreatic size and weight, as well as the presence of autoantibodies.
T1D Etiology
- Potential triggers for T1D include:
- Coxsackie Virus: Historical evidence from the 1970s shows Coxsackie Virus B4 isolation from islet cells in children with diabetic ketoacidosis.
- Cow's Milk: Early introduction of cow's milk can induce a humoral response, potentially triggering an inflammatory autoimmune reaction due to diabetogenic antigens present in cow's milk.
T1D Presentation and Symptoms
- T1D often presents with classic symptoms of hyperglycemia, including:
- Polyuria (increased urination)
- Polydipsia (increased thirst)
- Polyphagia (increased hunger)
- Blurred vision
- Fatigue
T1D Diagnosis
- T1D diagnosis is based on a combination of clinical presentation and laboratory tests.
- Diagnostic criteria include:
- HbA1c > 6.5%
- Fasting Plasma Glucose (FPG) > 126 mg/dL
- Random Plasma Glucose (RPG) > 200 mg/dL
- Presence of diabetes-specific antibodies (e.g., Insulin Autoantibodies (IAA), Glutamic Acid Decarboxylase Autoantibodies (GADA), Zinc Transporter-8 Autoantibodies (ZnT8A), Islet Cell Cytoplasmic Autoantibodies (ICA))
- C-Peptide < 0.2 nmol/L
- Hyperglycemia in the presence of antibodies
T1D Treatment
- The gold standard treatment for T1D involves insulin therapy administered via different methods:
- Multiple Daily Injections (MDI)
- Continuous Insulin Infusion (CI)
- Blood glucose monitoring is essential to manage T1D:
- Self-Monitoring of Blood Glucose (SMBG)
- Continuous Glucose Monitoring (CGM)
- Target blood glucose levels are typically between 80-120 mg/dL.
Managing Hypoglycemia and Hyperglycemia
- Hypoglycemia is defined as low blood glucose levels, typically below 70 mg/dL.
- Signs and symptoms of hypoglycemia include:
- Shaking, sweating, feeling nervous, hunger, dizziness, and confusion.
- Treatment for hypoglycemia includes consuming quick-acting carbohydrates like juice, glucose tablets, honey, or sugar.
- In severe cases, glucagon injections are administered to increase blood glucose levels.
- Hyperglycemia occurs when blood glucose levels are above 150 mg/dL.
- Symptoms of hyperglycemia include:
- Polyuria (increased urination)
- Polydipsia (increased thirst)
- Polyphagia (increased hunger)
- Blurred vision
- Fatigue.
- Treatment for hyperglycemia involves adjusting insulin dosing and monitoring blood glucose levels.
- Inpatient management of hyperglycemia requires close monitoring and interventions to maintain blood glucose levels within safe ranges.
- Correction factors (CF) can be calculated to determine the necessary insulin dosage for glucose correction.
T1D Complications
- Long-term complications of T1D can impact various organ systems:
- Microvascular complications: Include retinopathy (eye damage), nephropathy (kidney damage), and neuropathy (nerve damage).
- Macrovascular complications: Include cardiovascular disease, peripheral vascular disease, and cerebrovascular disease.
- Management of T1D complications involves:
- Regular monitoring and screening for early detection.
- Lifestyle modifications, including diet, exercise, and smoking cessation.
- Medications to manage underlying conditions such as high blood pressure and high cholesterol.
- Neuropathy: Nerve damage, particularly the most common type, distal symmetric polyneuropathy (DPN) can lead to loss of sensation, pain, and balance issues.
- Early screening for DPN in individuals with T1D is recommended, and foot exams should be regularly conducted to identify potential complications.
- Treatment options for DPN include medications such as pregabalin, gabapentin, tricyclic antidepressants (TCAs), and topical treatments like lidocaine or capsaicin.
- Diabetic nephropathy: Involves the progressive deterioration of kidney function.
- Early detection and management are crucial to slow down the progression of kidney disease.
- Treatment includes:
- Annual creatinine, urinary albumin excretion, and potassium monitoring.
- ACE inhibitors or angiotensin II receptor blockers (ARBs) to manage high blood pressure and protect the kidneys.
- Insulin dose adjustments based on GFR.
- Referral to nephrology if GFR falls below 30.
New Developments in T1D Management
- New Insulin Therapies:
- Once-weekly insulin analogs like Icodec (Novo Nordisk) and Efsitora (Lilly) are being investigated for their potential to improve glycemic control and reduce hypoglycemia.
- T1D Onset Delay:
- Teplizumab (ProventionBio & Sanofi) is FDA-approved to delay T1D onset.
- It is effective at delaying the onset of T1D for approximately 2 years in individuals with detectable antibodies and without seroconversion to T1D.
- Investigational Medications:
- T2DM medications like metformin and GLP-1 agonists are being studied for their potential to reduce insulin requirements and improve blood glucose control in people with T1D.
Essential T1D Management Supplies
- Individuals with T1D need a comprehensive set of supplies for effective management:
- T1D Medical Alert ID.
- Insulin (basal and bolus) delivered via various devices (e.g., insulin pens, insulin pumps).
- Needles or infusion sets for insulin delivery depending on the device.
- Skin adhesives for pump sites.
- Blood glucose monitoring equipment (SMBG or CGM) with related supplies (testing strips, lancets, skin adhesives for CGM).
- Glucagon injection (expires annually).
- Supplies for treating hypoglycemia.
- Alcohol preps for cleansing injection sites.
Importance of Regular Monitoring and Follow-Up
- T1D requires a proactive approach to management, including:
- Quarterly visits with healthcare providers for HbA1c monitoring and neurological and podiatric assessments.
- Yearly fundoscopic exams to evaluate eye health.
- Adherence to health plans for managing T1D at school and in daily life.
- Extra supplies for emergencies such as pump site failures, insulin degradation, or unexpected changes in blood glucose levels.
Type 1 Diabetes Overview
- Type 1 Diabetes (T1D) is an autoimmune disease in which the immune system destroys the insulin-producing beta cells in the pancreas.
- Beta cell destruction is complex and is influenced by genetic predisposition and environmental factors.
- Approximately 1.25 million Americans have T1D which represents only 5-10% of all diabetes cases.
- The incidence of T1D has increased 21% between 2001 and 2009.
T1D Pathophysiology
- Pancreatic tissue samples from individuals with T1D at the onset of symptoms show signs of chronic inflammation in the endocrine portions.
- This inflammation is further evidenced by the presence of autoantibodies.
- Over time, the pancreas undergoes anatomical changes, including a decrease in size and weight, contributing to the progressive autoimmune process.
T1D Etiology
- Genetic Predisposition: Certain genes, particularly those associated with HLA-DQ and HLA-DR, increase susceptibility to T1D.
- Environmental Factors:
- Coxsackie Virus: Historical evidence suggests a link between Coxsackie Virus B4 and the development of T1D.
- Cow's Milk: Early introduction of cow's milk has been associated with an increased risk of T1D due to the presence of diabetogenic antigens that trigger an immune response.
T1D Diagnosis & Treatment
- Diagnosis relies on clinical presentation, laboratory testing, and assessment of autoantibodies.
- Laboratory Tests: Fasting plasma glucose (FPG), random plasma glucose (RPG), glycosylated hemoglobin (A1c), C-peptide, and autoantibody testing.
- Treatment Gold Standard: Insulin therapy through multiple daily injections (MDI) or continuous insulin pumps (CI), combined with self-monitoring of blood glucose (SMBG) or continuous glucose monitoring (CGM).
T1D Management
- Patients with T1D require regular monitoring of blood glucose levels and adjustments to insulin doses based on individual needs.
- Hyperglycemia:
- Symptoms include polyuria, polydipsia, polyphagia, blurry vision, and fatigue.
- Treatment involves insulin correction doses based on blood glucose readings, target blood sugar range, and individual insulin sensitivity.
- For blood glucose levels exceeding 250 mg/dL: check for ketones, adjust fluid intake, and monitor for signs of diabetic ketoacidosis (DKA).
- Hypoglycemia:
- Symptoms include sweating, shakiness, confusion, and loss of consciousness.
- Treatment involves prompt administration of "quick" carbohydrates such as juice, glucose tablets, or honey.
- "Quick" carbs should be followed by a "slow" carb to prevent rebound hyperglycemia.
T1D Complications
- Diabetic Ketoacidosis (DKA): A serious complication of uncontrolled T1D characterized by dehydration, high blood glucose, and accumulation of ketones, leading to metabolic acidosis.
- Long-Term Complications:
- Retinopathy: Damage to the blood vessels in the retina, potentially leading to vision loss.
- Nephropathy: Damage to blood vessels in the kidneys, leading to kidney dysfunction and potentially kidney failure.
- Neuropathy: Damage to nerves, often affecting the feet and hands, causing numbness, pain, and weakness.
Insulin Therapy
- Insulin Resistance: Individuals with insulin resistance may require higher insulin doses and might benefit from higher potency insulin formulations.
- Pregnancy: Tight blood glucose control is crucial during pregnancy to prevent complications for both mother and fetus.
Future Developments
- New Insulin Formulations: Research is ongoing to develop longer-acting insulin analogs aimed at improving blood glucose control and reducing hypoglycemia.
- Prevention: Research is investigating the use of teplizumab, an antibody that can delay the onset of T1D in individuals with detectable autoantibodies.
Importance of Comprehensive Care
- Patients with T1D require regular checkups, including A1C monitoring, neurologic and podiatric assessments, and annual funduscopic exams.
- Proper management of T1D involves close collaboration between patients, healthcare providers, and family members.
T1D Overview
- T1D is an autoimmune disease that causes the body to destroy beta cells in the pancreas, resulting in an inability to produce insulin.
- T1D is a chronic condition that requires lifelong management with insulin therapy.
- Prevalence of T1D is 1.25 million Americans, representing only 5-10% of all diabetes cases.
- Incidence of T1D has increased by 21% between 2001-2009.
T1D Pathophysiology & Etiology
- T1D develops due to genetic predisposition and environmental triggers.
- Genetic factors include HLA-DQ and HLA-DR genes.
- Environmental triggers may include Coxsackie virus, cow’s milk, and other factors.
- Pancreatic tissue specimens taken at the onset of symptoms show signs of chronic inflammation.
T1D Diagnostic Tests
- T1D diagnosis relies on clinical presentation, fasting plasma glucose (FPG), random plasma glucose (RPG), A1C levels, C-peptide levels, and antibody testing.
T1D Treatment & Management
- Treatment involves insulin therapy delivered via multiple daily injections (MDI) or continuous insulin pump (CIP) with self-monitoring of blood glucose (SMBG) or continuous glucose monitoring (CGM).
- Glucagon injection is used to treat severe hypoglycemia.
- Dietary management plays a crucial role in managing blood glucose levels.
- Correction factor (CF) is used to calculate insulin doses for correcting hyperglycemia.
T1D Complications
- Complications include hyperglycemia, hypoglycemia, diabetic ketoacidosis (DKA), neuropathy, nephropathy, retinopathy, and cardiovascular disease.
- Hyperglycemia occurs when blood glucose > 150 mg/dL.
- Hypoglycemia occurs when blood glucose < 70 mg/dL.
- DKA is a serious condition resulting from high blood glucose and dehydration.
- Neuropathy can cause numbness, tingling, and pain in the extremities.
- Nephropathy is damage to the kidneys.
- Retinopathy is damage to the eyes.
- Cardiovascular disease is a leading cause of death in people with T1D.
T1D Medications
- Amylin (Pramlintide): a synthetic amylin analog used as adjunctive therapy for post-prandial glucose control.
- SGLT1/2 inhibitors: (Dapagliflozin, Empagliflozin) inhibit glucose reabsorption in the kidneys and are used as adjunctive therapy for reducing A1C and FPG/RPG levels.
Insulin Therapy for Special Populations
- Insulin-resistant patients may require higher potency or concentration insulin.
- Pregnant women with T1D require tighter glucose control to prevent complications.
New Treatments & Research
- Novel once-weekly insulins (Icodec and Efsitora) with longer half-lives are being investigated to improve glycemic control with fewer hypoglycemic episodes.
- Teplizumab is a monoclonal antibody approved for delaying T1D onset in individuals with detectable antibodies.
T1D Management Resources
- T1D medical alert ID is essential for patients with T1D.
- Regular monitoring of blood glucose, A1C levels, and neuro/podiatry checks are vital for managing T1D.
- Appropriate supplies for insulin delivery, blood glucose monitoring, and treatment of hypoglycemia are crucial for managing T1D.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.