Podcast
Questions and Answers
ما هي الوحدة الوظيفية الأساسية للكبد؟
ما هي الوحدة الوظيفية الأساسية للكبد؟
- قناة الصفراء
- الوريد الكبدي الأيمن
- الفصيص الكبدي (correct)
- الشريان الكبدي
كم عدد الفصائص الموجودة في كبد الإنسان؟
كم عدد الفصائص الموجودة في كبد الإنسان؟
- 155 - 50 ألف فصيص (correct)
- 300 - 200 ألف فصيص
- 200 - 100 ألف فصيص
- 75 - 10 ألف فصيص
أي الأوردة التالية هي إحدى الأوردة الكبدية الرئيسية؟
أي الأوردة التالية هي إحدى الأوردة الكبدية الرئيسية؟
- الوريد الكبدي الأيمن (correct)
- الوريد العميق
- الوريد الرئوي
- الوريد الركبي
ما هو الشكل الذي يتشكل حوله الفصيص الكبدي؟
ما هو الشكل الذي يتشكل حوله الفصيص الكبدي؟
إلى أين تصب الأوردة الكبدية؟
إلى أين تصب الأوردة الكبدية؟
ما الذي يميز الفص المدنب في الكبد؟
ما الذي يميز الفص المدنب في الكبد؟
كم عدد الأوردة الكبدية الرئيسية؟
كم عدد الأوردة الكبدية الرئيسية؟
ما هو المسؤول الرئيسي عن تصريف الدم من الفصوص الكبدية؟
ما هو المسؤول الرئيسي عن تصريف الدم من الفصوص الكبدية؟
أي من المستويات التالية يمكن أن تؤثر على وظيفة الكبد؟
أي من المستويات التالية يمكن أن تؤثر على وظيفة الكبد؟
Flashcards
الفصيص الكبدي
الفصيص الكبدي
الوحدة الوظيفية الأساسية للكبد، شكلها مضلّع.
عدد الفصوص في الكبد
عدد الفصوص في الكبد
يحتوي كبد الإنسان على 155- 200 ألف فصيص.
الوريد المركزي
الوريد المركزي
الوعاء الدموي الذي يتشكل حوله الفصيص الكبدي.
الأوردة الكبدية
الأوردة الكبدية
Signup and view all the flashcards
الوريد الأجوف السفلي
الوريد الأجوف السفلي
Signup and view all the flashcards
الفص المذنب
الفص المذنب
Signup and view all the flashcards
الأوردة الكبدية (فوق الكبد)
الأوردة الكبدية (فوق الكبد)
Signup and view all the flashcards
الدماغ الكبدي
الدماغ الكبدي
Signup and view all the flashcards
الجزء خلف الكبد
الجزء خلف الكبد
Signup and view all the flashcards
Study Notes
Functional Anatomy of the Liver (Lecture 2)
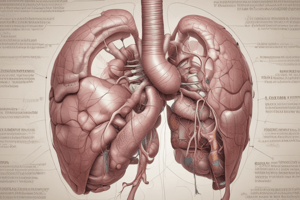
- The basic functional unit of the liver is the hepatic lobule, a polygonal structure.
- A human liver contains 50,000 to 100,000 lobules.
- The lobule is structured around a central vein, which flows into hepatic veins.
- There are three major hepatic veins: right, middle, and left.
- These drain into the inferior vena cava.
- The caudate lobe has small, independent hepatic veins that drain directly into the inferior vena cava.
- It also lacks a specific bile duct.
- The lobule is comprised of plates of hepatocytes radiating from the central vein like spokes of a bicycle wheel.
- Interstitial spaces between adjacent plates are vascular expansions called hepatic sinusoids.
- Each plate consists of two opposing bands of hepatocytes.
- Fine bile canaliculi are located between the opposing hepatocytes, emptying into bile ducts in the interlobular septa.
- Interlobular septa house branches of the hepatic portal vein (portal venules), which empty into the sinusoids situated between hepatocyte plates.
- This allows direct contact of hepatocytes with portal vein blood.
- Interlobular septa also contain branches of the hepatic artery (hepatic arterioles) that also empty into the sinusoids, but not in the septa itself, distant from the portal venules.
Hepatic Sinusoids Lining
- Hepatic sinusoids are lined by two types of cells.
- Adjacent endothelial cells have wide pores that can reach up to 1 micron in diameter.
- The space between the endothelial cells and the opposing hepatocytes is called Disse's spaces.
- The wide pores between the endothelial cells allow plasma and its components, including large proteins, to freely enter Disse's spaces.
- Disse's spaces connect to lymphatic vessels in the interlobular septa to drain excess fluid.
- Kupffer cells (also called reticulo-endothelial cells) are large phagocytes that engulf aged red blood cells, germs, and foreign substances in the sinusoids.
Liver Physiology
- The liver performs a vast array of functions involving thousands of chemical reactions.
- Absorbed substances go directly to the liver for storage or conversion into usable forms.
- Basic liver functions can be grouped into:
- Hemodynamic: blood storage and filtration.
- Metabolic: relating to most metabolic systems in the body.
- Excretory/secretory: bile formation and secretion into the digestive tract.
Hepatic Hemodynamics
- The portal vein transports approximately 1100 mL of blood per minute to hepatic sinusoids.
- The hepatic artery adds 350 mL per minute, summing to 1450 mL/minute, or 29% of the normal cardiac output or about one-third of the total blood flow in the body.
- Blood moves from sinusoids to the central vein, hepatic vein, and finally, the inferior vena cava with minimal pressure difference.
- Portal vein pressure at the sinusoids is approximately 9 mmHg, and hepatic vein pressure is approximately 0 mmHg.
- This negligible 9 mmHg pressure difference signifies very low vascular resistance in the hepatic sinusoids.
- Patients with cirrhosis (often caused by alcohol consumption) experience increased resistance due to increased fibrous tissue, obstructing portal blood flow.
- Portal vein flow decreases when a clot forms in the portal vein or its branches.
- When hepatic vein pressure increases (3-7 mmHg) or inferior vena cava pressure increases (10-15 mmHg), significant fluid seeps into the peritoneal cavity (ascites).
- This fluid is primarily plasma, containing 80-90% plasma protein content.
- Portal vein obstruction (and resulting elevated portal venous pressure) can also cause fluid leakage into the abdominal cavity and its formation, but this is less common than ascites resulting from hepatic congestion.
- The normal liver can store significant amounts of blood in its vessels (veins and sinusoids).
- A healthy adult liver accommodates up to 450 mL of blood, constituting 10% of total blood volume.
- Right atrial pressure elevation (due to heart failure) causes peripheral congestion and slows blood return.
- This may cause liver enlargement by storing excess blood (0.5-1 liter).
- The liver serves as a significant blood reservoir.
- Kupffer cells efficiently capture germs that reach the portal vein via the intestinal capillaries.
Metabolic Functions: Carbohydrates
- Simple hexose sugars enter the liver from the intestines through the portal vein.
- The liver's function is to maintain glucose concentrations between 75-95 mg/dL.
- Fructose and galactose are transformed into glucose.
- The liver converts fructose and galactose to glucose via specific enzymes.
- Glucose is the prime product released by the liver into the bloodstream for energy production.
- Glycogenesis: stimulated by insulin.
- Excess glucose is stored as glycogen.
- The liver possesses a high glycogen storage capacity (5-8% of its weight).
- Glycogenolysis: activated by glucagon (during fasting) or adrenaline (during stress).
Metabolic Functions: Fats
- The liver forms triglycerides, phospholipids, and cholesterol.
- Triglycerides are used for energy production.
- The energy produced from them is equivalent to that from carbohydrates.
- Lipolysis, the breakdown of triglycerides into glycerol and fatty acids, is the initial step.
- The liver also synthesizes triglycerides, primarily from carbohydrates, and to a lesser extent, from proteins.
- The liver produces most of the cholesterol and phospholipids in the body.
- Synthesizes lecithin, cephalin, and sphingomyelin, vital components.
Metabolic Functions: Proteins
- Liver plays essential roles in amino acid metabolism.
- It synthesizes plasma proteins (albumin, globulins, and fibrinogen).
- Albumin is the most abundant plasma protein, and its half-life is approximately three weeks.
- The liver is responsible for generating the majority of albumin, fibrinogen, and 75% of alpha & beta globulins.
- Gamma globulins are immunoglobulins produced by B-lymphocytes.
- Protein breakdown involves deamination (removal of the amino group).
- The remaining part of the molecule is oxidized to form pyruvate (used in cellular respiration and energy generation).
- The liver is responsible for urea synthesis to eliminate ammonia toxicity.
- Ammonia buildup occurs in liver failure, potentially leading to hepatic encephalopathy.
Other Metabolic Functions
-
The liver produces clotting factors (factors I, II, V, VII, IX, and X).
-
Vitamin K is essential for the synthesis of some of these factors.
-
Vitamin K deficiency during impaired fat absorption impacts clotting factor production.
-
The liver stores iron in ferritin form (derived from aged/damaged red blood cells).
-
The liver stores vitamins A, E, D, C, B12, and folic acid.
-
The liver plays a crucial role in detoxification, removing exogenous substances (drugs) and endogenous substances (hormones).
-
Detoxification utilizes two methods: conjugation (binding to glucuronic acid or sulfate) and metabolic inactivation (oxidation/reduction/hydroxyl radical addition).
Bile Secretion and Excretion
- The liver secretes bile, a greenish-yellow fluid, composed of water, bile salts, bilirubin, fatty acids, lecithin, cholesterol, and electrolytes (sodium, potassium, calcium, chloride, bicarbonate).
- Bile is important for fat digestion and absorption.
- It also removes waste products (cholesterol, bilirubin breakdown products).
- Bile drains continually from the liver via bile ducts to the common bile duct and eventually the duodenum.
- The gallbladder concentrates bile by reabsorbing water and electrolytes (except calcium).
- Cholecystokinin (CCK) stimulates gallbladder contraction and relaxation of the sphincter of Oddi.
- Fatty meals lead to complete gallbladder emptying within an hour; low-fat meals result in minimal emptying.
Enterohepatic Circulation of Bile Salts
- The terminal ileum reabsorbs approximately 95% of bile salts, which return to the liver via the portal vein.
- Approximately 5% of bile salts are eliminated in feces.
Formation of Gallstones
- Cholesterol insolubility in water is a major factor.
- Cholesterol precipitation in bile forms gallstones.
- Factors contributing to gallstone formation include:
- Excessive water absorption from bile.
- Excessive bile salt and lecithin absorption from bile.
- Excessive cholesterol secretion into bile.
- Inflammation of the gallbladder lining.
Bilirubin Excretion
- Bilirubin, a byproduct of heme (hemoglobin breakdown), is initially released as unconjugated bilirubin.
- This is transported as an albumin complex in the blood.
- Through hepatic uptake, the liver converts unconjugated bilirubin to conjugated bilirubin, a form soluble in water for excretion with bile.
- Conjugated bilirubin is released with bile.
- Elevated bilirubin levels in blood lead to jaundice.
- Two major forms of jaundice are characterized by elevated unconjugated (hemolytic) and conjugated (obstructive) bilirubin levels.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.