Podcast
Questions and Answers
During thyroid gland development, from which embryonic structure does the majority of the gland originate?
During thyroid gland development, from which embryonic structure does the majority of the gland originate?
- Ultimobranchial body
- Thyroglossal duct (correct)
- Neural crest cells
- Pharyngeal pouches
What is the most likely cause of a thyroglossal duct cyst?
What is the most likely cause of a thyroglossal duct cyst?
- Failure of the thyroglossal duct to descend properly
- Inflammation of the thyroid gland in utero
- Persistence of the thyroglossal duct (correct)
- Excessive production of thyroid hormones during development
Where is the foramen cecum located, relative to the adult thyroid gland?
Where is the foramen cecum located, relative to the adult thyroid gland?
- Inferior to the inferior pole of the thyroid gland
- Indicated by the cranial end of the thyroglossal duct at the tongue (correct)
- Superior to the superior pole of the thyroid gland
- Posterior to the thyroid gland
Which cells are derived from the ultimobranchial body?
Which cells are derived from the ultimobranchial body?
Why is the body of the hyoid bone sometimes removed during surgical removal of a thyroglossal duct cyst?
Why is the body of the hyoid bone sometimes removed during surgical removal of a thyroglossal duct cyst?
At what vertebral level does the base of each thyroid lobe typically lie?
At what vertebral level does the base of each thyroid lobe typically lie?
What is the clinical significance of the suspensory ligament of Berry during thyroid surgery?
What is the clinical significance of the suspensory ligament of Berry during thyroid surgery?
Which anatomical structure is contained within the carotid sheath?
Which anatomical structure is contained within the carotid sheath?
What is the most likely consequence of injuring the left and right inferior thyroid veins during a tracheostomy?
What is the most likely consequence of injuring the left and right inferior thyroid veins during a tracheostomy?
Why is it safer to tie the inferior thyroid artery away from the lower pole of the thyroid gland during a thyroidectomy?
Why is it safer to tie the inferior thyroid artery away from the lower pole of the thyroid gland during a thyroidectomy?
Which arteries primarily supply the thyroid gland?
Which arteries primarily supply the thyroid gland?
Where does the superior thyroid vein typically drain?
Where does the superior thyroid vein typically drain?
During a nuclear scan of the thyroid, what does a 'cold spot' indicate?
During a nuclear scan of the thyroid, what does a 'cold spot' indicate?
What is a key characteristic of a goiter upon physical examination?
What is a key characteristic of a goiter upon physical examination?
What is the function of follicular cells in the thyroid?
What is the function of follicular cells in the thyroid?
A patient presents with a midline neck swelling that moves with swallowing. Surgical removal of the swelling also involves removal of the hyoid bone. What embryological structure is most likely implicated in this scenario?
A patient presents with a midline neck swelling that moves with swallowing. Surgical removal of the swelling also involves removal of the hyoid bone. What embryological structure is most likely implicated in this scenario?
A surgeon is performing a thyroidectomy and identifies a fibromuscular band connecting the pyramidal lobe to the hyoid bone. Injury to what structure is most likely to cause retraction of the gland superiorly?
A surgeon is performing a thyroidectomy and identifies a fibromuscular band connecting the pyramidal lobe to the hyoid bone. Injury to what structure is most likely to cause retraction of the gland superiorly?
Following a thyroidectomy, a patient develops hoarseness. Further examination reveals damage to a nerve closely associated with the suspensory ligament of Berry. Which nerve is most likely affected?
Following a thyroidectomy, a patient develops hoarseness. Further examination reveals damage to a nerve closely associated with the suspensory ligament of Berry. Which nerve is most likely affected?
During a thyroid surgery, a surgeon encounters an enlarged thyroid gland extending downwards into the superior mediastinum. What anatomical structure is most likely arresting the upward shift of the thyroid gland?
During a thyroid surgery, a surgeon encounters an enlarged thyroid gland extending downwards into the superior mediastinum. What anatomical structure is most likely arresting the upward shift of the thyroid gland?
A surgeon is about to perform a tracheostomy. Understanding the vascular relations of the thyroid isthmus is crucial to avoid complications. From superficial to deep, which layers must a surgeon traverse anterior to the trachea to reach the isthmus?
A surgeon is about to perform a tracheostomy. Understanding the vascular relations of the thyroid isthmus is crucial to avoid complications. From superficial to deep, which layers must a surgeon traverse anterior to the trachea to reach the isthmus?
During a thyroidectomy, the surgeon needs to ligate the superior thyroid artery. To minimize the risk of damaging the external laryngeal nerve, where is the safest location to perform the ligation?
During a thyroidectomy, the surgeon needs to ligate the superior thyroid artery. To minimize the risk of damaging the external laryngeal nerve, where is the safest location to perform the ligation?
A patient undergoing thyroid surgery experiences injury to the venous plexus lying deep to the true capsule of the thyroid gland. What is the most likely immediate consequence of this injury?
A patient undergoing thyroid surgery experiences injury to the venous plexus lying deep to the true capsule of the thyroid gland. What is the most likely immediate consequence of this injury?
A surgeon is operating near the inferior pole of the thyroid gland and needs to ligate the inferior thyroid artery. What anatomical relationship should the surgeon be aware of to avoid complications?
A surgeon is operating near the inferior pole of the thyroid gland and needs to ligate the inferior thyroid artery. What anatomical relationship should the surgeon be aware of to avoid complications?
During a surgical procedure involving the thyroid gland, the ascending branch of the inferior thyroid artery is carefully preserved. What anatomical structures receive their main blood supply from this arterial branch?
During a surgical procedure involving the thyroid gland, the ascending branch of the inferior thyroid artery is carefully preserved. What anatomical structures receive their main blood supply from this arterial branch?
A patient presents with hoarseness following a thyroidectomy. What is the most likely cause of this complication, considering the anatomical relations of the thyroid?
A patient presents with hoarseness following a thyroidectomy. What is the most likely cause of this complication, considering the anatomical relations of the thyroid?
A surgeon is resecting the thyroid gland and identifies Kocher's vein. Where does this vein typically drain into?
A surgeon is resecting the thyroid gland and identifies Kocher's vein. Where does this vein typically drain into?
A patient with papillary thyroid carcinoma shows normal thyroid appearance on examination, but enlarged deep cervical lymph nodes are found to contain thyroid tissue. What explains this?
A patient with papillary thyroid carcinoma shows normal thyroid appearance on examination, but enlarged deep cervical lymph nodes are found to contain thyroid tissue. What explains this?
A patient presents with compression symptoms from a goiter, including difficulty swallowing and shortness of breath. What respective structures are primarily affected to cause each of these symptoms?
A patient presents with compression symptoms from a goiter, including difficulty swallowing and shortness of breath. What respective structures are primarily affected to cause each of these symptoms?
How do thyroid hormones circulate in the blood, and what implications does this have on their biological activity?
How do thyroid hormones circulate in the blood, and what implications does this have on their biological activity?
What is the significance of thyroid peroxidase (TPO) in thyroid hormone synthesis, and how would a deficiency impact hormone production?
What is the significance of thyroid peroxidase (TPO) in thyroid hormone synthesis, and how would a deficiency impact hormone production?
Flashcards
Origin of the thyroid gland
Origin of the thyroid gland
Thyroglossal duct & Ultimobranchial body. Starts functioning from the 4th month of intrauterine life.
Follicular cell origin
Follicular cell origin
The lower end of the thyroglossal duct gives rise to the follicular cells of the thyroid gland.
Ultimobranchial body Function
Ultimobranchial body Function
It joins the lower end of the thyroglossal duct and gives rise to parafollicular cells.
Cause of ectopic thyroid
Cause of ectopic thyroid
Signup and view all the flashcards
Cause of thyroglossal cyst
Cause of thyroglossal cyst
Signup and view all the flashcards
Thyroid gland location and weight
Thyroid gland location and weight
Signup and view all the flashcards
Isthmus Function
Isthmus Function
Signup and view all the flashcards
Apex of each lobe Location
Apex of each lobe Location
Signup and view all the flashcards
Function of the False Capsule
Function of the False Capsule
Signup and view all the flashcards
Function of Suspensory Ligament of Berry
Function of Suspensory Ligament of Berry
Signup and view all the flashcards
Function of the Anterior border
Function of the Anterior border
Signup and view all the flashcards
Thyroid Stimulating Antibodies
Thyroid Stimulating Antibodies
Signup and view all the flashcards
Thyroid follicles
Thyroid follicles
Signup and view all the flashcards
Follicular cells
Follicular cells
Signup and view all the flashcards
Parafollicular cells
Parafollicular cells
Signup and view all the flashcards
Thyroglossal duct origin
Thyroglossal duct origin
Signup and view all the flashcards
Pyramidal lobe
Pyramidal lobe
Signup and view all the flashcards
Levator glandulae thyroideae
Levator glandulae thyroideae
Signup and view all the flashcards
Thyroglossal cyst location
Thyroglossal cyst location
Signup and view all the flashcards
Thyroid gland parts
Thyroid gland parts
Signup and view all the flashcards
The base of each lobe Location
The base of each lobe Location
Signup and view all the flashcards
True Capsule (Fibrous)
True Capsule (Fibrous)
Signup and view all the flashcards
Function of the Posterior border
Function of the Posterior border
Signup and view all the flashcards
Lobe location (left & right)
Lobe location (left & right)
Signup and view all the flashcards
Isthmus Location
Isthmus Location
Signup and view all the flashcards
Iodide Trapping
Iodide Trapping
Signup and view all the flashcards
Oxidation process
Oxidation process
Signup and view all the flashcards
Goiter
Goiter
Signup and view all the flashcards
Study Notes
- The thyroid gland comes from the thyroglossal duct and the ultimobranchial body
- Function begins during the 4th month of intrauterine life
Thyroglossal Duct
- Originates from the endoderm of the embryonic pharynx at the foramen cecum
- Starts at the foramen caecum
- Travels midline anterior to the hyoid bone
- Curves posterior to the hyoid bone
- Proceeds down the front of the thyroid and cricoid cartilage
- The cranial end location is indicated by the foramen cecum of the tongue
Fate of the cranial end
- May remain as:
- Pyramidal lobe that extends from the isthmus
- Levator glandulae thyroideae which is a fibromuscular band that connects the pyramidal lobe to the hyoid bone
- The lower end gives rise to the follicular cells of the thyroid gland
- The rest of the duct obliterates
Ultimobranchial Body
- Joins the lower end of the thyroglossal duct
- Gives rise to parafollicular cells
Congenital Anomalies
- Ectopic thyroid results from the thyroglossal duct failing to descend
- Thyroglossal cyst results from persistence of the thyroglossal duct
- With thyroglossal cysts, a Midline swelling is present in the neck near the hyoid bone, which is sometimes removed to prevent recurrence
- Lingual thyroid: Gland remains on the dorsum of the tongue
- When the cyst breaks through the skin it creates a thyroglossal fistula which is never congenial
Surgical Anatomy General
- Located in the lower front of the neck
- Weighs about 25 grams in adults, slightly heavier in females
- The vertebral level of the thyroid is at C5-T1
- It has two lateral lobes (right and left), which connect to the trachea via the isthmus, and a small pyramidal lobe
Extent of lobes
- Apex lies opposite the oblique line of the thyroid cartilage
- The base is at the level of the 5th or 6th tracheal ring
- Vertebral level is C5 to T1
- Against the level from the 2nd to (3rd or 4th) tracheal rings
- Pyramidal lobe is on the left side of the upper margin of isthmus
- Pyramidal lobe may connect to hyoid bone via levator glandulae thyroideae ms
- Has a true capsule (fibrous) and a false capsule (fascial)
Clinical Correlation
- Enlarged thyroid glands shift downward instead of upward
- Upward shift is stopped by the attachment of the sternothyroid muscle
- Downward shift occurs when short neck and strong strap muscles push the enlarged gland downward into the superior mediastinum (retrosternal goiter)
Thyroid Capsule
- True capsule: completely surrounds the gland, derived from the connective tissue at the periphery, and the venous plexus lies deep to it
- During surgical removal of the gland care is taken to remove the gland along with its true capsule to avoid injury to venous plexus
- False capsule: derived from the pretracheal layer of deep cervical fascia
Pretracheal Fascia attachment
- Superiorly: to the oblique line of the thyroid cartilage
- Laterally: continuous with the deep cervical fascia
- Inferiorly: continuous with the fibrous pericardium
- Importance: Responsible for movement of the thyroid gland up with swallowing
Pretracheal Fascia Clinical Correlation
- Movements of the thyroid during swallowing (deglutition) & speech
- Retrosternal extension
- Compression manifestation of huge goitre
- Suspensory ligament of Berry: a thickening of pretracheal fascia
- Site: Posteromedial aspect of thyroid gland lobe & cricoid cartilage
- Importance: Secures the gland to the larynx preventing downward movement and during surgical removal of the enlarged gland the recurrent laryngeal nerve (RLN) lies behind it & it is liable to injury during operation
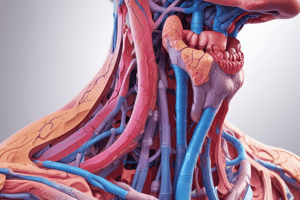
Relations of Lobes
- Each lobe of the thyroid gland have the following:
- Three surfaces: Superficial (anterolateral), Medial, Posterior (posterolateral)
- Two boarders: Anterior, Posterior
- Two poles: Superior "apex", Inferior "base"
Relations of surfaces
- Superficial Surface: Infrahyoid muscles: Sternothyroid, Sternohyoid, Omohyoid "Superior belly", laterally covered by the anterior margin of Sternomastoid
- Medial Surface:
- Two Tubes: Larynx & Pharynx above, Trachea & Esophagus below
- Two Muscles: Inferior constrictor, Cricothyroid
- Two Cartilages: Cricoid, Thyroid
- Two Nerves: External laryngeal, Recurrent laryngeal
Recurrent laryngeal nerve
- Passes upwards in the groove between the trachea and esophagus
- Lies immediately behind the cricothyroid joint and the ligament of Berry
- Posterior Relations: Carotid sheath (Vagus nerve - Carotid artery - Internal jugular vein), sympathetic chain "behind the carotid sheath", prevertebral fascia & longus colli. "directly behind", and on left side, the lower pole may be related to arch of thoracic duct
Relations of boarders
- Anterior Boarder is related to: The anterior branch of the superior thyroid artery
- Posterior Boarder is related to: The parathyroid glands and the anastomosis between the superior & inferior thyroid arteries
Relations of the Isthmus
- Anteriorly: Covered from within outwards by pretracheal fascia, strap muscles, investing layer of deep fascia, superficial fascia with anterior jugular veins, and the skin
- Posteriorly: It sits on the 2nd to (3rd or 4th) tracheal rings
- Upper margin: Terminal parts of anterior branches of both superior thyroid arteries
- Lower margin: Inferior thyroid veins emerge and the thyroidea ima (when present) enters
Relations of poles
- Superior Pole "Apex": limited by the insertion of thyrohyoid muscle to thyroid cartilage and related to the superior thyroid artery and the external laryngeal nerve
- Inferior Pole "Base": Related to the inferior thyroid artery, the recurrent laryngeal nerve, and the arch of the thoracic duct is on the left side
Surface Anatomy
- Lobes (Left & Right):
- Site: In the anterior triangles in the lower neck, and inferior to the position of the oblique line of the thyroid cartilage
- Relation to sternothyroid: Sternothyroid at arches superiorly to the oblique lines & lies anterior to the lobes of the thyroid gland
- Prevents the upward movement of the lobes
- Palpation of the lobes: By finding the thyroid prominence & arch of the cricoid cartilage, then feeling posterolateral to the larynx
- Isthmus:
- Site: Crosses anterior to the upper end of the trachea
- Palpation of the isthmus: In the midline inferior to the arch of the cricoid
Isthmus Clinical Importance
- Presence of the thyroid Isthmus & the associated vessels crossing the midline
- Makes tracheal cartilage palpation difficult
- Complicates anterior airway entry during surger tracheostomy
Venous drainage
- Thyroid veins do not accompany the thyroid arteries
- 3 Pairs of veins arise from venous plexus that lies deep to the true capsule
- Superior thyroid vein from the upper pole on each side drains into the corresponding internal jugular vein
- Middle thyroid vein (very short) which corresponds to the lobe and corresponding Internal jugular vein
- Inferior thyroid vein from the lower margin of Isthmus drains on the anterior surface of trachea, right and left drain into left innominate (brachio-cephalic) vein, sometimes each vein may drain into respective brachio-cephalic veins
- Right and left inferior thyroid veins connect before trachea, their injury causes bleeding in tracheostomy
- Occasionally Kocher's vein "Another vein may be present", site is between the inferior & middle thyroid veins, and opens into the internal jugular vein
Arterial Supply
- Pairs of superior and inferior thyroid arteries
- The thyroidea ima
- The accessory thyroid arteries
Superior thyroid arteries
- Arises from the external carotid artery
- Descends to the superior pole of the lateral lobe of the gland, “Accompanying the external laryngeal nerve”, and enters the gland at the upper pole
- The upper pole is the safest site for tying the superior thyroid artery during thyroidectomy
Inferior thyroid arteries
- Arises from the thyrocervical trunk of the 1st part of the subclavian artery
- Forms a loop with upward convexity to sixth cervical vertebra
- Descends to reach the base of the lateral lobe of the gland
- Enters the lower pole of the gland "Where it is very close to the recurrent laryngeal nerve"
- Safer to tie the inferior thyroid artery as away from the lower pole of the gland as possible during thyroidectomy
Vascular Supply
- Inferior thyroid artery's ascending branch joins superior thyroid artery's descending branch at gland's posterior margin
- Ascending branch of inferior thyroid artery is preserved during ligation as it is the main supply to parathyroid glands
- The Thyroidea Ima (Not Always Present): Comes from arch of aorta (or) Brachiocephalic trunk then ascends in front of the trachea & enters the isthmus.
- The Accessory Thyroid Arteries: Comes from twigs from Esophageal & Tracheal branches of inferior thyroid arteries
Lymphatics (lymph from upper and lower parts)
- Lymph from the upper part from the upper deep cervical nodes (jugulo-digastric) and directly from the prelaryngeal nodes
- Lymph from the lower part from the lower deep cervical group (jugulo-omohyoid) and directly through the pretracheal (delphic) & paratracheal nodes
- A few lymph vessels may drain into brachiocephalic nodes in the superior mediastinum, while others may directly reach the thoracic duct
- Lymphatic spread of papillary carcinoma of the thyroid gland manifests in an interesting way; The thyroid gland looks normal but the deep cervical LNs of the jugular chain is enlarged & contains thyroid tissue
Nuclear Scan of Thyroid Gland
- Used to study the function of the thyroid gland by isotope scanning steps
- Radioactive iodine (131I) is given orally
- Photographs of thyroid gland are taken
- Hot spots indicate hyperactive areas
- Cold spots indicate hypoactive areas
- Thyroid scans find ectopic thyroid tissue outside the neck (lingual or retrosternal)
Pathology: Goiter
- General Characteristics: Abnormal enlargement of the thyroid gland, a common cause of a midline swelling in the neck, thyroid swelling moves with deglutition, may present as a smooth swelling or a nodular swelling
- One of the complications is Pressure Effects and varies depending on structure or structures compressed, structures compressed anatomical relations
Pressure Effects Caused by Goiter
- Trachea → Dyspnea (shortness of breath)
- Esophagus → Dysphagia (difficulty in swallowing)
- Recurrent laryngeal nerve → Hoarseness of voice
- Carotid sheath → Posterior displacement
- Sympathetic chain → Horner's syndrome
B) Thyroid Stimulating Antibodies
- A family of IgG immunoglobulins, collectively known as Thyroid Stimulating Antibodies (TsAB)
- Activates the TSH receptors on the follicular cell membrane
- More protracted action than TSH (TsAB = 16 - 24 hours vs TSH = 1.5 - 3 hours)
- Responsible for almost all cases of thyrotoxicosis ("Which is not due to autonomous toxic nodules")
- Serum concentrations are very low & not routinely measured
Histological Structure (Thyroid Follicles)
- It is the structural & functional unit of the thyroid gland and made of about 30 million units
- General Characteristics
- Number is about 30 million
- Size 0.05 - 0.5 mm
- Shape rounded or oval and filled with colloid (Thyroglobulin)
- Wall lined by low cubical epithelial cells
Types of Cells Lining the Follicles
- Follicular cells which make up 98% and are responsible for synthesis & secretion of thyroid hormones
- Parafollicular cells (C-cells, clear cells, or light cells) which make up 2% and secrete calcitonin hormone which causes reduced serum calcium level
Physiology (Thyroid Hormones Synthesis)
- Main hormones secreted are T3 and T4 and their synthesis is controlled by several enzymes
- Steps:
- Trapping of inorganic Iodide from the blood by the thyroid gland
- Oxidation by thyroid peroxidase enzyme (TPO), Iodide → lodine
- Binding of iodine to Tyrosine to form Mono-iodotyrosine (MIT), Di-iodotyrosine (DIT)
- Di + Di → T4 (Tetra iodothyronine), Mono + Di → T3 (Tri iodothyronine), coupling occurs within the thyroglobulin molecule
- Under TSH control
- Complex is resorbed into the cell
- Thyroglobulin is broken down into T3 & T4 & liberated into blood
- Thyroid hormones circulate in 2 forms
- Protein bound which is mainly Thyroxin Binding Globulin (TBG) and is 99% of the bounded part
- Free part which is in equilibrium with the protein bound hormone and is the active part which is less than 1% Bounded
- Peripheral conversion: part of T4 can be converted to T3 in the peripheral tissue and as T3 it is more important & quick acting (within a few hours) whereas T4 acts more slowly (4-14 days)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.