Podcast
Questions and Answers
What is the most common cause of elevated SHBG?
What is the most common cause of elevated SHBG?
- Androgenic steroids
- Aging (correct)
- Hypothyroidism
- HIV infection
What condition is associated with low testosterone and high LH+FSH?
What condition is associated with low testosterone and high LH+FSH?
- Prostate cancer
- Secondary Hypogonadism (correct)
- Klinefelter Syndrome
- Hypothyroidism
What is the most common cause of gynecomastia during puberty?
What is the most common cause of gynecomastia during puberty?
- Idiopathic (correct)
- Hypogonadism
- Hyperthyroidism
- Testicular tumor
What is the main investigation for gynecomastia?
What is the main investigation for gynecomastia?
What is the primary site of testosterone production in men?
What is the primary site of testosterone production in men?
What is the main cause of gynecomastia in chronic renal insufficiency?
What is the main cause of gynecomastia in chronic renal insufficiency?
What is the most common cause of low SHBG?
What is the most common cause of low SHBG?
What is the primary treatment for persistent pubertal gynecomastia?
What is the primary treatment for persistent pubertal gynecomastia?
What is the main cause of elevated SHBG in moderate obesity?
What is the main cause of elevated SHBG in moderate obesity?
What is the most common cause of primary hypogonadism?
What is the most common cause of primary hypogonadism?
What is synthesized by Sertoli cells in the seminiferous tubules?
What is synthesized by Sertoli cells in the seminiferous tubules?
Which cells in the testes produce Testosterone?
Which cells in the testes produce Testosterone?
What is involved in the release of Testosterone?
What is involved in the release of Testosterone?
Which hormone is involved in spermatogenesis?
Which hormone is involved in spermatogenesis?
What type of secretion does GnRH exhibit?
What type of secretion does GnRH exhibit?
What is synthesized by Leydig cells?
What is synthesized by Leydig cells?
What is the primary role of FSH?
What is the primary role of FSH?
Which cells in the seminiferous tubules are involved in sperm production?
Which cells in the seminiferous tubules are involved in sperm production?
What do Leydig cells produce?
What do Leydig cells produce?
What is the function of inhibin B?
What is the function of inhibin B?
What is the primary source of testosterone production in normal young men?
What is the primary source of testosterone production in normal young men?
What percentage of testosterone is present as free hormone in the blood?
What percentage of testosterone is present as free hormone in the blood?
What is the primary hormone to which androgen target cells convert testosterone before binding to the androgen receptor?
What is the primary hormone to which androgen target cells convert testosterone before binding to the androgen receptor?
How is primary hypogonadism characterized?
How is primary hypogonadism characterized?
What is a suggested condition for screening male hypogonadism?
What is a suggested condition for screening male hypogonadism?
Which investigation is recommended for diagnosing male hypogonadism?
Which investigation is recommended for diagnosing male hypogonadism?
What is the recommended focus for screening male hypogonadism?
What is the recommended focus for screening male hypogonadism?
What do guidelines recommend for initial morning total testosterone levels?
What do guidelines recommend for initial morning total testosterone levels?
What is the definition of male hypogonadism?
What is the definition of male hypogonadism?
What is the primary source of testosterone in both men and women?
What is the primary source of testosterone in both men and women?
What percentage of testosterone is present as free hormone in the blood?
What percentage of testosterone is present as free hormone in the blood?
Where is testosterone primarily secreted from in both men and women?
Where is testosterone primarily secreted from in both men and women?
What is the primary source of testosterone production in a normal young man?
What is the primary source of testosterone production in a normal young man?
Which hormone is the key hormone required for the actions of testosterone in the body?
Which hormone is the key hormone required for the actions of testosterone in the body?
What is the primary protein to which testosterone is bound in the blood?
What is the primary protein to which testosterone is bound in the blood?
In a normal young man, how much testosterone is made each day?
In a normal young man, how much testosterone is made each day?
What is a potential indicator of testosterone deficiency?
What is a potential indicator of testosterone deficiency?
Which condition is NOT associated with an increased risk of testosterone deficiency?
Which condition is NOT associated with an increased risk of testosterone deficiency?
What symptoms can overlap between testosterone deficiency and depressive symptoms?
What symptoms can overlap between testosterone deficiency and depressive symptoms?
What can small testicles lead to?
What can small testicles lead to?
What can long-term opioid use do to the pituitary axis?
What can long-term opioid use do to the pituitary axis?
What is a potential consequence of prolonged testosterone deficiency?
What is a potential consequence of prolonged testosterone deficiency?
Which of the following is a primary cause of male hypogonadism?
Which of the following is a primary cause of male hypogonadism?
What are the clinical features of hypogonadism?
What are the clinical features of hypogonadism?
Which condition can be a sign of imbalanced testosterone and estrogen in hypogonadism?
Which condition can be a sign of imbalanced testosterone and estrogen in hypogonadism?
What can hypogonadism lead to apart from erectile dysfunction and reduced sex drive?
What can hypogonadism lead to apart from erectile dysfunction and reduced sex drive?
Which type of hypogonadism results from issues in the hypothalamus or pituitary?
Which type of hypogonadism results from issues in the hypothalamus or pituitary?
What is crucial for diagnosing and managing male hypogonadism?
What is crucial for diagnosing and managing male hypogonadism?
In the assessment of testosterone levels, what is the impact of nutritional deficiencies on hypothalamic pituitary suppression and testosterone levels?
In the assessment of testosterone levels, what is the impact of nutritional deficiencies on hypothalamic pituitary suppression and testosterone levels?
What should be considered in the assessment of testosterone levels regarding family history?
What should be considered in the assessment of testosterone levels regarding family history?
What is the potential impact of major life events on testosterone deficiency?
What is the potential impact of major life events on testosterone deficiency?
What is the significance of inquiring about recent changes in the body, such as gynaecomastia or testicle problems, in the assessment of testosterone levels?
What is the significance of inquiring about recent changes in the body, such as gynaecomastia or testicle problems, in the assessment of testosterone levels?
What is the consideration regarding starting testosterone therapy after investigations?
What is the consideration regarding starting testosterone therapy after investigations?
What is the impact of medications on testosterone levels?
What is the impact of medications on testosterone levels?
Which enzyme is responsible for the conversion of testosterone to dihydrotestosterone (DHT)?
Which enzyme is responsible for the conversion of testosterone to dihydrotestosterone (DHT)?
What is the primary hormone involved in the pulsatile secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH)?
What is the primary hormone involved in the pulsatile secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH)?
Which hormone is a concern for those taking excess androgens due to its aromatization from testosterone?
Which hormone is a concern for those taking excess androgens due to its aromatization from testosterone?
What is the primary hormone responsible for the increased risk of myocardial infarction due to its impact on cholesterol levels?
What is the primary hormone responsible for the increased risk of myocardial infarction due to its impact on cholesterol levels?
Which hormone has a role in the development of reproductive organs in the fetus?
Which hormone has a role in the development of reproductive organs in the fetus?
What is the primary hormone responsible for the impact on cholesterol levels and its association with increased risk of myocardial infarction?
What is the primary hormone responsible for the impact on cholesterol levels and its association with increased risk of myocardial infarction?
Study Notes
Understanding Testosterone and Male Hypogonadism
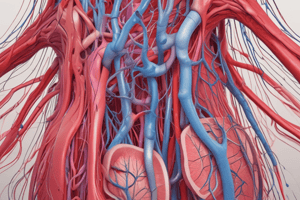
- Testosterone is a steroid hormone secreted in both men and women from the testes, ovary, and adrenal glands, with normal young men producing about 7 mg each day, primarily from the testes.
- In blood, testosterone is predominantly bound to plasma proteins, with less than 5% derived from adrenal secretions and only about 2% present as free hormone.
- The synthesis of androgens involves the conversion of cholesterol to various intermediates, ultimately leading to the production of testosterone and its conversion to dihydrotestosterone (DHT) and estradiol.
- Testosterone, like other steroid hormones, penetrates target cells to stimulate growth and function, with androgen target cells generally converting testosterone to DHT before binding to the androgen receptor.
- Male hypogonadism is defined as the failure of the testes to produce adequate testosterone, leading to a decrease in sperm production or testosterone production, and can be caused by primary (testicular) or secondary (hypothalamic or pituitary) factors.
- Primary hypogonadism is characterized by low testosterone and elevated serum LH and/or FSH, while secondary hypogonadism features low testosterone and normal or low serum LH and/or FSH.
- Causes of male hypogonadism include genetic disorders, infections, trauma, tumors, medications, and systemic illnesses, with clinical features ranging from incomplete sexual development to decreased libido and infertility.
- Screening for male hypogonadism is suggested in conditions such as pituitary mass, medication use affecting testosterone production, HIV-associated weight loss, and infertility, with a focus on history, physical examination, and investigations including hormone levels, semen analysis, and imaging.
- Key investigations for male hypogonadism include serum testosterone, LH/FSH, SHBG, liver function tests, semen analysis, karyotyping, pituitary function testing, and DEXA scan for bone density.
- Guidelines on screening for male hypogonadism recommend initial morning total testosterone levels, with consideration of age-dependent normal ranges and exclusion of reversible causes before diagnosis and follow-up.
- The text provides a comprehensive overview of the synthesis, action, regulation, and clinical aspects of testosterone, as well as the diagnosis and management of male hypogonadism.
- The link provided offers further resources on testosterone testing and related information for clinical use.
Understanding Testosterone and its Effects
- The testicle contains sertoli cells that produce anti-mullerian hormone (AMH) and inhibit follicle-stimulating hormone (FSH), and leydig cells that produce testosterone.
- Testosterone synthesis begins with cholesterol, which is converted to pregnenolone, then to progesterone and DHEA, eventually leading to testosterone production.
- Testosterone can be converted to dihydrotestosterone (DHT) or aromatized to estradiol, the latter being a concern for those taking excess androgens.
- The hypothalamic-pituitary-testicular axis involves the pulsatile secretion of luteinizing hormone (LH) and FSH, which stimulate testosterone and spermatogenesis production.
- Excess testosterone leads to negative feedback regulation, reducing the production of LH and FSH to prevent further testosterone increase.
- Testosterone can enter cells and be converted to DHT, which has about five times more potency than testosterone, affecting specific induced proteins and resulting in various effects.
- Testosterone has numerous effects, including increased beard growth, prostate growth, laryngeal development, penis size, sperm production, muscle mass, and cholesterol levels.
- Testosterone increases the risk of myocardial infarction due to its impact on cholesterol levels, and it affects sex drive, external genitalia production, and the development of reproductive organs in the fetus.
- Low testosterone levels can lead to depression, fatigue, memory loss, and an increased risk of Alzheimer's disease.
- The effects of testosterone are influenced by its conversion to DHT or estradiol, with potential synergistic or antagonistic effects.
- Testosterone has a wide range of effects on the human body, impacting physical, reproductive, and psychological aspects.
- Understanding the synthesis and effects of testosterone is crucial for comprehending its role in the body and in medical conditions related to hormonal imbalance.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge of testosterone and male hypogonadism with this informative quiz. Explore the synthesis, action, regulation, and clinical aspects of testosterone, and learn about the diagnosis and management of male hypogonadism. Test your understanding of key investigations and guidelines for screening, and enhance your knowledge of this important hormone and its implications for men's health.