Podcast
Questions and Answers
What is Hallux Rigidus?
What is Hallux Rigidus?
Painful, degenerative arthritis of the first metatarsal phalangeal joint
What characterizes Hallux Rigidus?
What characterizes Hallux Rigidus?
Decreased 1st MPJ ROM; specifically dorsiflexion of the 1st MPJ
What is progressively formed in Hallux Rigidus?
What is progressively formed in Hallux Rigidus?
Progressive osteophyte formation
What are the etiologies of hallux rigidus?
What are the etiologies of hallux rigidus?
What is Metatarsus Primus Elevatus?
What is Metatarsus Primus Elevatus?
Greater than _________ distance of 1st met to 2nd met = MPE
Greater than _________ distance of 1st met to 2nd met = MPE
What is the Hallux Interphalangeal Angle?
What is the Hallux Interphalangeal Angle?
What is the normal value of the Hallux Interphalangeal Angle?
What is the normal value of the Hallux Interphalangeal Angle?
Where is pain on palpation with hallux limitus?
Where is pain on palpation with hallux limitus?
What views should be used for radiographic evaluation of hallux rigidus?
What views should be used for radiographic evaluation of hallux rigidus?
What is the dorsal osteophyte sign called?
What is the dorsal osteophyte sign called?
What is the goal of conservative options for hallux rigidus?
What is the goal of conservative options for hallux rigidus?
What are the joint salvage surgery options?
What are the joint salvage surgery options?
What is the indication for Keller Arthroplasty?
What is the indication for Keller Arthroplasty?
What is the fixation used in a 1st MPJ arthrodesis procedure?
What is the fixation used in a 1st MPJ arthrodesis procedure?
What is the fixation and post-op course for joint salvage met osteotomy?
What is the fixation and post-op course for joint salvage met osteotomy?
What is the post-op course for 1st MPJ arthrodesis?
What is the post-op course for 1st MPJ arthrodesis?
Flashcards are hidden until you start studying
Study Notes
Hallux Rigidus Overview
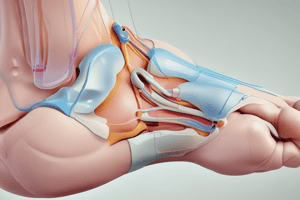
- Hallux Rigidus refers to painful, degenerative arthritis of the first metatarsal phalangeal joint, leading to decreased range of motion, specifically dorsiflexion.
- Characterized by progressive osteophyte formation at the joint.
Etiologies of Hallux Rigidus
- Factors include metatarsal head shape, metatarsus primus elevatus, hallux interphalangeus, hallux valgus deformity, and trauma.
- Additional contributors: pes planus, 1st ray hypermobility, variations in metatarsal length, and metatarsus adductus.
Metatarsus Primus Elevatus
- Defined by the elevation of the first metatarsal compared to the second on lateral radiographs, indicated by more than a 5 mm difference at the distal cortices.
- Results in jamming of the proximal phalanx during dorsiflexion.
Hallux Interphalangeal Angle
- Angle between the longitudinal axes of the proximal and distal phalanges; normal range is 0-10 degrees.
- Increased angle can contribute to stress at the 1st MPJ and exacerbate hallux limitus.
Trauma and Hallux Rigidus
- Can be caused by intra-articular fractures or cumulative minor traumas.
- Pain is typically unilateral and specific to the affected joint.
Pain on Palpation
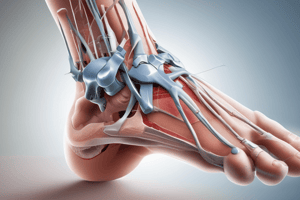
- Palpable pain commonly occurs on the dorsal, medial aspect of the 1st MPJ, under the lesser metatarsal heads, and laterally on the foot.
Radiographic Evaluation
- Requires weight-bearing AP, oblique, and lateral views of the foot.
- Key indicators include osteophytes, loose bodies, joint space narrowing, and metatarsal length and alignment.
Osteophyte Formation
- Identified by the "dorsal flag sign" indicating dorsal osteophyte presence.
Regnauld Classification
- Grade 1: Mild osteophytes, normal joint space.
- Grade 2: Moderate osteophytes and reduced joint space with subchondral changes.
- Grade 3: Severe osteophytes, significant joint space loss, degenerative changes in the hallux-sesamoid complex.
Coughlin & Shurnas Classification
- Grade 1: Dorsal osteophyte with pain at maximum dorsiflexion.
- Grade 2: Osteophytes present with increased pain and reduced motion.
- Grade 3: Narrowed joint space, constant pain at extremes of motion.
- Grade 4: Similar to grade 3, with pain throughout the range of motion.
Conservative Management Options
- Use of hard-soled shoes, orthotics with Morton extension, and rocker-bottom shoes.
- Medications include NSAIDs and potential steroid injections.
- Goal: Pain reduction and limitation of 1st MPJ motion.
Joint Salvage Surgical Options
- Procedures include cheilectomy, phalangeal dorsiflexion osteotomy, and decompression metatarsal osteotomy.
Joint Destructive Surgical Options
- Options include Keller arthroplasty, Valenti arthroplasty, interpositional arthroplasty, implant arthroplasty, and 1st MPJ arthrodesis.
Cheilectomy Procedure
- Involves excision of a third of the dorsal metatarsal head and surrounding osteophytes.
- Indicated for Grades I and II hallux rigidus, aiming for increased dorsiflexion.
Phalangeal Osteotomy
- Bonney-Kessel osteotomy repositions the hallux to decrease jamming, utilizing various fixation techniques.
Metatarsal Osteotomy Techniques
- Includes Watermann, Green-Watermann, Youngswick-Austin, and Lambrinudi techniques aimed at shortening and plantarflexing the 1st metatarsal.
Implant Arthroplasty Indications and Types
- Used for advanced cases, especially Grades 3 or 4; functions as a joint spacer with types including silicone, hemi, and total implants.
1st MPJ Arthrodesis
- Gold standard for end-stage hallux rigidus, indicated when there is <50% cartilage remaining.
- Requires careful positioning of the hallux at 10-15 degrees of dorsiflexion for optimal outcomes.
- Post-operative care involves non-weight bearing for 4-6 weeks to ensure bony fusion.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.