Podcast
Questions and Answers
What is the primary issue with the 1ST MTPJ IMPLANT SYNTHETIC CARTILAGE IMPLANT?
What is the primary issue with the 1ST MTPJ IMPLANT SYNTHETIC CARTILAGE IMPLANT?
- Subsidence is not common
- It does not mimic the modulus of elasticity of cartilage
- It is not suitable for hallux rigidus treatment
- Subsidence is very common (correct)
What is the 'gold standard' for hallux rigidus surgical treatment?
What is the 'gold standard' for hallux rigidus surgical treatment?
- 1st MTPJ implant
- Lapidus procedure
- Synthetic cartilage graft
- 1st MTPJ fusion (correct)
What is the recommended positioning for 1st MTPJ fusion?
What is the recommended positioning for 1st MTPJ fusion?
- Intraoperative loading to determine optimal positioning (correct)
- 20° abducted and 20° dorsiflexed
- 15° abducted and 15° dorsiflexed
- 10° abducted and 10° dorsiflexed
What is the primary benefit of the Lapidus procedure?
What is the primary benefit of the Lapidus procedure?
Why do patients often dislike double fusions (1st MTPJ and 1st TMTJ)?
Why do patients often dislike double fusions (1st MTPJ and 1st TMTJ)?
What is the typical presentation of a patient with hallux rigidus?
What is the typical presentation of a patient with hallux rigidus?
What is the goal of arthrodiastasis in the treatment of hallux rigidus?
What is the goal of arthrodiastasis in the treatment of hallux rigidus?
What is the purpose of penetrating the subchondral plate in chondroplasty?
What is the purpose of penetrating the subchondral plate in chondroplasty?
What is the indication for Valenti resection arthroplasty?
What is the indication for Valenti resection arthroplasty?
What is the Lapidus procedure?
What is the Lapidus procedure?
What is the result of penetrating the subchondral plate in chondroplasty?
What is the result of penetrating the subchondral plate in chondroplasty?
What is the function of the plantar phalangeal base in arthrodiastasis?
What is the function of the plantar phalangeal base in arthrodiastasis?
What is the primary characteristic of Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary characteristic of Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
Which procedure is used to remove osteophytosis from the metatarsal head and proximal phalanx?
Which procedure is used to remove osteophytosis from the metatarsal head and proximal phalanx?
What is the treatment goal for Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the indication for a Kessel & Bonney Decompression osteotomy?
What is the indication for a Kessel & Bonney Decompression osteotomy?
What is the result of drilling subchondral bone in a Cheilectomy procedure?
What is the result of drilling subchondral bone in a Cheilectomy procedure?
What is the primary characteristic of Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary characteristic of Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the purpose of a Youngswick Decompression osteotomy?
What is the purpose of a Youngswick Decompression osteotomy?
What is the consequence of performing a Kessel & Bonney Decompression osteotomy?
What is the consequence of performing a Kessel & Bonney Decompression osteotomy?
What is the primary goal of a Joint-Salvage procedure?
What is the primary goal of a Joint-Salvage procedure?
What is the characteristic of Stage 2 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the characteristic of Stage 2 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary concern when considering 1st MTPJ fusion for a patient who is a smoker?
What is the primary concern when considering 1st MTPJ fusion for a patient who is a smoker?
What is the primary goal of recommending orthotics for a patient with 1st MTPJ arthrosis?
What is the primary goal of recommending orthotics for a patient with 1st MTPJ arthrosis?
What is the likely diagnosis for a patient with no ROM in the 1st MTPJ with forefoot loaded and 50° when unloaded?
What is the likely diagnosis for a patient with no ROM in the 1st MTPJ with forefoot loaded and 50° when unloaded?
What is the primary advantage of arthrodiastasis over chondroplasty in the treatment of hallux rigidus?
What is the primary advantage of arthrodiastasis over chondroplasty in the treatment of hallux rigidus?
What is the primary indication for recommending Gastroc recession?
What is the primary indication for recommending Gastroc recession?
What is the primary difference between Valenti and Keller resection arthroplasty?
What is the primary difference between Valenti and Keller resection arthroplasty?
What is the likely treatment for a patient with Stage 3 1st MTPJ arthrosis who does not want surgery?
What is the likely treatment for a patient with Stage 3 1st MTPJ arthrosis who does not want surgery?
What is the primary concern when considering 1st MTPJ fusion for a patient with a prior bunion surgery?
What is the primary concern when considering 1st MTPJ fusion for a patient with a prior bunion surgery?
Which surgical technique is often considered a joint salvage procedure?
Which surgical technique is often considered a joint salvage procedure?
What is the primary goal of penetrating the subchondral plate in chondroplasty?
What is the primary goal of penetrating the subchondral plate in chondroplasty?
Which technique is used to remove cartilage erosions that are often present in hallux rigidus?
Which technique is used to remove cartilage erosions that are often present in hallux rigidus?
What is the primary benefit of using a mini-rail external fixation in arthrodiastasis?
What is the primary benefit of using a mini-rail external fixation in arthrodiastasis?
What is the primary goal of a Youngswick Decompression osteotomy?
What is the primary goal of a Youngswick Decompression osteotomy?
What is the consequence of performing a Cheilectomy procedure on a deteriorated joint?
What is the consequence of performing a Cheilectomy procedure on a deteriorated joint?
What is the primary benefit of Kessel & Bonney Decompression osteotomy?
What is the primary benefit of Kessel & Bonney Decompression osteotomy?
What is the treatment goal for Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary characteristic of Stage 2 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary characteristic of Stage 2 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the purpose of a Joint-Salvage procedure?
What is the purpose of a Joint-Salvage procedure?
What is the primary goal of a Cheilectomy procedure?
What is the primary goal of a Cheilectomy procedure?
What is the characteristic of Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the characteristic of Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary benefit of a Joint-Salvage procedure?
What is the primary benefit of a Joint-Salvage procedure?
What is the primary purpose of resection arthroplasty in the treatment of hallux rigidus?
What is the primary purpose of resection arthroplasty in the treatment of hallux rigidus?
What is the primary benefit of using a mini-rail external fixation in arthrodiastasis?
What is the primary benefit of using a mini-rail external fixation in arthrodiastasis?
What is the primary goal of penetrating the subchondral plate in chondroplasty?
What is the primary goal of penetrating the subchondral plate in chondroplasty?
What is the primary difference between Valenti and Keller resection arthroplasty?
What is the primary difference between Valenti and Keller resection arthroplasty?
What is the primary goal of 1st MTPJ arthrodesis?
What is the primary goal of 1st MTPJ arthrodesis?
What is the primary characteristic of Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary characteristic of Stage 1 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for a patient with Stage 1 1st MTPJ arthrosis who does not want surgery?
What is the treatment goal for a patient with Stage 1 1st MTPJ arthrosis who does not want surgery?
What is the likely diagnosis for a patient with a painful 1st MTPJ with forefoot loaded and 50° when unloaded?
What is the likely diagnosis for a patient with a painful 1st MTPJ with forefoot loaded and 50° when unloaded?
What is the recommended treatment for a patient with Stage 3 1st MTPJ arthrosis who is a smoker and does not want surgery?
What is the recommended treatment for a patient with Stage 3 1st MTPJ arthrosis who is a smoker and does not want surgery?
What is the next step in treatment for a patient with Stage 2 1st MTPJ arthrosis who has already undergone bunion surgery?
What is the next step in treatment for a patient with Stage 2 1st MTPJ arthrosis who has already undergone bunion surgery?
What is the primary concern when considering 1st MTPJ fusion for a patient with a prior bunion surgery?
What is the primary concern when considering 1st MTPJ fusion for a patient with a prior bunion surgery?
What is the treatment goal for a patient with Stage 3 1st MTPJ arthrosis who wants to maintain range of motion?
What is the treatment goal for a patient with Stage 3 1st MTPJ arthrosis who wants to maintain range of motion?
What is the primary indication for a Cheilectomy procedure in Hallux Rigidus?
What is the primary indication for a Cheilectomy procedure in Hallux Rigidus?
What is the consequence of performing a Kessel & Bonney Decompression osteotomy on an adult?
What is the consequence of performing a Kessel & Bonney Decompression osteotomy on an adult?
What is the primary benefit of a Youngswick Decompression osteotomy in Hallux Rigidus?
What is the primary benefit of a Youngswick Decompression osteotomy in Hallux Rigidus?
What is the characteristic of Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the characteristic of Stage 3 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary goal of a Joint-Salvage procedure in Hallux Rigidus?
What is the primary goal of a Joint-Salvage procedure in Hallux Rigidus?
What is the consequence of performing a Cheilectomy procedure on a deteriorated joint?
What is the consequence of performing a Cheilectomy procedure on a deteriorated joint?
What is the primary indication for a Kessel & Bonney Decompression osteotomy?
What is the primary indication for a Kessel & Bonney Decompression osteotomy?
What is the primary goal of arthrodiastasis in the treatment of Hallux Rigidus?
What is the primary goal of arthrodiastasis in the treatment of Hallux Rigidus?
What is the treatment goal for Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the treatment goal for Stage 4 in the Drago, Oloff, & Jacobs Classification of Hallux Rigidus?
What is the primary benefit of a Joint-Salvage procedure in Hallux Rigidus?
What is the primary benefit of a Joint-Salvage procedure in Hallux Rigidus?
What is the primary advantage of the traditional dorsomedial approach in surgical procedures for hallux rigidus?
What is the primary advantage of the traditional dorsomedial approach in surgical procedures for hallux rigidus?
What type of anesthesia is typically required for more proximal procedures in hallux rigidus surgery?
What type of anesthesia is typically required for more proximal procedures in hallux rigidus surgery?
What is the primary purpose of using an ankle tourniquet in distal procedures for hallux rigidus?
What is the primary purpose of using an ankle tourniquet in distal procedures for hallux rigidus?
What is the primary benefit of a medial approach in surgical procedures for hallux rigidus?
What is the primary benefit of a medial approach in surgical procedures for hallux rigidus?
What is the primary purpose of capsulotomy in surgical procedures for hallux rigidus?
What is the primary purpose of capsulotomy in surgical procedures for hallux rigidus?
What is the primary advantage of using epinephrine in hemostasis during hallux rigidus surgery?
What is the primary advantage of using epinephrine in hemostasis during hallux rigidus surgery?
What is the primary purpose of reefing/plication of the medial joint capsule during closure?
What is the primary purpose of reefing/plication of the medial joint capsule during closure?
What is the postoperative course for soft tissue procedures?
What is the postoperative course for soft tissue procedures?
What is the primary concern in postoperative care for soft tissue procedures?
What is the primary concern in postoperative care for soft tissue procedures?
What is the purpose of adductor tendon transfer?
What is the purpose of adductor tendon transfer?
What is the Akin procedure?
What is the Akin procedure?
What is the primary indication for a Distal Akin osteotomy?
What is the primary indication for a Distal Akin osteotomy?
What is the purpose of a Proximal Akin osteotomy?
What is the purpose of a Proximal Akin osteotomy?
What is the primary benefit of using a screw in an Oblique Akin osteotomy?
What is the primary benefit of using a screw in an Oblique Akin osteotomy?
What is the typical postoperative course for proximal phalangeal osteotomies?
What is the typical postoperative course for proximal phalangeal osteotomies?
What is the primary concern when performing a Proximal Akin osteotomy to correct abnormal HAIA?
What is the primary concern when performing a Proximal Akin osteotomy to correct abnormal HAIA?
What is the primary difference between a Cylindrical Akin osteotomy and a Sagittal Z osteotomy?
What is the primary difference between a Cylindrical Akin osteotomy and a Sagittal Z osteotomy?
What is the primary advantage of the traditional dorsomedial approach in surgical procedures for hallux rigidus?
What is the primary advantage of the traditional dorsomedial approach in surgical procedures for hallux rigidus?
What is the primary purpose of using an ankle tourniquet in distal procedures for hallux rigidus?
What is the primary purpose of using an ankle tourniquet in distal procedures for hallux rigidus?
What is the primary benefit of a medial approach in surgical procedures for hallux rigidus?
What is the primary benefit of a medial approach in surgical procedures for hallux rigidus?
What is the primary purpose of using epinephrine in hallux rigidus procedures?
What is the primary purpose of using epinephrine in hallux rigidus procedures?
What is the primary characteristic of a capsulotomy in line with the skin incision?
What is the primary characteristic of a capsulotomy in line with the skin incision?
What is the primary difference between a Mayo block and general anesthesia in hallux rigidus procedures?
What is the primary difference between a Mayo block and general anesthesia in hallux rigidus procedures?
What is the purpose of the Reverdin-Laird osteotomy?
What is the purpose of the Reverdin-Laird osteotomy?
What is the characteristic of the Biplanar Austin osteotomy?
What is the characteristic of the Biplanar Austin osteotomy?
What is the primary purpose of the Youngswick-Austin osteotomy?
What is the primary purpose of the Youngswick-Austin osteotomy?
What is the characteristic of the minimally invasive bunionectomy (MIS)?
What is the characteristic of the minimally invasive bunionectomy (MIS)?
What is the postoperative course for distal metatarsal osteotomies?
What is the postoperative course for distal metatarsal osteotomies?
What is the primary advantage of the Reverdin-Laird osteotomy?
What is the primary advantage of the Reverdin-Laird osteotomy?
What is a specific complication of the Scarf osteotomy that can cause elevation of the capital fragment?
What is a specific complication of the Scarf osteotomy that can cause elevation of the capital fragment?
What is the primary benefit of using 2 screws in the Kalish osteotomy?
What is the primary benefit of using 2 screws in the Kalish osteotomy?
Which osteotomy can correct PASA if the base is rotated laterally?
Which osteotomy can correct PASA if the base is rotated laterally?
What is the primary concern in postoperative care for metatarsal shaft osteotomies?
What is the primary concern in postoperative care for metatarsal shaft osteotomies?
What is the primary benefit of the Scarf osteotomy over a DMO?
What is the primary benefit of the Scarf osteotomy over a DMO?
What is the primary advantage of the Kalish osteotomy over the Scarf osteotomy?
What is the primary advantage of the Kalish osteotomy over the Scarf osteotomy?
What is the specific complication of the Scarf osteotomy that causes elevation of the capital fragment?
What is the specific complication of the Scarf osteotomy that causes elevation of the capital fragment?
What is the primary difference between the Kalish osteotomy and the Scarf osteotomy in terms of PASA correction?
What is the primary difference between the Kalish osteotomy and the Scarf osteotomy in terms of PASA correction?
Why is the Scarf osteotomy considered to be controversial?
Why is the Scarf osteotomy considered to be controversial?
What is the typical postoperative course for metatarsal shaft osteotomies?
What is the typical postoperative course for metatarsal shaft osteotomies?
What is the primary benefit of the Reverdin-Green-Laird modification in distal metatarsal osteotomies?
What is the primary benefit of the Reverdin-Green-Laird modification in distal metatarsal osteotomies?
What is the characteristic of the Biplanar Austin osteotomy?
What is the characteristic of the Biplanar Austin osteotomy?
What is the postoperative course for distal metatarsal osteotomies?
What is the postoperative course for distal metatarsal osteotomies?
What is the primary purpose of the Youngswick-Austin osteotomy?
What is the primary purpose of the Youngswick-Austin osteotomy?
What is the characteristic of the minimally invasive bunionectomy (MIS)?
What is the characteristic of the minimally invasive bunionectomy (MIS)?
What is the primary difference between the Austin and Biplanar Austin osteotomies?
What is the primary difference between the Austin and Biplanar Austin osteotomies?
What is the primary treatment option for a patient with a hallux varus deformity?
What is the primary treatment option for a patient with a hallux varus deformity?
What is a common complication of fibular sesamoidectomy?
What is a common complication of fibular sesamoidectomy?
What is the primary goal when treating a patient with a hallux varus deformity?
What is the primary goal when treating a patient with a hallux varus deformity?
What is a common characteristic of a patient with a mild hallux varus deformity?
What is a common characteristic of a patient with a mild hallux varus deformity?
What is the primary concern when revising a hallux varus deformity?
What is the primary concern when revising a hallux varus deformity?
What is the primary benefit of considering multiple variables when treating a patient with a hallux varus deformity?
What is the primary benefit of considering multiple variables when treating a patient with a hallux varus deformity?
What is the main reason for performing a closing base wedge osteotomy from a more proximal location?
What is the main reason for performing a closing base wedge osteotomy from a more proximal location?
What is the primary consequence of removing a wedge of bone during a closing base wedge osteotomy?
What is the primary consequence of removing a wedge of bone during a closing base wedge osteotomy?
What is the main advantage of performing a closing base wedge osteotomy over a distal head procedure?
What is the main advantage of performing a closing base wedge osteotomy over a distal head procedure?
Why is it difficult to fixate the bone during a closing base wedge osteotomy?
Why is it difficult to fixate the bone during a closing base wedge osteotomy?
What is the ideal characteristic of a patient who would benefit from a closing base wedge osteotomy?
What is the ideal characteristic of a patient who would benefit from a closing base wedge osteotomy?
What is the main challenge during a closing base wedge osteotomy?
What is the main challenge during a closing base wedge osteotomy?
What is the primary benefit of making majority of DMO cuts at an angle?
What is the primary benefit of making majority of DMO cuts at an angle?
What is the limitation of unicorrectional DMO in terms of plane correction?
What is the limitation of unicorrectional DMO in terms of plane correction?
What is the purpose of using Kirshner wires in DMO?
What is the purpose of using Kirshner wires in DMO?
What is the difference between unicorrectional and bicorrectional DMO in terms of corrections?
What is the difference between unicorrectional and bicorrectional DMO in terms of corrections?
What is the result of not making a transverse cut in DMO?
What is the result of not making a transverse cut in DMO?
What is the advantage of DMO in terms of healing?
What is the advantage of DMO in terms of healing?
What is the purpose of resecting the proximal osseous shelf in unicorrectional DMO?
What is the purpose of resecting the proximal osseous shelf in unicorrectional DMO?
What is the difference between uniplanar and biplanar corrections in DMO?
What is the difference between uniplanar and biplanar corrections in DMO?
What is the benefit of adjusting the metatarsal length in DMO?
What is the benefit of adjusting the metatarsal length in DMO?
What is the direction of the correction in biplanar DMO?
What is the direction of the correction in biplanar DMO?
Flashcards are hidden until you start studying
Study Notes
Hallux Rigidus and 1st MTPJ Implant
- Synthetic Cartilage Graft: 1st implant to mimic the modulus of elasticity of cartilage, but subsidence is very common, occurring within 3 weeks post-op.
1st MTPJ Fusion
- Considered the "gold standard" for hallux rigidus surgical treatment
- Definitive positioning is critical for proper function post-operatively
- Optimal positioning: 15° abducted and 15° dorsiflexed
- Lapidus procedure: realigns a structurally pathologic 1st metatarsal, shortens the first ray, and "decompresses" the joint
Drago, Oloff, & Jacobs Classification
- Stage 1: Functional Limitus - limited dorsiflexion with weightbearing, normal ROM with non-weight-bearing, and little/no degenerative changes
- Stage 2: Adaptation - flattening of the first metatarsal head, osteochondral defect, pain on end ROM, limited passive ROM, small dorsal exostosis, and subchondral sclerosis
- Stage 3: Deterioration - severe flattening of the first metatarsal head, dorsal osteophytosis, asymmetric joint space narrowing, degeneration of articular cartilage, crepitus, and subchondral cystic formation
- Stage 4: Anklylosis - obliteration of joint space, exuberant dorsal osteophytosis, < 10° ROM, degeneration of articular cartilage, deformity/malalignment, and total ankylosis
Surgical Treatment Options
- Joint salvage procedures:
- Cheilectomy: joint clean up procedure, removal of osteophytosis, can be primary procedure, often used with others
- Youngswick: decompression osteotomy of metatarsal head, allows for shortening and plantarflexion
- Kessel & Bonney: decompression osteotomy of phalangeal head, changes posture of hallux
- Arthrodiastasis: external fixation with mini-rail, stretches periarticular soft-tissue structure, and gives cartilage a "rest"
- Chondroplasty: addresses cartilage erosions, rarely done in isolation
- Joint destructive procedures:
- Resection arthroplasty
- Interpositional implant arthroplasty
- Valenti Keller Hemi-implants
- Silastic implants
- Cartiva
- Total joint replacement
- 1st MTPJ arthrodesis
- Lapidus
Case Studies
- Case #1: 71-year-old female with 1st MTPJ arthrosis, mild elevatus, pronatory changes, horizontal calcaneal inclination angle, and NC arthrosis with sag; treatment options include 1st MTPJ fusion, NC fusion, gastroc recession, and orthotics/stretching regimen
- Case #2: 66-year-old female with functional limitus, NC sag, and previous bunion surgery; treatment options include orthotics and cheilectomy
- Case #3: 63-year-old female with 1st MTPJ arthrosis, structural rigidus, and smoking history; treatment options include 1st MTPJ fusion### Drago, Oloff, & Jacobs Classification
- Stage 1: Functional Limitus
- Limited dorsiflexion with weightbearing
- Normal ROM with non-weight-bearing
- Little/no degenerative changes
- Biomechanical derangement (pronation)
- 1st ray insufficiency
- Treatment: Joint-Salvage procedure
- Stage 2: Adaptation
- Flattening of the first metatarsal head
- Osteochondral defect
- Pain on end ROM
- Limited passive ROM
- Small dorsal exostosis
- Subchondral sclerosis
- Periarticular lipping of the first metatarsal head, proximal phalanx, & sesamoids
- Treatment: Joint-Salvage procedure
- Stage 3: Deterioration
- Severe flattening of the first metatarsal head
- Dorsal osteophytosis
- Asymmetric joint space narrowing
- Degeneration of articular cartilage
- Crepitus
- Subchondral cystic formation
- Pain on full ROM
- Treatment: Joint-Salvage or Joint-Destructive procedure
- Stage 4: Anklylosis
- Obliteration of joint space
- Exuberant dorsal osteophytosis with loose bodies
- < 10° ROM
- Degeneration of articular cartilage
- Deformity/Malalignment
- Total ankylosis may occur
- Treatment: Joint-Destructive procedure
Hallux Rigidus Surgical Treatment Options
- Joint salvage procedures
- Cheilectomy
- Decompression osteotomy
- Youngswick - distal metatarsal osteotomy
- Kessel & Bonney- phalangeal osteotomy
- Arthrodiastasis
- Chondroplasty (rarely used in isolation)
- Cheilectomy
- Joint clean up procedure
- Removal of osteophytosis from the metatarsal head and proximal phalanx
- Can be the primary procedure
- Often used with other procedures
- Can be coupled with chondroplasty if a chondral defect is present
- Surgical Approach
- Medial approach
- Traditional dorsomedial approach
- Capsulotomy
- In line with the skin incision (most common)
- Numerous other options (Linear, T-shaped, Inverted L-shaped, Oblique, Vertical, U-shaped, H-shaped, L-shaped)
Proximal Phalangeal Osteotomies
- Distal Akin
- Medial closing wedge of the head of the proximal phalanx
- Corrects increased hallux abductus interphalangeus angle (HAIA)
- Oblique Akin
- Corrects abnormal DASA and/or interphalngeus
- Proximal Akin
- Medial closing wedge of the base of the proximal phalanx
- Corrects abnormal DASA
- Cylindrical Akin
- Corrects shortening of a congenitally long proximal phalanx
- Sagittal Z osteotomy
- Corrects shortening or lengthening of the proximal phalanx
Anasthesia and Hemostasis
- Anesthesia
- Depends on the procedure
- Distal first ray work only: Mayo block and IV sedation (MAC with local)
- More proximal: general anesthetic
- Hemostasis
- Epinephrine
- Ankle tourniquet for distal procedures
- Thigh tourniquet for proximal procedures
Postoperative Course
- Weightbearing as tolerated in a post-operative shoe until bone is healed (2-3 weeks for soft tissue procedures, 4-6 weeks for osteotomies)
- More WB protection may be warranted for poor bone quality
- Post-op course based on protection of incision as there is no osteotomy to protect from displacement (soft-tissue procedure only)
Distal Metatarsal Osteotomies
- Austin (Chevron) Osteotomy
- Corrects IMA with translation of the metatarsal head
- Biplanar Austin
- Corrects IMA (transverse)
- Allows for mild plantarflexion (sagittal)
- Bicorrectional Austin
- Corrects PASA
- Youngswick-Austin
- Corrects IMA
- Plantarflexes & shortens the first metatarsal
- Removal of a dorsal rectangle
- Useful for long & mildly elevated 1st metatarsals
- Minimally invasive bunionectomy (MIS)
- Percutaneous transverse osteotomy
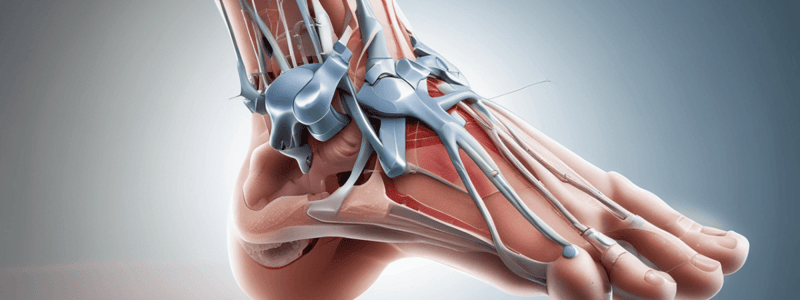
- Capital fragment shifted laterally and fixated with percutaneous screws### Anatomy of the Medial Column and Soft Tissue Surgical Procedures
- Demonstrate knowledge of the anatomy of the medial column
- Soft tissue surgical procedures are performed at the first MTPJ (metatarsophalangeal joint)
Osteotomies for Bunion Correction
- Osteotomies can be performed in the proximal phalanx of the hallux and distal first metatarsal for bunion correction
- Metatarsal shaft osteotomies, proximal first metatarsal procedures, and first metatarsal cuneiform joint arthrodesis can also be used for bunion correction
Distal Metatarsal Osteotomies (DMO)
Basic Concepts
- Most DMO cuts are made at an angle, increasing stability and allowing for more metaphyseal bone contact, which leads to faster healing
- Cuts at an angle spare the articulation of the sesamoidal apparatus, but do not allow for correction of frontal plane deformities
- Transverse cuts are required to correct frontal plane deformities and allow the metatarsal head to rotate
Key Concepts of DMO
- The amount of obtainable correction depends on metatarsal width, as the metatarsal head can only be slid so far before stability is lost
- DMO is a versatile procedure that can achieve multiple corrections depending on procedure selection and angle of cut
- Corrections can be unicorrectional (one correction in the transverse plane), bicorrectional (two corrections in the transverse plane), uniplanar (correction in one plane), or biplanar (corrections in two planes)
Unicorrectional and Bicorrectional DMO
- Unicorrectional DMO involves one transverse plane correction, reducing the intermetatarsal angle (IMA) and performing medial eminence resection
- Bicorrectional DMO involves two transverse plane corrections, reducing both the IMA and PASA (proximal articular set angle)
Uniplanar and Biplanar Corrections
- Uniplanar corrections involve reduction of the intermetatarsal angle in the transverse plane only
- Biplanar corrections involve reduction of the intermetatarsal angle in the transverse plane and angling the cut to allow for plantarflexion or dorsiflexion in the sagittal plane
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.