Podcast
Questions and Answers
What defines the motility of spirochetes?
What defines the motility of spirochetes?
- Periplasmic flagella or endoflagella (correct)
- Flagella located at one end
- Movement through passive diffusion
- Cilia covering their surface
Which genus is NOT part of the Spirochaetaceae family?
Which genus is NOT part of the Spirochaetaceae family?
- Leptospira (correct)
- All are part of Spirochaetaceae
- Treponema
- Borrelia
How can Treponema organisms be visualized in a laboratory setting?
How can Treponema organisms be visualized in a laboratory setting?
- With standard plate culture methods
- Using light microscopy with Gram stain
- Using darkfield microscopy (correct)
- Through macroscopic observation
Which of the following diseases is caused by T.pallidum ssp.pallidum?
Which of the following diseases is caused by T.pallidum ssp.pallidum?
What is a key virulence factor of T.pallidum?
What is a key virulence factor of T.pallidum?
What percentage of patients with neurological or cardiac involvement progress to the subsequent stage of the disease?
What percentage of patients with neurological or cardiac involvement progress to the subsequent stage of the disease?
What is characteristic of Leptospira interrogans?
What is characteristic of Leptospira interrogans?
What is the main route of transmission for leptospirosis to humans?
What is the main route of transmission for leptospirosis to humans?
Which antibiotic is NOT mentioned as a treatment for Lyme disease?
Which antibiotic is NOT mentioned as a treatment for Lyme disease?
Which of the following is a clinical manifestation of anicteric leptospirosis?
Which of the following is a clinical manifestation of anicteric leptospirosis?
What is the main cause of tissue destruction and lesions in syphilis?
What is the main cause of tissue destruction and lesions in syphilis?
Which characteristic describes the chancre during primary syphilis?
Which characteristic describes the chancre during primary syphilis?
In the case of secondary syphilis, which feature is true?
In the case of secondary syphilis, which feature is true?
What percentage of late latent syphilis patients is likely to progress to tertiary syphilis?
What percentage of late latent syphilis patients is likely to progress to tertiary syphilis?
Which process happens during the primary stages of syphilis?
Which process happens during the primary stages of syphilis?
What defines tertiary syphilis?
What defines tertiary syphilis?
Which statement is true regarding the transmission of syphilis?
Which statement is true regarding the transmission of syphilis?
In late stages of syphilis, the inhibition of cell-mediated immunity is:
In late stages of syphilis, the inhibition of cell-mediated immunity is:
What is a common symptom of atypical (walking) pneumonia?
What is a common symptom of atypical (walking) pneumonia?
What type of pneumonia is characterized by an abrupt onset and high fever?
What type of pneumonia is characterized by an abrupt onset and high fever?
Which treatment is effective against M. genitalium?
Which treatment is effective against M. genitalium?
What is a secondary complication associated with M. pneumoniae infection?
What is a secondary complication associated with M. pneumoniae infection?
What is the main prevention strategy for M. pneumoniae infections?
What is the main prevention strategy for M. pneumoniae infections?
What is the primary consequence of congenital syphilis for the developing fetus?
What is the primary consequence of congenital syphilis for the developing fetus?
What is the recommended duration for penicillin treatment of early-stage syphilis?
What is the recommended duration for penicillin treatment of early-stage syphilis?
Treponema pallidum subsp.pertenue is primarily associated with which disease?
Treponema pallidum subsp.pertenue is primarily associated with which disease?
Which of the following methods is NOT recommended for the prevention of syphilis?
Which of the following methods is NOT recommended for the prevention of syphilis?
What type of lesions are initially associated with Bejel?
What type of lesions are initially associated with Bejel?
The incubation period for Pinta is approximately how long?
The incubation period for Pinta is approximately how long?
Which of the following best describes the disease Yaws?
Which of the following best describes the disease Yaws?
What is the primary mode of transmission for Treponema carateum, the causative agent of Pinta?
What is the primary mode of transmission for Treponema carateum, the causative agent of Pinta?
What is the primary cause of hepatic injury in icteric leptospirosis?
What is the primary cause of hepatic injury in icteric leptospirosis?
Which treatment is considered effective for icteric leptospirosis?
Which treatment is considered effective for icteric leptospirosis?
What is a common symptom of leptospiremia in the early stages of illness?
What is a common symptom of leptospiremia in the early stages of illness?
Which characteristic is true for Mycoplasma bacteria?
Which characteristic is true for Mycoplasma bacteria?
What structural feature distinguishes Mycoplasma bacteria from most other bacteria?
What structural feature distinguishes Mycoplasma bacteria from most other bacteria?
What role do P1 pili play in the virulence of M.pneumoniae?
What role do P1 pili play in the virulence of M.pneumoniae?
What is a distinguishing feature of Mycoplasma colonies when cultured?
What is a distinguishing feature of Mycoplasma colonies when cultured?
Which of the following is a common clinical manifestation of M.pneumoniae infection?
Which of the following is a common clinical manifestation of M.pneumoniae infection?
What characteristic of Treponema makes it challenging to observe with light microscopy?
What characteristic of Treponema makes it challenging to observe with light microscopy?
Which virulence factor of Treponema pallidum is associated with facilitating tissue infiltration?
Which virulence factor of Treponema pallidum is associated with facilitating tissue infiltration?
Which disease is caused by the subspecies of Treponema pallidum identified as T.pallidum ssp. pertenue?
Which disease is caused by the subspecies of Treponema pallidum identified as T.pallidum ssp. pertenue?
What primarily causes tissue destruction and lesions associated with T.pallidum infections?
What primarily causes tissue destruction and lesions associated with T.pallidum infections?
What unique structural feature of spirochetes contributes to their motility?
What unique structural feature of spirochetes contributes to their motility?
What is a characteristic feature of Leptospira interrogans?
What is a characteristic feature of Leptospira interrogans?
What are the primary host animals associated with the transmission of leptospirosis?
What are the primary host animals associated with the transmission of leptospirosis?
What type of antibiotic is indicated for the treatment of relapsing fever?
What type of antibiotic is indicated for the treatment of relapsing fever?
What is the primary cause of tissue destruction and lesions in leptospirosis?
What is the primary cause of tissue destruction and lesions in leptospirosis?
Which stage of Lyme disease may exhibit migrating episodes of painful arthritis?
Which stage of Lyme disease may exhibit migrating episodes of painful arthritis?
Which of the following symptoms is NOT typically associated with atypical (walking) pneumonia?
Which of the following symptoms is NOT typically associated with atypical (walking) pneumonia?
What is the primary treatment recommended for M. hominis infections?
What is the primary treatment recommended for M. hominis infections?
Which of the following complications is NOT associated with M. pneumoniae infection?
Which of the following complications is NOT associated with M. pneumoniae infection?
Which treatment option is considered ineffective against M. pneumoniae infections?
Which treatment option is considered ineffective against M. pneumoniae infections?
What is a notable characteristic of Mycoplasma bacteria?
What is a notable characteristic of Mycoplasma bacteria?
What is the hallmark lesion associated with primary syphilis?
What is the hallmark lesion associated with primary syphilis?
Which statement accurately describes the secondary stage of syphilis?
Which statement accurately describes the secondary stage of syphilis?
During which stage of syphilis is the patient non-infectious?
During which stage of syphilis is the patient non-infectious?
What typically occurs at the site of inoculation during primary syphilis?
What typically occurs at the site of inoculation during primary syphilis?
Which feature is characteristic of tertiary syphilis?
Which feature is characteristic of tertiary syphilis?
What indicates the onset of the latent stage of syphilis?
What indicates the onset of the latent stage of syphilis?
What is a potential outcome for infants affected by congenital syphilis?
What is a potential outcome for infants affected by congenital syphilis?
Which treatment duration is appropriate for early-stage syphilis?
Which treatment duration is appropriate for early-stage syphilis?
What type of lesions are the initial manifestations of Bejel?
What type of lesions are the initial manifestations of Bejel?
Which of the following is true regarding the transmission of Yaws?
Which of the following is true regarding the transmission of Yaws?
What are the late-stage lesions associated with Pinta?
What are the late-stage lesions associated with Pinta?
Which antibiotic is the primary choice for treating syphilis?
Which antibiotic is the primary choice for treating syphilis?
Which of the following is a characteristic of Treponema pallidum subsp.pertenue?
Which of the following is a characteristic of Treponema pallidum subsp.pertenue?
What is a recommended method for syphilis prevention?
What is a recommended method for syphilis prevention?
Which symptom is typically associated with leptospiremia during the early stages of illness?
Which symptom is typically associated with leptospiremia during the early stages of illness?
What is a common treatment for icteric leptospirosis?
What is a common treatment for icteric leptospirosis?
Which of the following is a characteristic of Mycoplasma bacteria?
Which of the following is a characteristic of Mycoplasma bacteria?
Which Mycoplasma species is specifically known for causing infections in the respiratory tract?
Which Mycoplasma species is specifically known for causing infections in the respiratory tract?
What role do P1 pili play in M.pneumoniae virulence?
What role do P1 pili play in M.pneumoniae virulence?
Which of the following statements about the incubation period for icteric leptospirosis is correct?
Which of the following statements about the incubation period for icteric leptospirosis is correct?
What type of colonies do Mycoplasma bacteria form when cultured?
What type of colonies do Mycoplasma bacteria form when cultured?
Flashcards
Spirochetes
Spirochetes
A type of bacteria known for its spiral (coiled) shape, belonging to the order Spirochaetales.
Origin of the term 'Spirochete'
Origin of the term 'Spirochete'
The term 'Spirochete' comes from the Greek word for 'coiled hair'.
Physical characteristics of Spirochetes
Physical characteristics of Spirochetes
These bacteria are extremely thin and can be very long.
Motility of Spirochetes
Motility of Spirochetes
Signup and view all the flashcards
Treponema classification
Treponema classification
Signup and view all the flashcards
Treponema pallidum
Treponema pallidum
Signup and view all the flashcards
Primary syphilis
Primary syphilis
Signup and view all the flashcards
Secondary syphilis
Secondary syphilis
Signup and view all the flashcards
Latent stage syphilis
Latent stage syphilis
Signup and view all the flashcards
Tertiary syphilis
Tertiary syphilis
Signup and view all the flashcards
Treponema pallidum infection and immune response
Treponema pallidum infection and immune response
Signup and view all the flashcards
Treponema pallidum and vasculature
Treponema pallidum and vasculature
Signup and view all the flashcards
Persistence of Treponema pallidum
Persistence of Treponema pallidum
Signup and view all the flashcards
Syphilis
Syphilis
Signup and view all the flashcards
Congenital Syphilis
Congenital Syphilis
Signup and view all the flashcards
Penicillin
Penicillin
Signup and view all the flashcards
Bejel (Endemic Syphilis)
Bejel (Endemic Syphilis)
Signup and view all the flashcards
Yaws
Yaws
Signup and view all the flashcards
Pinta
Pinta
Signup and view all the flashcards
Leptospirosis
Leptospirosis
Signup and view all the flashcards
Borrelia
Borrelia
Signup and view all the flashcards
Leptospira interrogans
Leptospira interrogans
Signup and view all the flashcards
Leptospira
Leptospira
Signup and view all the flashcards
Virulence factors of Leptospira interrogans
Virulence factors of Leptospira interrogans
Signup and view all the flashcards
Epidemiology of leptospirosis
Epidemiology of leptospirosis
Signup and view all the flashcards
What is icteric leptospirosis?
What is icteric leptospirosis?
Signup and view all the flashcards
What is leptospiremia?
What is leptospiremia?
Signup and view all the flashcards
What is leptospiruria?
What is leptospiruria?
Signup and view all the flashcards
How is icteric leptospirosis treated and prevented?
How is icteric leptospirosis treated and prevented?
Signup and view all the flashcards
What makes Mycoplasmas unique?
What makes Mycoplasmas unique?
Signup and view all the flashcards
What are some common human diseases caused by Mycoplasmas?
What are some common human diseases caused by Mycoplasmas?
Signup and view all the flashcards
How does M. pneumoniae adhere to respiratory tissues?
How does M. pneumoniae adhere to respiratory tissues?
Signup and view all the flashcards
How does M. pneumoniae trigger excessive inflammation?
How does M. pneumoniae trigger excessive inflammation?
Signup and view all the flashcards
Atypical (Walking) Pneumonia
Atypical (Walking) Pneumonia
Signup and view all the flashcards
Mycoplasma pneumoniae Infections
Mycoplasma pneumoniae Infections
Signup and view all the flashcards
Mycoplasmas
Mycoplasmas
Signup and view all the flashcards
Treatment for Mycoplasma pneumoniae Infections
Treatment for Mycoplasma pneumoniae Infections
Signup and view all the flashcards
Other Mycoplasmas and Their Infections
Other Mycoplasmas and Their Infections
Signup and view all the flashcards
Treponema
Treponema
Signup and view all the flashcards
Syphilis and Cardiovascular Health
Syphilis and Cardiovascular Health
Signup and view all the flashcards
Penicillin for Syphilis
Penicillin for Syphilis
Signup and view all the flashcards
Preventing Syphilis
Preventing Syphilis
Signup and view all the flashcards
Treating Syphilis
Treating Syphilis
Signup and view all the flashcards
Latent Syphilis
Latent Syphilis
Signup and view all the flashcards
Chancre
Chancre
Signup and view all the flashcards
Gumma
Gumma
Signup and view all the flashcards
Syphilis and Vasculature
Syphilis and Vasculature
Signup and view all the flashcards
Clinical Disease: Leptospirosis
Clinical Disease: Leptospirosis
Signup and view all the flashcards
Icteric Leptospirosis
Icteric Leptospirosis
Signup and view all the flashcards
Leptospiremia
Leptospiremia
Signup and view all the flashcards
Leptospiruria
Leptospiruria
Signup and view all the flashcards
M. pneumoniae
M. pneumoniae
Signup and view all the flashcards
M. genitalium
M. genitalium
Signup and view all the flashcards
P1 pili
P1 pili
Signup and view all the flashcards
Superantigen
Superantigen
Signup and view all the flashcards
Atypical Pneumonia
Atypical Pneumonia
Signup and view all the flashcards
Mycoplasma pneumoniae
Mycoplasma pneumoniae
Signup and view all the flashcards
Treatment for Mycoplasma pneumoniae
Treatment for Mycoplasma pneumoniae
Signup and view all the flashcards
Study Notes
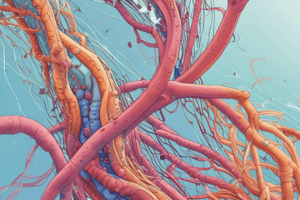
Spirochaetes
- Gram-negative bacteria
- Shaped like a spiral
- Extremely thin, can be very long
- Motile due to periplasmic flagella (axial fibrils or endoflagella)
Taxonomy
- Order: Spirochaetales
- Family: Spirochaetaceae
- Genus: Treponema
- Species: T. pallidum ssp. pallidum (Syphilis)
- Species: T. pallidum ssp. endemicum (Bejel)
- Species: T. pallidum ssp. pertenue(Yaws) -Species: T. carateum(Pinta)
- Genus: Treponema
- Family: Leptospiraceae
- Genus: Leptospira
- Species: L. interrogans
- Genus: Leptospira
Treponema
- Too thin to be seen by light microscopy in stained specimens
- Motile spirochetes can be seen with darkfield microscopy.
- Stained with anti-treponemal antibodies labeled with fluorescent dyes
- Intracellular pathogen
- Has three periplasmic flagella at each end
- Cannot be grown in cell-free cultures in vitro (meaning it does not survive well outside a host)
Treponema and Human Disease
- T. pallidum ssp. pallidum causes Syphilis, transmitted by direct sexual contact or from mother to fetus.
- Transmission rates depend on the stage of the disease.
- Syphilis has a long incubation period when the host is non-infectious.
- Syphilis causes tissue destruction and lesions, which are primarily caused by the patient’s immune response.
- Syphilis is a disease of blood vessels and the perivascular areas, and the organisms can persist for decades.
- Primary Syphilis involves invasion of mucus membranes, rapid multiplication, and wide dissemination through perivascular lymphatic system. The first sign is a painless chancre.
- Secondary Syphilis shows up 2-10 weeks after the primary lesion. Characterized by a widely disseminated mucocutaneous rash and secondary lesions.
- Latent stage syphilis: following secondary disease, the host enters a latent period.
- First 4 years = early latent
- Subsequent period = late latent
- 40% of late latent patients progress to late tertiary syphilitic disease
- Tertiary syphilis: characterized by localized granulomatous dermal lesions (gummas), few microorganisms present.
- Late neurosyphilis develops usually more than 5 years after initial infection, involving the central nervous system and spinal cord, and can cause dementia, seizures, and wasting.
- Cardiovascular involvement can appear 10-40 years after initial infection resulting in myocardial insufficiency and death.
Congenital Syphilis
- Results from transplacental infection
- Characterized by T. pallidum septicemia in the developing fetus and wide dissemination.
- Can cause abortion, neonatal mortality, and late mental or physical problems
Prevention and Treatment of Syphilis
- Penicillin is the drug of choice.
- WHO monitors treatment recommendations
- 7-10 days continuously for early stage
- At least 21 days continuously beyond early stage
- Prevention with barrier methods
- Prophylactic treatment for contacts identified through epidemiological tracing
Treponema pallidum subsp. endemicum
- Causes Bejel (endemic syphilis).
- Initial lesions are oral, and secondary lesions are oral papules and mucosal patches
- Late lesions are gummas of skin, bones, and nasopharynx
- Transmitted person-to-person by contaminated eating utensils
- Found in primitive tropical/subtropical areas (Africa, Asia, and Australia)
Treponema pallidum subsp pertenue
- Characterized by Yaws: granulomatous skin disease, early skin lesions, late destructive lesions of skin, lymph nodes and bones with painless nodules widely distributed over body.
- Transmitted via direct contact with lesions of the skin containing abundant spirochetes
- Typical of primitive tropical areas (South America, Central Africa, Southeast Asia).
Treponema carateum
- Primarily restricted to skin
- Has a 1-3 week incubation period
- Initial symptoms are small pruritic papules which progress into enlarged plaques that last for months to years
- Late lesions may cause disseminated, recurrent hypopigmentation or depigmentation of skin
- Transmitted by direct skin-to-skin contact.
- Found in primitive tropical areas (Mexico, Central and South America).
Borrelia spp.
- Gram-negative spirochetes identified via Giemsa stain of blood, and phase contrast microscopy
- Antigenic shift and immune reactions are responsible for the disease
Borrelia and Human Disease
- B. recurrentis: reservoir: humans, vector: body lice; causes Relapsing fever (epidemic)
- B. spp: reservoir: rodents and ticks, vector: soft-shelled ticks; causes Relapsing fever (endemic)
- B. burgdorferi: reservoir: rodents, ticks, other animals, vector: hard-shelled ticks; causes Lyme disease
Relapsing Fever
- Associated with poverty, crowding, and warfare
- Arthropod vectors (lice or ticks) transmit person-to-person.
- Lice transmit to hosts only when injured (e.g., during scratching).
- Lice leave infected hosts and seek normal temperature hosts.
- Often characterized by an acute infection with a 2-14 day incubation period followed by recurring febrile episodes and a constantly worsening spirochaetemia during these febrile episodes.
Epidemiology of Lyme Borreliosis
- Recognized in 1975 in Lyme, Connecticut
- Associated with B. burgdorferi
- Transmitted by hard-bodied ticks (Ixodes)
- Reservoirs are white-footed deer mice, other rodents, deer, domesticated pets, and hard-shelled ticks.
Lyme Disease
- Characterized by three stages with an initial unique skin lesion (erythema migrans) with malaise.
- Lesions periodically reoccur.
- 5-15% of patients develop neurological or cardiac involvement.
- Third stage involves non-destrucive, but painful arthritis.
Leptospira interrogans
- Gram-negative spirochete, with characteristic hooked ends (like a question mark)
- Two periplasmic flagella
- Tissue destruction and lesions are caused by the host's immune response
- Able to directly invade and replicate in tissues, inducing inflammatory response
Epidemiology of Leptospirosis
- Zoonotic disease (transmitted to humans from various wild and domestic animal hosts such as rats, dogs, farm, and wild animals.)
- Transmitted through breaks in the skin or intact mucus membranes, or through indirect contact with infected urine (e.g., in soil, water, feed).
- Occupational disease of animal handling
Clinical Disease: Leptospirosis
-
Mild virus-like syndrome
-
Anicteric leptospirosis: systemic with aseptic meningitis
-
Icteric leptospirosis (Weil's disease): overwhelming disease with vascular collapse, thrombocytopenia, hemorrhage, hepatic and renal dysfunction
-
Note: Icteric refers to jaundice (yellowing of skin and mucus membranes from deposition of bile) and liver involvement
Pathogenesis of Icteric Leptospirosis
- Direct invasion and replication in tissues.
- Characterized by an acute febrile jaundice and glomerulonephritis.
- 10-12 day incubation period with flu-like illness, progressing through two clinical stages.
- Leptospiremia develops rapidly (usually lasts 7 days) without local lesion.
- Infect the kidneys, shed in the urine (leptospiruria), with renal failure and death.
- Hepatic injury and meningeal irritation is common.
Treatment of Leptospirosis
- Treatment with penicillin or doxycycline
- Control reservoirs
- Vaccinate animals
Mycoplasmas
- Smallest bacteria (0.1-0.3 µm)
- Grow slowly, need sterols and glucose as a source of energy
- Ureaplasma spp requires urea.
- Facultative anaerobes; except M. pneumoniae - strict aerobe.
- Lack a cell wall.
- Resistant to penicillin, cephalosporins, vancomycin but sensitive to tetracycline and erythromycin.
- Small, fried-egg-like colonies (except M. pneumoniae)
Mycoplasmataceae and Human Disease
- Genus: Mycoplasma
- Species: M. pneumoniae
- Species: M. hominis
- Species: M. genitalium
- Genus: Ureaplasma
- Species: U. urealyticum
M. pneumoniae
- Primarily asymptomatic carriage
- Causes acute pharyngitis, low-grade-fever, malaise, headache, persistent dry and non-productive cough for more than 2 weeks
- Tracheobronchitis with lymphocyte and plasma cell infiltration, and an atypical (walking) pneumonia.
- Secondary complications include hemolytic anemia, arthritis, myocarditis, pericarditis, and neurologic abnormalities (like meningoencephalitis)
Atypical (Walking) Pneumonia
- Chronic; onset and recovery
- Flu-like symptoms (generalized aches, discomfort, headache, chills, and low-grade fever).
- Persistent non-productive cough
Typical (Bacterial) Pneumonia
- Abrupt, rigorous onset
- Productive cough with purulent sputum
- High fever, chest pain stiffness in the neck
Treatment and Prevention of M. pneumoniae
- Treatment with tetracycline or erythromycin or newer fluoroquinolones (cannot use cell wall synthesis inhibitors)
- Prevention: avoid close contact; no vaccine.
Other Mycoplasmataceae
- M. genitalium: erythromycin, tetracycline
- Ureaplasma: erythromycin.
- M. hominis: clindamycin
- Avoid unprotected sex.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.