Podcast
Questions and Answers
Which of the following correctly describes the mechanism by which sepsis leads to decreased oxygen delivery to organs?
Which of the following correctly describes the mechanism by which sepsis leads to decreased oxygen delivery to organs?
- Decreased cardiac output due to a combination of dilated blood vessels and increased vascular permeability. (correct)
- Reduced oxygen carrying capacity of blood due to the formation of microclots in the capillaries.
- Increased red blood cell destruction due to disseminated intravascular coagulation (DIC).
- Increased systemic vascular resistance due to vasoconstriction.
Which of the following is a direct consequence of the increased permeability of blood vessels during sepsis?
Which of the following is a direct consequence of the increased permeability of blood vessels during sepsis?
- Increased production of systemic cytokines.
- Development of disseminated intravascular coagulation (DIC).
- Formation of microclots in the capillaries. (correct)
- Increased metabolic acidosis.
Which of the following best explains the link between sepsis and the development of metabolic acidosis?
Which of the following best explains the link between sepsis and the development of metabolic acidosis?
- Accumulation of lactic acid as a byproduct of anaerobic metabolism in oxygen-deprived tissues. (correct)
- Increased production of ketones by the liver in response to low blood sugar.
- Reduced oxygen delivery to tissues due to microclot formation and decreased cardiac output.
- Decreased bicarbonate production by the kidneys due to organ dysfunction.
Which of the following accurately describes the role of disseminated intravascular coagulation (DIC) in sepsis?
Which of the following accurately describes the role of disseminated intravascular coagulation (DIC) in sepsis?
Which of the following best explains the clinical presentation of increased respiratory rate (tachypnea) and accessory muscle use in sepsis?
Which of the following best explains the clinical presentation of increased respiratory rate (tachypnea) and accessory muscle use in sepsis?
A patient presents with a pH of 7.32, PaCO2 of 48 mmHg, and HCO3 of 25 mEq/L. What is the most likely interpretation of these findings?
A patient presents with a pH of 7.32, PaCO2 of 48 mmHg, and HCO3 of 25 mEq/L. What is the most likely interpretation of these findings?
A patient with a history of chronic obstructive pulmonary disease (COPD) is found to have a PaCO2 of 60 mmHg. Which of the following is most likely to be the patient's pH?
A patient with a history of chronic obstructive pulmonary disease (COPD) is found to have a PaCO2 of 60 mmHg. Which of the following is most likely to be the patient's pH?
A patient presents with severe diarrhea resulting in excessive bicarbonate loss. Which of the following changes in blood gas parameters would you expect to see?
A patient presents with severe diarrhea resulting in excessive bicarbonate loss. Which of the following changes in blood gas parameters would you expect to see?
A patient with a history of hyperventilation is found to have a PaCO2 of 28 mmHg. Which of the following mechanisms is most likely responsible for this finding?
A patient with a history of hyperventilation is found to have a PaCO2 of 28 mmHg. Which of the following mechanisms is most likely responsible for this finding?
Which of the following scenarios would most likely result in an increased pH and a decreased PaCO2?
Which of the following scenarios would most likely result in an increased pH and a decreased PaCO2?
A patient with a pH of 7.50 and a HCO3 of 32 mEq/L is most likely experiencing which of the following conditions?
A patient with a pH of 7.50 and a HCO3 of 32 mEq/L is most likely experiencing which of the following conditions?
Which of the following interpretations is incorrect regarding the relationship between pH and PaCO2 in respiratory compensation for metabolic acidosis?
Which of the following interpretations is incorrect regarding the relationship between pH and PaCO2 in respiratory compensation for metabolic acidosis?
A patient with a history of asthma is experiencing an acute asthma exacerbation. Would you expect to see a decrease in PaCO2, an increase in PaCO2, or no change in PaCO2?
A patient with a history of asthma is experiencing an acute asthma exacerbation. Would you expect to see a decrease in PaCO2, an increase in PaCO2, or no change in PaCO2?
Flashcards
Sepsis
Sepsis
A severe reaction to infection causing systemic inflammation.
Immunologic overactivity
Immunologic overactivity
An exaggerated immune response to infection leading to harmful effects.
Cytokines
Cytokines
Proteins released during inflammation that trigger immune responses.
Disseminated intravascular coagulopathy (DIC)
Disseminated intravascular coagulopathy (DIC)
Signup and view all the flashcards
Metabolic acidosis
Metabolic acidosis
Signup and view all the flashcards
ABG Normal Values
ABG Normal Values
Signup and view all the flashcards
Lactic Acid
Lactic Acid
Signup and view all the flashcards
Respiratory Compensation
Respiratory Compensation
Signup and view all the flashcards
Respiratory Issues
Respiratory Issues
Signup and view all the flashcards
Metabolic Issues
Metabolic Issues
Signup and view all the flashcards
Acidosis
Acidosis
Signup and view all the flashcards
Alkalosis
Alkalosis
Signup and view all the flashcards
ABG Interpretation Rule
ABG Interpretation Rule
Signup and view all the flashcards
Study Notes
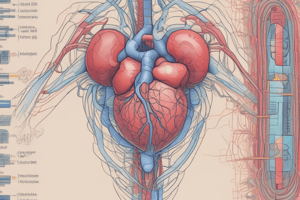
Sepsis Summary
- Infection triggers reaction.
- Triggers immunologic overactivity.
- Hyperactive response + white blood cells.
- Systemic cytokines released.
- Dilated blood vessels + permeability.
- SpO2 ↓ HR ↑ BP ↓
- Rash /Edema.
- Lowers SV, HR ↑ + low O2 to organs.
- Respiratory ↑ acidosis.
- Accessory muscle use.
- Triggers disseminated intravascular coagulopathy.
- Leads to metabolic acidosis → Multiple organ failure → even less O2.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.