Podcast
Questions and Answers
According to the CDC, approximately how many adults in the United States develop sepsis annually?
According to the CDC, approximately how many adults in the United States develop sepsis annually?
- 270,000
- 1.7 million (correct)
- 3.4 million
- 500,000
Which type of infection is most commonly associated with the progression of sepsis?
Which type of infection is most commonly associated with the progression of sepsis?
- Gram-positive bacterial infections (correct)
- Gram-negative bacterial infections
- Fungal infections
- Viral infections
Which of the following is NOT identified as a factor contributing to the increasing incidence of sepsis?
Which of the following is NOT identified as a factor contributing to the increasing incidence of sepsis?
- Decreasing use of invasive procedures (correct)
- Increased antimicrobial resistance
- Aging population
- Increased use of immunosuppressive medications
According to the Sepsis 3 definition, what is the hallmark of sepsis?
According to the Sepsis 3 definition, what is the hallmark of sepsis?
What condition is characterized by profound circulatory and metabolic abnormalities, greatly increasing mortality?
What condition is characterized by profound circulatory and metabolic abnormalities, greatly increasing mortality?
Which of the following is a hematological disorder associated with enhanced coagulation and is a possible complication of severe sepsis?
Which of the following is a hematological disorder associated with enhanced coagulation and is a possible complication of severe sepsis?
What is the immediate immune response activated upon pathogen invasion?
What is the immediate immune response activated upon pathogen invasion?
Which of the following is a late manifestation of septic shock, indicating prolonged poor tissue perfusion?
Which of the following is a late manifestation of septic shock, indicating prolonged poor tissue perfusion?
In the progression of MODS, which organ system is typically the first to show signs of dysfunction?
In the progression of MODS, which organ system is typically the first to show signs of dysfunction?
What is a late indicator of progressive sepsis related to clotting that indicates the development of Disseminated Intravascular Coagulation (DIC)?
What is a late indicator of progressive sepsis related to clotting that indicates the development of Disseminated Intravascular Coagulation (DIC)?
What is the significance of elevated venous oxygen saturation (SvO2) and ScvO2 levels in the later stages of sepsis?
What is the significance of elevated venous oxygen saturation (SvO2) and ScvO2 levels in the later stages of sepsis?
Which of these laboratory findings is NOT associated with the progression to Disseminated Intravascular Coagulation (DIC) in sepsis?
Which of these laboratory findings is NOT associated with the progression to Disseminated Intravascular Coagulation (DIC) in sepsis?
What is the primary mechanism that leads to the systemic vasodilation observed in sepsis?
What is the primary mechanism that leads to the systemic vasodilation observed in sepsis?
In the later stages of septic shock (cold shock), what best describes the change in venous oxygen levels?
In the later stages of septic shock (cold shock), what best describes the change in venous oxygen levels?
Which of the following best describes the state of blood volume during septic shock?
Which of the following best describes the state of blood volume during septic shock?
What is the role of antithrombin III in the coagulation cascade?
What is the role of antithrombin III in the coagulation cascade?
Which of the following best contributes to the pro-inflammatory effect seen in sepsis?
Which of the following best contributes to the pro-inflammatory effect seen in sepsis?
What is the primary goal of the Surviving Sepsis campaign?
What is the primary goal of the Surviving Sepsis campaign?
In early or 'warm' sepsis, what assessment findings would be most expected?
In early or 'warm' sepsis, what assessment findings would be most expected?
Which is the most accurate description of protein C's role in the coagulation process?
Which is the most accurate description of protein C's role in the coagulation process?
What is the commonality of tools like NEWS, MEWS and SOFA in sepsis assessment?
What is the commonality of tools like NEWS, MEWS and SOFA in sepsis assessment?
According to the latest guidelines, within what timeframe should a patient needing a higher level of care be admitted to the ICU?
According to the latest guidelines, within what timeframe should a patient needing a higher level of care be admitted to the ICU?
Which of these practices constitutes a first-line therapy for preventing infections in a healthcare setting?
Which of these practices constitutes a first-line therapy for preventing infections in a healthcare setting?
Within the 'Surviving Sepsis Campaign' bundle of care, what is the recommended initial intravenous fluid for resuscitation?
Within the 'Surviving Sepsis Campaign' bundle of care, what is the recommended initial intravenous fluid for resuscitation?
Which vasopressor is recommended as the first-line choice by the Surviving Sepsis campaign to maintain the appropriate mean arterial pressure in patients with sepsis?
Which vasopressor is recommended as the first-line choice by the Surviving Sepsis campaign to maintain the appropriate mean arterial pressure in patients with sepsis?
According to the provided information, when should antibiotics be administered in relation to suspected sepsis?
According to the provided information, when should antibiotics be administered in relation to suspected sepsis?
Which medication is LEAST likely to be implicated in masking a patient's response to pain or discomfort during withdrawal of support?
Which medication is LEAST likely to be implicated in masking a patient's response to pain or discomfort during withdrawal of support?
When are corticosteroids typically recommended in the treatment of sepsis according to the Surviving Sepsis guidelines?
When are corticosteroids typically recommended in the treatment of sepsis according to the Surviving Sepsis guidelines?
What is the PRIMARY mechanism by which stress ulcers develop in critically ill patients?
What is the PRIMARY mechanism by which stress ulcers develop in critically ill patients?
Which hemodynamic parameter is preferred for monitoring responsiveness to therapy by the Surviving Sepsis campaign?
Which hemodynamic parameter is preferred for monitoring responsiveness to therapy by the Surviving Sepsis campaign?
What is the most common initial clinical manifestation when clots lodge in the microvasculature during the thrombotic phase of DIC?
What is the most common initial clinical manifestation when clots lodge in the microvasculature during the thrombotic phase of DIC?
Which dynamic measure is recommended to assess fluid responsiveness by the provided content?
Which dynamic measure is recommended to assess fluid responsiveness by the provided content?
Which laboratory finding is LEAST likely to be present during the bleeding phase of DIC?
Which laboratory finding is LEAST likely to be present during the bleeding phase of DIC?
What should be a primary consideration when discussions regarding withdrawal of life support are initiated with patients or their families?
What should be a primary consideration when discussions regarding withdrawal of life support are initiated with patients or their families?
Which of the following is considered a primary risk factor for clinically significant stress ulcer bleeding?
Which of the following is considered a primary risk factor for clinically significant stress ulcer bleeding?
When transitioning from active intervention to palliative care during the withdrawal of life support, it is crucial to emphasize:
When transitioning from active intervention to palliative care during the withdrawal of life support, it is crucial to emphasize:
What is the PRIMARY treatment for a patient experiencing bleeding from a stress ulcer?
What is the PRIMARY treatment for a patient experiencing bleeding from a stress ulcer?
Which of the following is NOT a common cause of Disseminated Intravascular Coagulopathy?
Which of the following is NOT a common cause of Disseminated Intravascular Coagulopathy?
What is the PRIMARY objective of an ethics consultation in cases of conflict during withdrawal of support?
What is the PRIMARY objective of an ethics consultation in cases of conflict during withdrawal of support?
What is the expected outcome when fibrinolysis attempts to break down clots during the bleeding phase of DIC?
What is the expected outcome when fibrinolysis attempts to break down clots during the bleeding phase of DIC?
In addition to treating the underlying cause, which supportive treatment method is LEAST likely to be used in managing DIC?
In addition to treating the underlying cause, which supportive treatment method is LEAST likely to be used in managing DIC?
Flashcards
Sepsis
Sepsis
A life-threatening condition triggered by a widespread inflammatory response to infection, resulting in organ dysfunction.
Septic Shock
Septic Shock
A life-threatening complication of sepsis characterized by abnormal circulation and metabolism, leading to a significant increase in mortality.
Innate Immune Response
Innate Immune Response
The initial, non-specific immune response triggered by a pathogen, involving neutrophils, macrophages, and inflammatory signals.
Pro-inflammatory Cytokines
Pro-inflammatory Cytokines
Signup and view all the flashcards
Complement Proteins
Complement Proteins
Signup and view all the flashcards
Disseminated Intravascular Coagulation (DIC)
Disseminated Intravascular Coagulation (DIC)
Signup and view all the flashcards
Multiple Organ Dysfunction Syndrome (MODS)
Multiple Organ Dysfunction Syndrome (MODS)
Signup and view all the flashcards
Localized Inflammation
Localized Inflammation
Signup and view all the flashcards
Coagulation Cascade
Coagulation Cascade
Signup and view all the flashcards
Protein C
Protein C
Signup and view all the flashcards
Antithrombin III
Antithrombin III
Signup and view all the flashcards
Hyperdynamic Sepsis (Warm Sepsis)
Hyperdynamic Sepsis (Warm Sepsis)
Signup and view all the flashcards
Hypodynamic Sepsis (Cold Sepsis)
Hypodynamic Sepsis (Cold Sepsis)
Signup and view all the flashcards
Surviving Sepsis Campaign
Surviving Sepsis Campaign
Signup and view all the flashcards
Sepsis Prevention
Sepsis Prevention
Signup and view all the flashcards
Sepsis Admission Guideline
Sepsis Admission Guideline
Signup and view all the flashcards
Surviving Sepsis Bundle
Surviving Sepsis Bundle
Signup and view all the flashcards
Fluid Resuscitation in Sepsis
Fluid Resuscitation in Sepsis
Signup and view all the flashcards
Fluid Resuscitation Solution
Fluid Resuscitation Solution
Signup and view all the flashcards
Antibiotic Timing in Sepsis
Antibiotic Timing in Sepsis
Signup and view all the flashcards
Corticosteroids in Sepsis
Corticosteroids in Sepsis
Signup and view all the flashcards
Ongoing Monitoring in Sepsis
Ongoing Monitoring in Sepsis
Signup and view all the flashcards
Withdrawal of Life Support in Sepsis
Withdrawal of Life Support in Sepsis
Signup and view all the flashcards
Palliative Care in Sepsis
Palliative Care in Sepsis
Signup and view all the flashcards
Apoptosis
Apoptosis
Signup and view all the flashcards
Microvascular Dysfunction
Microvascular Dysfunction
Signup and view all the flashcards
Mitochondrial Toxicity
Mitochondrial Toxicity
Signup and view all the flashcards
Decreased DO2 in Sepsis
Decreased DO2 in Sepsis
Signup and view all the flashcards
Hypermetabolism in Sepsis
Hypermetabolism in Sepsis
Signup and view all the flashcards
Stress Ulcer
Stress Ulcer
Signup and view all the flashcards
Thrombotic Phase of DIC
Thrombotic Phase of DIC
Signup and view all the flashcards
Bleeding Phase of DIC
Bleeding Phase of DIC
Signup and view all the flashcards
D-dimer
D-dimer
Signup and view all the flashcards
Medications that hide patient response
Medications that hide patient response
Signup and view all the flashcards
Interventions that cause patient discomfort
Interventions that cause patient discomfort
Signup and view all the flashcards
Educating Family Members about the Dying Process
Educating Family Members about the Dying Process
Signup and view all the flashcards
Resolving Conflict through Dialogue
Resolving Conflict through Dialogue
Signup and view all the flashcards
Study Notes
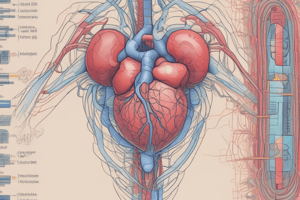
Sepsis/Septic Shock: Epidemiology
- Incidence of sepsis in the US: ~1.7 million adults annually; ~270,000 deaths annually
- Increasing incidence attributed to factors like:
- Increased invasive procedures and monitoring
- Growing aging population
- Rise in chemotherapy/immunosuppressive use
- Growing antimicrobial resistance
- Mortality is decreasing due to improved treatment
- Gram-positive infections more common but gram-negative still substantial
- Fungal infections increasing but still less frequent than bacterial infections
Sepsis/Septic Shock: Definitions and Pathophysiology
- Sepsis 3 definition: life-threatening organ dysfunction caused by a deregulated host response to infection.
- Septic shock: circulatory and metabolic abnormalities, substantially increasing mortality.
- Potential complications: DIC (disseminated intravascular coagulopathy), MODS (multiple organ dysfunction syndrome)
- Pathophysiology: initial immune response activation (innate immunity)
- Mobilization of macrophages & neutrophils
- Pro-inflammatory cytokine activation
- Complement activation
- Coagulation activation (fibrin mesh for localization)
- Sepsis results from an amplified and uncontrolled systemic inflammatory response
- Normal deactivation process impaired, leading to excessive pro-inflammatory cytokines
- Inflammatory damage to blood vessels, vasodilation, and increased permeability
- Contributing factors: endotoxins and exotoxins from invading organisms (gram-negative & gram-positive)
- Coagulation cascade dysfunction: significant fibrin deposition, impaired fibrinolysis (breakdown of clots), decreased protein C and antithrombin III levels
- Microvascular clots, reduced blood flow and organ dysfunction
Sepsis/Septic Shock: Clinical Manifestations
- Early (hyperdynamic/warm): tachycardia, bounding pulses, warm flushed skin, fever, potentially normal blood pressure (compensatory response).
- Early signs of decreased organ perfusion (confusion, decreased urine output).
- Increased cardiac output (as long as adequate fluid resuscitation).
- Low filling pressures (CVP, PAOP).
- Systemic vascular resistance (SVR) is low due to vasodilation.
- Late (hypodynamic/cold): cool, pale skin, weak/thready pulses, hypothermia, persistent tachycardia,
- Low blood pressure.
- Severe end-organ hypoperfusion (lethargy/coma, anuria).
- Decreased cardiac output.
- Variable filling pressures (dependent on fluid resuscitation).
- SVR may remain low or increase with compensation & drug therapy.
- Low venous oxygen levels (reflecting inadequate tissue oxygen delivery)
Sepsis/Septic Shock: Interprofessional Management
- Surviving Sepsis campaign: standardized care to reduce sepsis mortality.
- Diagnosis: general indicators of infection (fever, WBC count changes in BP/RR/HR), specific infection signs, lab tests (CBC, metabolic panels, cultures), imaging (radiographs, CT, MRI)
- Severity assessment: NEWS, MEWS, SOFA scores
- ICU admission within 6 hours for those needing it
Sepsis/Septic Shock: Medical Management
- Prevention first: hand hygiene, aseptic technique, and minimizing invasive procedures.
- Bundle of care (1 hour): fluid resuscitation, blood work (lactate, blood cultures), antibiotics (after cultures)
- Fluid resuscitation: balanced crystalloid solution, 30 mL/kg over 3 hours
- Vasopressors: norepinephrine as first line if fluids are insufficient
- Antibiotics: within 1 hour of diagnosis, guided by cultures
- Corticosteroids: low-dose only in non-responsive patients to fluid & vasopressors
Sepsis/Septic Shock: Ongoing Monitoring
- Frequent vital signs, peripheral perfusion, and mental status checks.
- Cultures and blood testing (WBC, lactate).
- Hemodynamic monitoring (CVP/PAOP, SvO2/ScvO2); PA catheter use is not standard.
- Cardiac response evaluation (echocardiography after passive leg raise) .
- Capillary refill time monitoring
Sepsis/Septic Shock: Withdrawal of Life Support
- Patient/family discussion fundamental for withdrawal decisions.
- Using “withdrawal of support” instead of “withdrawal of care” to reduce anxiety.
- DNR order.
- Gradual or immediate discontinuation of ventilation, with comfort measures.
- Pain and sedation management driven by patient response, not a schedule
- Discontinuing non-comfort interventions
Sepsis/Septic Shock: Complication - Stress Ulcers
- Common in ICU patients, risk factors include: Mechanical ventilation, coagulopathy, shock, sepsis, major trauma, and head injury.
- Prophylaxis: enteral PPIs or H2 blockers, IV options for those unable to take enteral drugs
Sepsis/Septic Shock: Complication - Disseminated Intravascular Coagulopathy (DIC)
- Enhanced coagulation from procoagulant release during the inflammatory response of sepsis.
- Two phases: thrombotic (clotting) and bleeding, often occurring simultaneously.
- Thrombotic phase leads to microvascular clots, ischemia, and necrosis.
- Bleeding phase caused by impaired fibrinolysis and excessive fibrin degradation products.
- Diagnosis through clinical symptoms and lab tests (decreased fibrinogen, increased fibrin degradation products, D-dimer, decreased platelets, prolonged PT/aPTT, decreased antithrombin III)
- Management: focus on treating underlying sepsis, hypotentions, hypoxemia, and metabolic acidosis. Fluid support, blood products, and clotting factors may be required.
Sepsis/Septic Shock: Complication - Multiple Organ Dysfunction Syndrome (MODS)
- Multifaceted cause:
- Accelerated apoptosis (programmed cell death)
- Widespread vascular endothelium damage
- Microvascular dysfunction
- Enhanced coagulation
- Hypermetabolism
- Mitochondrial toxicity
- Progression typically starts in lungs, then renal, hepatic, and GI systems.
- High mortality rates, especially when 3+ organ systems are affected.
Sepsis/Septic Shock: Nursing Management
- Assessment: neurological status, vital signs, hemodynamic readings, urine output, skin, bleeding.
- Nursing Diagnoses: altered tissue perfusion, excessive clotting, bleeding.
- Interventions: hand hygiene, oxygen, fluid replacement, monitoring lactate, labs (cultures, ABGs, coagulation studies).
- Administer antibiotics after cultures.
- Vasopressors for inadequate blood pressure
- Oral care, nutrition, supportive care, turning to prevent complications.
- Teaching: sepsis prevention, importance of hand hygiene, patient comfort
Sepsis/Septic Shock: Evaluating Outcomes
- Early recognition & swift treatment (antibiotics, fluids)
- Maintaining cardiac output
- Monitor hemodynamics, frequent labs
- Supportive care to prevent complications.
- Evaluating response in blood pressure, cardiac output, and tissue perfusion.
Sepsis/Septic Shock: Delirium Management (Box 14.1)
- Delirium: altered consciousness, impaired focus and memory.
- Common in ICU
- Management: -Orientation aids -Cognitive stimulation -Sleep-wake cycle support -Minimize restraints -Avoid problematic medications (benzodiazepines, opiates, antihistamines)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.