Podcast
Questions and Answers
What is the primary characteristic of bronchiectasis?
What is the primary characteristic of bronchiectasis?
- Temporary dilation of bronchi
- Obstruction of airways due to mucus
- Altered central blood flow
- Permanent dilation of bronchi and bronchioles (correct)
Which of the following conditions is NOT a predisposing factor for bronchiectasis?
Which of the following conditions is NOT a predisposing factor for bronchiectasis?
- Chronic GVHD
- Postinfectious conditions
- Cystic fibrosis
- Acute respiratory distress syndrome (correct)
What dysfunction is most commonly associated with primary ciliary dyskinesia?
What dysfunction is most commonly associated with primary ciliary dyskinesia?
- Overactive cilia leading to excess mucus clearance
- Immotile cilia due to dynein arm mutations (correct)
- Excessively mobile cilia causing lung damage
- Abnormal cilia with improved airflow
Which imaging method is most effective for visualizing bronchiectasis?
Which imaging method is most effective for visualizing bronchiectasis?
What is a common consequence of impaired ciliary function in conditions like cystic fibrosis?
What is a common consequence of impaired ciliary function in conditions like cystic fibrosis?
In bronchiectasis, what causes permanent dilation of the bronchi and bronchioles?
In bronchiectasis, what causes permanent dilation of the bronchi and bronchioles?
What condition is associated with situs inversus in addition to bronchiectasis?
What condition is associated with situs inversus in addition to bronchiectasis?
Which of the following is a common feature observed in patients with cystic fibrosis?
Which of the following is a common feature observed in patients with cystic fibrosis?
Which type of chronic bronchitis is characterized by a productive cough without airflow obstruction?
Which type of chronic bronchitis is characterized by a productive cough without airflow obstruction?
What is the primary cause of chronic bronchitis?
What is the primary cause of chronic bronchitis?
What does a Reid index greater than 0.5 indicate?
What does a Reid index greater than 0.5 indicate?
Which histological feature is NOT associated with bronchiectasis?
Which histological feature is NOT associated with bronchiectasis?
Which histological change is typical of chronic bronchitis?
Which histological change is typical of chronic bronchitis?
What is the classic biochemical abnormality observed in cystic fibrosis?
What is the classic biochemical abnormality observed in cystic fibrosis?
Which symptom is least likely associated with asthma?
Which symptom is least likely associated with asthma?
Which factor is least likely to contribute to the pathogenesis of chronic bronchitis?
Which factor is least likely to contribute to the pathogenesis of chronic bronchitis?
Which of the following complications is NOT typically associated with cystic fibrosis?
Which of the following complications is NOT typically associated with cystic fibrosis?
In chronic asthmatic bronchitis, what occurs alongside hyperreactive airways?
In chronic asthmatic bronchitis, what occurs alongside hyperreactive airways?
What primary defect is responsible for the symptoms of cystic fibrosis?
What primary defect is responsible for the symptoms of cystic fibrosis?
Which mechanism contributes to the recurrent pulmonary infections seen in cystic fibrosis?
Which mechanism contributes to the recurrent pulmonary infections seen in cystic fibrosis?
What does chronic inflammation in chronic bronchitis primarily lead to?
What does chronic inflammation in chronic bronchitis primarily lead to?
In the context of bronchiectasis, which pathogen is most commonly associated with chronic infections?
In the context of bronchiectasis, which pathogen is most commonly associated with chronic infections?
How does cystic fibrosis primarily affect the pancreas?
How does cystic fibrosis primarily affect the pancreas?
What role does the CFTR protein play in cystic fibrosis pathogenesis?
What role does the CFTR protein play in cystic fibrosis pathogenesis?
Flashcards
Bronchiectasis
Bronchiectasis
Permanent dilation of bronchi and bronchioles due to destruction of smooth muscle and supporting elastic tissue, often associated with chronic necrotizing infections.
Conditions Predisposing to Bronchiectasis
Conditions Predisposing to Bronchiectasis
Cystic fibrosis, primary ciliary dyskinesia, immunodeficiency states, necrotizing bacterial pneumonias, bronchial obstruction (tumor, foreign bodies), Rheumatoid arthritis, SLE, IBD, Chronic GVHD.
Primary Ciliary Dyskinesia
Primary Ciliary Dyskinesia
Autosomal recessive disorder with defects in ciliary motor proteins, leading to bronchiectasis, sinusitis, and male sterility.
Kartagener Syndrome
Kartagener Syndrome
Signup and view all the flashcards
Bronchiectasis Histology
Bronchiectasis Histology
Signup and view all the flashcards
Cystic Fibrosis Pathogenesis
Cystic Fibrosis Pathogenesis
Signup and view all the flashcards
Sweat Chloride Test (Cystic Fibrosis)
Sweat Chloride Test (Cystic Fibrosis)
Signup and view all the flashcards
Simple Chronic Bronchitis
Simple Chronic Bronchitis
Signup and view all the flashcards
Chronic Asthmatic Bronchitis
Chronic Asthmatic Bronchitis
Signup and view all the flashcards
Obstructive Chronic Bronchitis
Obstructive Chronic Bronchitis
Signup and view all the flashcards
Pathogenesis of Chronic Bronchitis
Pathogenesis of Chronic Bronchitis
Signup and view all the flashcards
Mucus Gland Hyperplasia
Mucus Gland Hyperplasia
Signup and view all the flashcards
Reid Index
Reid Index
Signup and view all the flashcards
Goblet Cell Metaplasia
Goblet Cell Metaplasia
Signup and view all the flashcards
Chronic Bronchitis: Histopathology
Chronic Bronchitis: Histopathology
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
Asthma - Diagnosis
Asthma - Diagnosis
Signup and view all the flashcards
Study Notes
Papanicolaou Stain
- Reddish core with a fuzzy margin
- Cells attached secondarily
- Arrow points at a macrophage
Charcot-Leyden Crystals
- Eosinophils
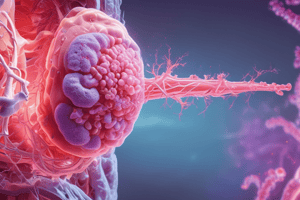
Bronchiectasis
- Permanent dilation of bronchi and bronchioles
- Destruction of smooth muscle and supporting elastic tissue
- Results from or is associated with chronic necrotizing infections
- Not a primary disorder
Conditions Predisposing to Bronchiectasis
- Congenital or hereditary conditions:
- Cystic fibrosis
- 1° ciliary dyskinesia (immotile cilia syndrome/Kartagener syndrome)
- Immunodeficiency states associated with recurrent bacterial infections (i.e., immunoglobulin deficiencies)
- Postinfectious conditions:
- Necrotizing bacterial pneumonias (especially with Staph aureus, Klebsiella, or TB in endemic regions)
- Bronchial obstruction due to tumor, foreign bodies
- Other conditions: Rheumatoid arthritis, SLE, IBD, chronic GVHD
Pathogenesis of Bronchiectasis
- Cases due to nonspecific obstruction and infection:
- Both are necessary for full-blown lesions
- Either can be the initiating factor
- Normal clearing mechanisms are impaired:
- Most readily apparent in cystic fibrosis
- Thick viscid mucus obstructs airways and predisposes to infections
- Most readily apparent in cystic fibrosis
- Primary ciliary dyskinesia (immotile cilia syndrome):
- Autosomal recessive/variable penetrance
- Defects in ciliary motor proteins (dynein arm mutations)
- Kartagener syndrome: situs inversus, bronchiectasis, sinusitis
- Bronchiectasis
- Sterility in males: sperm dysmotility
- Poorly functioning cilia: Retention of secretions --> recurrent infections --> bronchiectasis
Immotile Cilia Syndrome
- Normal dynein arms
- Immotile cilia syndrome
Bronchiectasis: CT Scan and Gross Specimen
- Dilated airways on the CT scan in longitudinal section (arrowhead) and cross section (arrow)
- Cut surface of lung with distended peripheral bronchi filled with mucopurulent secretions (white arrow) in cystic fibrosis
Bronchiectasis: Gross
- Bronchiectasis tends to be localized with disease processes
- Widespread bronchiectasis is typical in patients with cystic fibrosis
Bronchiectasis: Histology
- Desquamation of surface epithelium with ulceration
- Destruction of cartilage and smooth muscle
- Dilatation of airways
- Chronic inflammation and fibrosis of wall
- Intraluminal purulent material
Cystic Fibrosis Pathogenesis
- Disorder of epithelial ion transport affecting fluid secretion in exocrine glands and epithelial linings of the respiratory tract, GI tract, and reproductive tract
- Abnormally viscid mucous secretions --> airway and the pancreatic duct blockages
- Leading to recurrent and chronic pulmonary infections and pancreatic insufficiency
- Most common (incidence 1:2500 live births) lethal genetic disease in whites (carrier freq 1:20)
- Classic biochemical abnormality: high sodium chloride level in sweat (sweat chloride test)
- Primary defect is reduced production (or abnormal function) of an epithelial chloride channel protein encoded by the CF transmembrane conductance regulator (CFTR) gene
- In sweat duct, result is increased sodium and chloride in sweat
- In epithelium of respiratory and GI tract, decreased chloride secretion with increased sodium and water reabsorption in airways results in dehydrated mucus layer, defective mucociliary action, and mucous plugging
- Cystic fibrosis affects several organs:
- Pancreas: Mild to most severe
- Exocrine gland atrophy and fibrosis
- Impaired fat absorption
- Vitamin A deficiency
- Small intestine: Mucus plugs --> meconium ileus
- Pulmonary: Thick viscid mucous of submucosal glands --> sinusitis, mucous plugging of bronchioles --> bronchiectasis --> abscesses
- Staph aureus, Hemophilus influenzae, and Pseudomonas aeruginosa are the most common organisms with Burkholderia cepacia (formerly Pseudomonas cepacia) increasing
- Pancreas: Mild to most severe
Chronic Bronchitis Types
- Simple chronic bronchitis: Productive cough but no physiologic evidence of airflow obstruction
- Chronic asthmatic bronchitis: Hyperreactive airways with intermittent bronchospasm and wheezing
- Obstructive chronic bronchitis: Develop chronic airflow obstruction
- Usually have associated emphysema
Pathogenesis of Chronic Bronchitis
- Hallmark is hypersecretion of mucus beginning in large airways
- Most important cause is cigarette smoking, followed by other environmental pollutants
- Histologic findings:
- Mucus gland hyperplasia: Increased size of glands
- Reid index = ratio of thickness of mucous gland layer to the thickness of the wall between the epithelium and the cartilage (NL = 0.4)
- Goblet cell metaplasia: Often seen
- Inflammatory infiltration of bronchiolar walls: Lymphocytes, macrophages, neutrophils, no eosinophils
- Fibrosis of the bronchiolar wall: Older patients
- May see squamous metaplasia or dysplasia: Especially with smoking
- Mucus gland hyperplasia: Increased size of glands
Evolution of Chronic Bronchitis and Emphysema
- Both chronic bronchitis and emphysema can result from different pathways
- Either one can predominate
Chronic Bronchitis: Histopathology
- Chronic inflammation
Reid Index
- Ratio of thickness of submucosal mucus gland layer to thickness of bronchial wall between epithelium and cartilage
- Normally = 0.4 or less
- Increased (>0.5) in chronic bronchitis proportionally to the duration and severity of disease
Asthma
- A chronic disorder of the airways
- Usually an immunologic reaction marked by:
- Episodic bronchoconstriction due to increased airway sensitivity to varied stimuli
- Inflammation of bronchial walls
- Increased mucus secretion
- Presents with recurrent episodes of wheezing, breathlessness, chest tightness, and cough, especially at night and/or in the early morning
- Symptoms are usually associated with:
- Exposure to allergens (pollen, dust mites, animal dander, molds)
- Viral infections (respiratory syncytial virus, rhinovirus)
- Irritants (cigarette smoke, air pollution, cold air, exercise)
- Drugs (aspirin, NSAIDs)
Asthma - Diagnosis
- Clinical history and examination: History of recurrent wheezing and shortness of breath
- Spirometry: To assess airflow obstruction
- Peak expiratory flow rate: Measures the maximum speed of air that can be forcibly exhaled
- Methacholine challenge test: Used to assess airway hyperresponsiveness
- Allergy testing: Skin prick test, blood tests
- Chest x-ray: To rule out other lung diseases
- Blood tests: To measure eosinophil count and other inflammatory markers
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.