Podcast
Questions and Answers
What is the primary benefit of NIV in the long-term treatment of respiratory failure?
What is the primary benefit of NIV in the long-term treatment of respiratory failure?
- Reduce the risk of lung transplantation in patients with neuromuscular disease
- Improve lung function in patients with cystic fibrosis
- Relieve morning headache and fatigue in patients with central alveolar hypoventilation (correct)
- Increase oxygen saturation in patients with spinal deformity
What is the primary indication for daytime NIV in patients with advanced lung disease?
What is the primary indication for daytime NIV in patients with advanced lung disease?
- Severe fatigue and headache
- Presence of pulmonary infection
- Elevated PaCO2 levels during sleep
- Muscular dystrophies or cystic fibrosis (correct)
Why is single-lung transplantation not recommended for patients with cystic fibrosis?
Why is single-lung transplantation not recommended for patients with cystic fibrosis?
- Inadequate improvement in lung function
- High risk of rejection
- Risk of cross-infection in the context of post-transplant immunosuppression (correct)
- Insufficient data on long-term outcomes
What is the median survival for double lung transplantation according to the International Society for Heart and Lung Transplantation?
What is the median survival for double lung transplantation according to the International Society for Heart and Lung Transplantation?
In which patients is lung transplantation an established treatment?
In which patients is lung transplantation an established treatment?
Flashcards
Respiratory Failure
Respiratory Failure
A condition where the lungs fail to maintain normal oxygen and carbon dioxide levels in the blood.
Type I Respiratory Failure
Type I Respiratory Failure
Occurs when the lung can't ventilate properly, leading to low oxygen and high carbon dioxide in the blood.
Type II Respiratory Failure
Type II Respiratory Failure
Occurs when there's a widespread problem with how the lungs exchange gases, leading to low oxygen and high carbon dioxide in the blood.
Chronic Respiratory Failure
Chronic Respiratory Failure
Signup and view all the flashcards
Lung Transplantation
Lung Transplantation
Signup and view all the flashcards
Study Notes
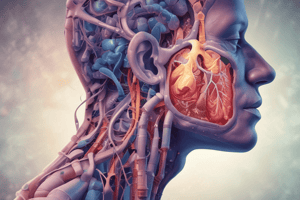
Respiratory Failure
- Respiratory failure occurs when pulmonary gas exchange fails to maintain normal arterial oxygen and carbon dioxide levels.
- Classified into types I and II, based on the absence or presence of hypercapnia (raised PaCO2).
Type I Respiratory Failure
- Occurs when disease impairs ventilation of part of a lung, resulting in hypoxic and CO2-laden blood entering the pulmonary veins.
- Increased ventilation of neighboring regions of normal lung can correct arterial CO2 to normal, but cannot augment oxygen uptake.
- Examples: asthma, pneumonia.
Type II Respiratory Failure
- Occurs when there is arterial hypoxia with hypercapnia, seen in conditions that cause generalized, severe ventilation-perfusion mismatch.
- Examples: conditions that reduce total ventilation, such as neuromuscular mechanisms of ventilation.
Management of Acute Respiratory Failure
- Type I: prompt diagnosis and management of the underlying cause, oxygen administration to maintain SaO2 (94%-98%).
- Type II: prompt diagnosis and management of the underlying cause, oxygen administration to maintain SaO2 (88%-92%) or safe PaO2 (>7.0 kPa or 52 mmHg) without increasing PaCO2 and acidosis.
Management of Chronic and 'Acute on Chronic' Type II Respiratory Failure
- Most common cause of chronic type II respiratory failure is severe COPD.
- Management: identify and treat the precipitating condition, achieve safe PaO2 (>7.0 kPa or 52 mmHg) without increasing PaCO2 and acidosis.
- Non-invasive ventilation (NIV) may be beneficial in conscious patients with adequate respiratory drive.
- Intubation and ventilation may be necessary for patients who are drowsy and have low respiratory drive.
Home Ventilation for Chronic Respiratory Failure
- Indications: spinal deformity, neuromuscular disease, central alveolar hypoventilation, and some patients with advanced lung disease (e.g. COPD and cystic fibrosis).
- Diagnosis: morning headache and fatigue, revealed by sleep studies or morning blood gas analysis.
- Treatment: home-based NIV overnight, often sufficient to restore daytime PCO2 to normal and relieve fatigue and headache.
Lung Transplantation
- Established treatment for carefully selected patients with advanced lung disease unresponsive to medical treatment.
- Contraindications: patients with chronic bilateral pulmonary infection, such as cystic fibrosis and bronchiectasis.
- Prognosis: improving steadily with modern immunosuppressive drugs, median survival for double lung transplantation is 7.8 years.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.