Podcast
Questions and Answers
What is the primary mechanism by which pulmonary edema impairs gas exchange in the lungs?
What is the primary mechanism by which pulmonary edema impairs gas exchange in the lungs?
- Reduced alveolar surface area due to inflammation.
- Increased thickness of the alveolar-capillary membrane due to fluid accumulation. (correct)
- Destruction of alveolar walls causing air trapping.
- Bronchoconstriction leading to decreased airflow.
A patient with pulmonary edema is prescribed furosemide (Lasix). What is the primary intended effect of this medication?
A patient with pulmonary edema is prescribed furosemide (Lasix). What is the primary intended effect of this medication?
- To dilate the bronchioles and improve airflow.
- To reduce preload by promoting diuresis. (correct)
- To improve cardiac contractility.
- To reduce anxiety and promote relaxation.
Which of the following assessment findings would be most indicative of pulmonary edema?
Which of the following assessment findings would be most indicative of pulmonary edema?
- Gradual onset of dyspnea with wheezing.
- Pink, frothy sputum and severe dyspnea. (correct)
- Sudden, sharp chest pain radiating to the arm.
- Productive cough with thick, green sputum.
A patient with a history of left-sided heart failure develops pulmonary edema. Which of the following pathophysiological processes is the primary cause of the edema in this scenario?
A patient with a history of left-sided heart failure develops pulmonary edema. Which of the following pathophysiological processes is the primary cause of the edema in this scenario?
Which intervention is most important for the nurse to implement when caring for a patient with pulmonary edema?
Which intervention is most important for the nurse to implement when caring for a patient with pulmonary edema?
Which of the following medications is used in the treatment of pulmonary edema to reduce anxiety and promote vasodilation?
Which of the following medications is used in the treatment of pulmonary edema to reduce anxiety and promote vasodilation?
A patient with pulmonary edema is being treated with oxygen therapy. Despite receiving high-flow oxygen, the patient's oxygen saturation remains low. What condition should the nurse suspect?
A patient with pulmonary edema is being treated with oxygen therapy. Despite receiving high-flow oxygen, the patient's oxygen saturation remains low. What condition should the nurse suspect?
What is the most common cause of a pulmonary embolism?
What is the most common cause of a pulmonary embolism?
A patient with a pulmonary embolism is started on heparin. What is the primary mechanism of action of heparin in this situation?
A patient with a pulmonary embolism is started on heparin. What is the primary mechanism of action of heparin in this situation?
Which of the following clinical manifestations is most indicative of a pulmonary embolism?
Which of the following clinical manifestations is most indicative of a pulmonary embolism?
A patient with a history of deep vein thrombosis (DVT) is at increased risk for pulmonary embolism. Which of the following interventions is most important to prevent PE in this patient?
A patient with a history of deep vein thrombosis (DVT) is at increased risk for pulmonary embolism. Which of the following interventions is most important to prevent PE in this patient?
A patient is receiving warfarin for long-term anticoagulation following a pulmonary embolism. Which laboratory value is most important to monitor to ensure therapeutic anticoagulation?
A patient is receiving warfarin for long-term anticoagulation following a pulmonary embolism. Which laboratory value is most important to monitor to ensure therapeutic anticoagulation?
A patient with a massive pulmonary embolism is hypotensive and unresponsive to traditional treatments. Which intervention is most likely to be considered in this situation?
A patient with a massive pulmonary embolism is hypotensive and unresponsive to traditional treatments. Which intervention is most likely to be considered in this situation?
Following a motor vehicle accident, a patient presents with chest pain, dyspnea, and decreased breath sounds on the left side. Which of the following conditions should the nurse suspect?
Following a motor vehicle accident, a patient presents with chest pain, dyspnea, and decreased breath sounds on the left side. Which of the following conditions should the nurse suspect?
A patient with a flail chest is experiencing severe pain and difficulty breathing. What is the priority intervention for this patient?
A patient with a flail chest is experiencing severe pain and difficulty breathing. What is the priority intervention for this patient?
A patient with a tension pneumothorax is showing signs of hemodynamic instability. Which of the following assessment findings would be most concerning?
A patient with a tension pneumothorax is showing signs of hemodynamic instability. Which of the following assessment findings would be most concerning?
A patient with multiple rib fractures is at risk for developing pneumonia. Which intervention is most important to prevent this complication?
A patient with multiple rib fractures is at risk for developing pneumonia. Which intervention is most important to prevent this complication?
A patient involved in a motor vehicle accident is diagnosed with a pulmonary contusion. What is the primary concern related to this injury?
A patient involved in a motor vehicle accident is diagnosed with a pulmonary contusion. What is the primary concern related to this injury?
What is the primary purpose of a chest tube?
What is the primary purpose of a chest tube?
In a three-chamber chest tube drainage system, what is the function of the water seal chamber?
In a three-chamber chest tube drainage system, what is the function of the water seal chamber?
A nurse observes continuous bubbling in the water seal chamber of a chest tube drainage system. What does this indicate?
A nurse observes continuous bubbling in the water seal chamber of a chest tube drainage system. What does this indicate?
What should the nurse do if a chest tube becomes accidentally disconnected from the drainage system?
What should the nurse do if a chest tube becomes accidentally disconnected from the drainage system?
Which assessment finding would indicate the need for a chest tube insertion?
Which assessment finding would indicate the need for a chest tube insertion?
What is the significance of the PaO2/FiO2 (P/F) ratio in assessing patients with acute respiratory failure?
What is the significance of the PaO2/FiO2 (P/F) ratio in assessing patients with acute respiratory failure?
A patient with acute respiratory failure has a PaCO2 of 60 mmHg and a pH of 7.25. What type of respiratory failure is the patient experiencing?
A patient with acute respiratory failure has a PaCO2 of 60 mmHg and a pH of 7.25. What type of respiratory failure is the patient experiencing?
Which of the following conditions is most likely to cause ventilation (hypercarbic) respiratory failure?
Which of the following conditions is most likely to cause ventilation (hypercarbic) respiratory failure?
A patient in acute respiratory failure is receiving oxygen therapy. What is the primary goal of oxygen therapy in this situation?
A patient in acute respiratory failure is receiving oxygen therapy. What is the primary goal of oxygen therapy in this situation?
Which of the following clinical manifestations is a late sign of acute respiratory failure?
Which of the following clinical manifestations is a late sign of acute respiratory failure?
What is the primary difference between acute respiratory failure (ARF) and acute respiratory distress syndrome (ARDS)?
What is the primary difference between acute respiratory failure (ARF) and acute respiratory distress syndrome (ARDS)?
A patient with ARDS has a PaO2/FiO2 ratio of 150. How would you interpret this value?
A patient with ARDS has a PaO2/FiO2 ratio of 150. How would you interpret this value?
Which of the following pathophysiological changes is characteristic of ARDS?
Which of the following pathophysiological changes is characteristic of ARDS?
A patient with ARDS is receiving mechanical ventilation. What strategy is often used to minimize further lung injury?
A patient with ARDS is receiving mechanical ventilation. What strategy is often used to minimize further lung injury?
A patient with ARDS develops hypotension and tachycardia. Which of the following interventions is most appropriate?
A patient with ARDS develops hypotension and tachycardia. Which of the following interventions is most appropriate?
Which of the following assessment findings is most indicative of ARDS?
Which of the following assessment findings is most indicative of ARDS?
A patient is prescribed nitroglycerin for pulmonary edema. What is the expected outcome of this medication?
A patient is prescribed nitroglycerin for pulmonary edema. What is the expected outcome of this medication?
When caring for a patient with a pulmonary embolism and prescribed anticoagulants, what nursing intervention is crucial for patient safety?
When caring for a patient with a pulmonary embolism and prescribed anticoagulants, what nursing intervention is crucial for patient safety?
A patient with chest trauma has a chest tube inserted. Which finding requires immediate intervention?
A patient with chest trauma has a chest tube inserted. Which finding requires immediate intervention?
What should the nurse educate the patient with rib fractures about to prevent pneumonia?
What should the nurse educate the patient with rib fractures about to prevent pneumonia?
A patient in acute respiratory failure is prescribed corticosteroids. What is the primary purpose of these medications?
A patient in acute respiratory failure is prescribed corticosteroids. What is the primary purpose of these medications?
Flashcards
Pulmonary Edema
Pulmonary Edema
Results when the left ventricle fails, increasing lung pressure, leading to fluid leakage into the airways.
Orthopnea
Orthopnea
Shortness of breath, often when lying flat.
Paroxysmal Nocturnal Dyspnea
Paroxysmal Nocturnal Dyspnea
Sudden nighttime breathlessness.
Tachypnea
Tachypnea
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Cardiogenic causes of Pulmonary Edema
Cardiogenic causes of Pulmonary Edema
Signup and view all the flashcards
Non-cardiogenic causes of Pulmonary Edema
Non-cardiogenic causes of Pulmonary Edema
Signup and view all the flashcards
Furosemide (Lasix)
Furosemide (Lasix)
Signup and view all the flashcards
Nitroglycerin
Nitroglycerin
Signup and view all the flashcards
Morphine
Morphine
Signup and view all the flashcards
Inotropic agents
Inotropic agents
Signup and view all the flashcards
Pulmonary Embolism (PE)
Pulmonary Embolism (PE)
Signup and view all the flashcards
Petechiae
Petechiae
Signup and view all the flashcards
Causes of Pulmonary Embolism
Causes of Pulmonary Embolism
Signup and view all the flashcards
Sudden Dyspnea
Sudden Dyspnea
Signup and view all the flashcards
Hemoptysis
Hemoptysis
Signup and view all the flashcards
Heparin Use
Heparin Use
Signup and view all the flashcards
Warfarin antidote
Warfarin antidote
Signup and view all the flashcards
Pulmonary Embolism Labs
Pulmonary Embolism Labs
Signup and view all the flashcards
Motor vehicle accidents
Motor vehicle accidents
Signup and view all the flashcards
Tension Pneumothorax
Tension Pneumothorax
Signup and view all the flashcards
Flail Chest
Flail Chest
Signup and view all the flashcards
Edema in Alveoli Symptoms
Edema in Alveoli Symptoms
Signup and view all the flashcards
Chest Tube Insertion
Chest Tube Insertion
Signup and view all the flashcards
Deep Breathing Exercises
Deep Breathing Exercises
Signup and view all the flashcards
Chest Tube Purpose
Chest Tube Purpose
Signup and view all the flashcards
Three-Chamber Drainage System
Three-Chamber Drainage System
Signup and view all the flashcards
Pleural Effusion
Pleural Effusion
Signup and view all the flashcards
Pulmonary Empyema
Pulmonary Empyema
Signup and view all the flashcards
Asymmetrical Breath Sounds
Asymmetrical Breath Sounds
Signup and view all the flashcards
Water seal chamber bubbling
Water seal chamber bubbling
Signup and view all the flashcards
Chest tube disconnects
Chest tube disconnects
Signup and view all the flashcards
Compromised Drainage System
Compromised Drainage System
Signup and view all the flashcards
Accidental Removal of Chest Tube
Accidental Removal of Chest Tube
Signup and view all the flashcards
Acute Respiratory Failure (ARF)
Acute Respiratory Failure (ARF)
Signup and view all the flashcards
Oxygenation Failure
Oxygenation Failure
Signup and view all the flashcards
Ventilation Failure
Ventilation Failure
Signup and view all the flashcards
Refractory Hypoxemia
Refractory Hypoxemia
Signup and view all the flashcards
Acute Respiratory Distress Syndrome
Acute Respiratory Distress Syndrome
Signup and view all the flashcards
Study Notes
-
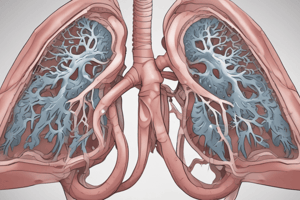
Pulmonary Edema
- Occurs when the left ventricle fails to eject sufficient blood, leading to increased pressure in the lungs.
- Increased pressure causes fluid leakage across pulmonary capillaries into the lung airways.
Manifestations of Pulmonary Edema
- Pink, frothy sputum
- Dyspnea (shortness of breath)
- Orthopnea (difficulty breathing when lying flat)
- Paroxysmal nocturnal dyspnea (sudden nighttime breathlessness)
- Cough with frothy, pink sputum
- Tachypnea (rapid breathing)
- Tachycardia (rapid heart rate)
- Cyanosis (bluish discoloration of the skin)
- Crackles (rales) on lung auscultation
Risk Factors for Pulmonary Edema
- Cardiogenic causes include left-sided heart failure, acute myocardial infarction, mitral valve disease, and hypertension.
- Non-cardiogenic causes include pneumonia, inhalation injury, sepsis, airway obstruction, and high altitude.
Medications for Pulmonary Edema
- Furosemide (Lasix) is used for diuresis.
- Nitroglycerin is used for vasodilation to lower high systolic blood pressure.
- Morphine is used for anxiety and vasodilation.
- ACE inhibitors or ARBs are used for heart failure management.
Treatment for Pulmonary Edema
- Oxygen therapy is administered to maintain adequate oxygen saturation.
- Diuretics are used to reduce fluid overload.
- Vasodilators are used to decrease afterload.
- Inotropic agents are used to improve cardiac output.
- Addressing the underlying cause (e.g., treating heart failure or infection) is crucial.
- Chest tube placement may be necessary.
Nursing Interventions for Pulmonary Edema
- Monitor vital signs and oxygen saturation.
- Assess lung sounds for crackles.
- Administer prescribed medications.
- Position the patient upright to facilitate breathing.
- Provide emotional support to reduce anxiety.
Safety and Nursing Care for Pulmonary Edema
- Implement fall precautions.
- Educate the patient on fluid and sodium restrictions.
- Monitor for signs of electrolyte imbalances.
- Encourage smoking cessation.
Pulmonary Embolism (PE)
- A collection of particulate matter enters venous circulation and lodges in pulmonary vessels.
- A blood clot is the most common cause, but fat emboli can occur with long bone breaks, indicated by petechiae.
Risk Factors for PE
- Prolonged immobility (e.g., bed rest, long flights)
- Recent surgery, especially orthopedic procedures
- Central venous catheter
- History of deep vein thrombosis (DVT)
- Cancer
- Smoking
- Obesity
- Use of estrogen-based contraceptives
- Pregnancy and postpartum period
- Age over 60
Clinical Manifestations of PE
- Sudden onset of dyspnea
- Pleuritic chest pain
- Hemoptysis (coughing up blood)
- Tachypnea
- Tachycardia
- Hypotension
- Anxiety
Treatments for PE
- Anticoagulation therapy (e.g., heparin, warfarin) is common.
- Thrombolytic therapy is used in severe cases.
- Surgical embolectomy may be indicated.
- Inferior vena cava (IVC) filter placement is used for recurrent PE.
Medications for PE
- Heparin is used for immediate anticoagulation; protamine sulfate is the antidote.
- Warfarin is used for long-term anticoagulation; vitamin K is the antidote.
- FFP (Fresh Frozen Plasma) is used in some cases.
- Direct oral anticoagulants (DOACs) are used as alternatives.
- Tissue plasminogen activator (tPA) is used for thrombolysis.
Nursing Interventions for PE
- Monitor for signs of bleeding.
- Assess respiratory status and oxygenation.
- Administer prescribed anticoagulants and thrombolytics.
- Educate the patient on medication adherence and bleeding precautions.
Labs for PE
- Low PACO2 on ABG, elevated troponin, BNP, and D-dimer (for clotting)
Safety and Basic Care for PE
- Implement fall precautions.
- Avoid invasive procedures that may cause bleeding.
- Encourage early ambulation to prevent DVT.
- Provide emotional support to reduce anxiety.
Chest Trauma
- Motor vehicle accidents often cause pulmonary contusion.
Risk Factors for Chest Trauma
- Blunt force to chest
- Pneumothorax, hemothorax, tension pneumothorax
- Rib fractures
- Flail chest
- Occupational accidents
Clinical Manifestations of Chest Trauma
- Chest pain
- Dyspnea
- Cyanosis
- Decreased breath sounds
- Hemorrhage and edema in alveoli
- Hypotension
- Tachycardia
Treatments for Chest Trauma
- Airway management (intubation if necessary)
- Oxygen therapy to maintain adequate oxygenation
- Chest tube insertion for pneumothorax or hemothorax
- Pain management to facilitate breathing and prevent complications
- Surgical repair for severe injuries (e.g., flail chest, major vessel injury)
Medications for Chest Trauma
- Analgesics (e.g., opioids, NSAIDs) for pain control
- Antibiotics if there is an open chest wound or risk of infection
- Sedatives or muscle relaxants if mechanical ventilation is required
Nursing Interventions for Chest Trauma
- Monitor respiratory status (rate, depth, breath sounds).
- Assess for signs of pneumothorax or hemothorax.
- Maintain chest tube drainage system (if present).
- Position the patient to optimize breathing (high Fowler’s position).
- Administer pain medications as prescribed.
- Provide emotional support and reassurance.
Safety and Basic Care for Chest Trauma
- Prevent further injury by stabilizing the patient.
- Educate the patient on deep breathing exercises to prevent pneumonia.
- Monitor for complications such as infection or respiratory failure.
- Ensure proper chest tube management to avoid dislodgement.
Chest Tubes
- Inserted into the pleural space to drain fluid, blood, or air.
- Facilitate lung expansion.
- Reestablish a negative pressure and restore intrapleural pressure.
- Removed when the lungs have re-expanded or there is no more fluid drainage.
Chest Tube Systems
- A disposable three-chamber drainage system is most often used, the first chamber is for drainage collection
- The second chamber is a water seal
- The third chamber is the suction control (can be wet or dry)
Indications for Chest Tubes
- Pneumothorax: Partial/complete lung collapse due to air in pleural space
- Hemothorax: Blood accumulation causing lung collapse
- Postoperative drainage following thoracotomy or open-heart surgery
- Pleural Effusion: Fluid accumulation in pleural space
- Pulmonary Empyema: Pus accumulation due to infection
Client Presentation with Chest Tubes
- Dyspnea
- Distended neck veins
- Hemodynamic instability
- Pleuritic chest pain
- Cough
- Absent or reduced breath sounds on the affected side
- Hyperresonance on percussion of affected side (pneumothorax)
- Dullness or flatness on percussion of the affected side (hemothorax, pleural effusion)
- Asymmetrical chest wall motion
Nursing Interventions for Chest Tubes
- Monitor the water seal chamber for continuous bubbling (air leak finding), locate the source of the air leak and tighten the connection or replace the system
- Check all connections
- Notify the provider if an air leak is noted, gently apply a padded clamp to determine the location of the air leak
- Instruct the client to exhale and cough to remove as much air as possible, if tubing separates
- Immerse the end of the chest tube in sterile water to provide a temporary water seal, if the chest tube drainage system is compromised
- Dress the area with dry, sterile gauze, if the chest tube is accidentally removed
Acute Respiratory Failure (ARF)
- Can result from a ventilation failure, oxygenation failure, or a combination with abnormalities shown on ABG
- Oxygenation failure: PaO2 < 60 mm Hg, with acidosis (low pH) and normal PaCO2.
- Ventilation failure: PaCO2 > 50 mm Hg, with acidosis (low pH) and normal PaO2.
- Combination: PaO2 < 60 mm Hg and PaCO2 > 50 mm Hg, with acidosis (low pH).
Types of Acute Respiratory Failure
- Oxygenation failure (type 1 ARF): O2 has difficulty moving into the blood from the lungs, decreased perfusion, caused by upper/lower obstruction, pneumonia, COVID-19, PE, pulmonary edema, shock, pneumothorax
- Ventilation failure (type 2 ARF): air movement is inadequate while blood movement remains normal, chest pressure doesn’t change enough to allow air in and out of the lungs, caused by myasthenia gravis, tetanus, stroke, meningitis, acities, COPD
- Combined failure: impaired gas exchange and lung perfusion, hypoventilation is always associated, caused by abnormal lungs, bronchitis, emphysema, or cystic fibrosis
Risk Factors for ARF
- Extremely young or advanced age
- Recent exposure to viral or bacterial infections
- Lack of immunizations
- Exposure to environmental contaminants (smoke, pollutants)
- Tobacco smoke
- Substance use (alcohol)
- Chronic lung disease
- Mechanical ventilation (ventilator-acquired pneumonia)
Clinical Manifestations of ARF
- Dyspnea is more intensive as respiratory failure progresses.
- Changes in respiratory rate
- Decreased O2 saturation
- Restlessness, irritability, agitation
- Tachycardia, tachypnea
- Confusion, fatigue
- Cyanosis (late sign)
- ABGs indicate hypoxia and hypercarbia.
Nursing Interventions / Treatment / Medications for ARF
- Nebulized or MDI bronchodilators or anti-inflammatory agents
- Corticosteroids are used if COVID-19 or COPD/Asthma.
- O2 therapy is used if acute hypoxemia; maintain PaO2 levels above 60 mmHg.
Supportive Care for ARF
- Reduce anxiety, position comfortably, conserve energy, encourage deep breathing.
Acute Respiratory Distress Syndrome (ARDS)
- ARDS is ARF with specific features including hypoxemia that persists even when 100% oxygen is given (refractory hypoxemia).
- Decreased pulmonary compliance with dyspnea, non-cardiac-associated bilateral pulmonary edema and dense pulmonary infiltrates on X-ray.
- Not primary diagnosis
Cause of ARDS
- Widespread inflammation leading to damage to alveolar-capillary membranes
Clinical Manifestations of ARDS
- Hyperpnea
- Tachypnea
- Hypoxemia
- Noisy respiration
- Cyanosis
- Pallor
- Retractions
- Hypotension
- Tachycardia
- Dysrhythmias
Diagnostic Assessment for ARDS
- Lowered partial pressure of arterial oxygen (PaO2) with a decreased P/F ratio
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.