Podcast
Questions and Answers
What is a primary cause of Type I respiratory failure?
What is a primary cause of Type I respiratory failure?
- Neuromuscular disease
- Pulmonary disease (correct)
- Obstructive sleep apnea
- Hypercapnia
Which clinical feature is associated with hypoxia?
Which clinical feature is associated with hypoxia?
- Tachycardia
- Restlessness (correct)
- Headache
- Coma
Which management step is essential when treating Type II respiratory failure?
Which management step is essential when treating Type II respiratory failure?
- Continuous positive airway pressure
- Immediate intubation
- Use of simple face mask only
- Controlled oxygen therapy (correct)
What distinguishes a Venturi mask from a simple face mask?
What distinguishes a Venturi mask from a simple face mask?
In cases of longstanding hypoxia, which condition may develop?
In cases of longstanding hypoxia, which condition may develop?
Flashcards are hidden until you start studying
Study Notes
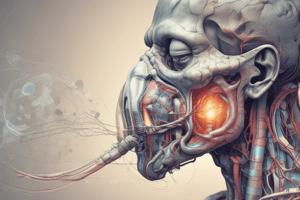
Overview of Respiratory Failure
- Respiratory failure implies inadequate gas exchange, leading to hypoxia.
- Defined as partial pressure of oxygen (PaO2) less than 45 mmHg.
- Caused primarily by alveolar hypoventilation, which may include ventilation/perfusion (V/Q) mismatch.
Causes of Respiratory Failure
- Pulmonary Diseases:
- Severe asthma, chronic obstructive pulmonary disease (COPD), pneumonia, end-stage pulmonary fibrosis, obstructive sleep apnoea.
- Reduced Respiratory Drive:
- Influenced by sedative drugs, central nervous system (CNS) tumors or trauma.
- Neuromuscular Diseases:
- Conditions like cervical cord lesions, diaphragmatic paralysis, poliomyelitis, myasthenia gravis, and Guillain–Barré syndrome.
- Thoracic Wall Disease:
- Flail chest and kyphoscoliosis.
Clinical Features
- Symptoms depend on the underlying cause, with features of hypoxia present.
- Hypoxia Symptoms:
- Dyspnea, restlessness, agitation, confusion, and central cyanosis.
- Long-term hypoxia can lead to complications like polycythaemia, pulmonary hypertension, and cor pulmonale.
- Hypercapnia Symptoms:
- Headache, peripheral vasodilation, tachycardia, bounding pulse, tremor/flap, papilloedema, confusion, drowsiness, and potentially coma.
Investigations
- Blood Tests: Complete blood count (FBC), urea and electrolytes (U&E), C-reactive protein (CRP), arterial blood gas (ABG).
- Radiological Exam: Chest X-ray (CXR).
- Microbiological Testing: Sputum and blood cultures, especially if febrile.
Management Strategies
-
Type I Respiratory Failure:
- Address the underlying cause.
- Administer oxygen via facemask for hypoxia correction.
- Consider assisted ventilation as needed.
-
Type II Respiratory Failure:
- Treat underlying cause and apply controlled oxygen therapy.
- Assisted ventilation may be necessary; if ineffective, intubation and ventilation considerations arise.
Oxygen Delivery Methods
-
Nasal Cannulae:
- Preferred by patients, but less precise delivery may cause nasal discomfort.
-
Simple Face Mask:
- Variable O2 amounts based on inflow rates; risk of CO2 accumulation can occur.
-
Venturi Mask:
- Provides controlled FiO2 (percentage of O2), starting at 24–28% for COPD patients.
-
Non-Rebreathing Mask:
- Equipped with a reservoir bag delivering high O2 concentrations (60–90%).
-
Non-invasive Ventilation:
- Techniques like Continuous Positive Airway Pressure (CPAP) and Bi-level Positive Airway Pressure (BiPAP).
-
Invasive Ventilation:
- Utilized when non-invasive methods fail or in specific severe cases.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.