Podcast
Questions and Answers
What happens to the kidneys' urine production when fluid intake is high?
What happens to the kidneys' urine production when fluid intake is high?
- They produce a large volume of concentrated urine
- They produce a small volume of concentrated urine
- They produce a large volume of dilute urine (correct)
- They stop producing urine
What is the purpose of the osmotic gradient in the medullary interstitial space?
What is the purpose of the osmotic gradient in the medullary interstitial space?
- To regulate blood pressure
- To control the body's temperature
- To regulate electrolyte balance
- To enable the kidneys to produce urine of various osmolarity (correct)
What type of nephrons are responsible for creating the osmotic gradient in the medullary interstitial space?
What type of nephrons are responsible for creating the osmotic gradient in the medullary interstitial space?
- Peritubular nephrons
- Juxtamedullary nephrons (correct)
- Mesangial nephrons
- Cortical nephrons
What is the range of osmolarity that the kidneys can produce urine in?
What is the range of osmolarity that the kidneys can produce urine in?
What happens to the kidneys' urine production when fluid intake is low or fluid loss is high?
What happens to the kidneys' urine production when fluid intake is low or fluid loss is high?
What is the effect of ADH on the late DCT and collecting ducts?
What is the effect of ADH on the late DCT and collecting ducts?
What is the osmolarity of the interstitial fluid in the pelvic tip of the medulla?
What is the osmolarity of the interstitial fluid in the pelvic tip of the medulla?
Which solutes contribute to the osmotic gradient in the renal medulla?
Which solutes contribute to the osmotic gradient in the renal medulla?
What is the main function of countercurrent multiplication?
What is the main function of countercurrent multiplication?
Why is the proximal tubule not fully permeable to urea?
Why is the proximal tubule not fully permeable to urea?
What is the purpose of urea recycling in the kidneys?
What is the purpose of urea recycling in the kidneys?
What type of symporters are present in the thick ascending limb of the LOH?
What type of symporters are present in the thick ascending limb of the LOH?
What is the direction of fluid flow in countercurrent mechanisms?
What is the direction of fluid flow in countercurrent mechanisms?
What is the name of the process that establishes the osmotic gradient in the renal medulla?
What is the name of the process that establishes the osmotic gradient in the renal medulla?
What is the primary function of the kidney in regulating body fluid osmolarity?
What is the primary function of the kidney in regulating body fluid osmolarity?
What is the estimated value of extracellular fluid osmolarity in relation to plasma sodium concentration?
What is the estimated value of extracellular fluid osmolarity in relation to plasma sodium concentration?
What is the primary mechanism involved in regulating extracellular fluid osmolarity?
What is the primary mechanism involved in regulating extracellular fluid osmolarity?
What is the result of an increase in body fluid osmolarity on ADH release?
What is the result of an increase in body fluid osmolarity on ADH release?
What is the role of the kidneys in regulating extracellular fluid osmolarity?
What is the role of the kidneys in regulating extracellular fluid osmolarity?
What is the result of a decrease in body fluid osmolarity on urine production?
What is the result of a decrease in body fluid osmolarity on urine production?
Which of the following hormones is involved in the regulation of extracellular fluid osmolarity?
Which of the following hormones is involved in the regulation of extracellular fluid osmolarity?
What is the main factor that regulates extracellular fluid osmolarity?
What is the main factor that regulates extracellular fluid osmolarity?
What is the primary function of the high water permeability of the descending limb of LOH?
What is the primary function of the high water permeability of the descending limb of LOH?
What is the effect of ADH on the collecting duct?
What is the effect of ADH on the collecting duct?
What is the osmolarity of the glomerular filtrate?
What is the osmolarity of the glomerular filtrate?
What is the role of Na+-K+-2Cl‒ symporters in the ascending limb of LOH?
What is the role of Na+-K+-2Cl‒ symporters in the ascending limb of LOH?
What is the primary mechanism of urine concentration?
What is the primary mechanism of urine concentration?
What is the effect of the absence of ADH on the collecting duct?
What is the effect of the absence of ADH on the collecting duct?
What is the osmolarity of the fluid entering the DCT?
What is the osmolarity of the fluid entering the DCT?
What is the primary function of the countercurrent exchanger?
What is the primary function of the countercurrent exchanger?
What is the minimum volume of urine that must be excreted daily to remove waste products?
What is the minimum volume of urine that must be excreted daily to remove waste products?
What is the osmolarity of urine in a dehydrated state?
What is the osmolarity of urine in a dehydrated state?
What stimulates the thirst center in the brain?
What stimulates the thirst center in the brain?
Why are ADH and thirst essential for controlling ECF osmolarity?
Why are ADH and thirst essential for controlling ECF osmolarity?
What is the ideal fluid balance in terms of isotonic urine production?
What is the ideal fluid balance in terms of isotonic urine production?
What is the osmolarity of waste products that must be excreted daily?
What is the osmolarity of waste products that must be excreted daily?
What is the effect of increased ECF osmolarity on ADH secretion?
What is the effect of increased ECF osmolarity on ADH secretion?
Why do aldosterone and Angiotensin II have little effect on ECF osmolarity?
Why do aldosterone and Angiotensin II have little effect on ECF osmolarity?
Study Notes
Regulation of Body Fluid Osmolarity
- The kidney plays a major role in regulating body fluid osmolarity.
- Extracellular fluid (ECF) osmolarity is estimated to be 2.1 times the plasma Na+ concentration.
- ECF osmolarity is regulated by the amount of fluid intake and renal excretion of water and Na.
Mechanisms of Regulating ECF Osmolarity
- Two mechanisms are involved: the osmo-receptor-ADH system and the thirst mechanism.
- The osmo-receptor-ADH system regulates ECF osmolarity through the ability of the kidneys to form diluted or concentrated urine.
- The thirst mechanism regulates ECF osmolarity through fluid intake.
Production of Dilute and Concentrated Urine
- Fluid intake is highly variable, but the total volume of body fluid remains stable due to the kidneys' ability to regulate water loss in urine.
- When fluid intake is high, the kidneys produce a large volume of dilute urine.
- When fluid intake is low or fluid loss is high, the kidneys produce a small volume of concentrated urine.
Formation of Dilute Urine
- The glomerular filtrate is isotonic with an osmolarity of about 300 mOsm/L.
- The fluid leaving the proximal convoluted tubule (PCT) is still isotonic, but its osmolarity increases as it moves down the descending limb of the Loop of Henle (LOH).
- The fluid entering the distal convoluted tubule (DCT) is hypotonic.
- In the absence of ADH, collecting ducts are impermeable to water, and urine becomes very diluted (65-70 mOsm/L).
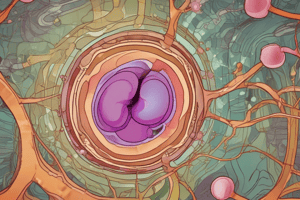
Formation of Concentrated Urine
- Depends on the vertical osmotic gradient established by Na+-K+-2Cl- symporters and urea recycling, and conserving it by the countercurrent exchanger.
- Presence of ADH stimulates aquaporin-2 channels insertion in the apical membrane of the principal cells of the collecting duct, leading to reabsorption of water by osmosis and concentrated urine.
Osmoreceptor-ADH Feedback System
- ADH secretion is more sensitive to increases in ECF osmolarity than reduction in blood volume or blood pressure.
- Stimuli for ADH secretion include:
- Increased osmolarity
- Reduced blood volume (cardiopulmonary receptors)
- Reduced blood pressure (baroreceptors)
Thirst Mechanism
- The thirst center in the brain is stimulated by:
- Increased osmolarity
- Decreased blood volume
- Decreased blood pressure
- Increased Angiotensin II levels
Integrated Responses for Control of ECF Osmolarity
- ADH and thirst mechanism are essential for controlling ECF osmolarity because they absorb water independent of Na+.
- Aldosterone and Angiotensin II have little effect on ECF osmolarity because water follows by osmosis after Na+ reabsorption.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the role of the kidney in regulating body fluid osmolarity, including the production of dilute and concentrated urine. It assesses your understanding of the relationship between extracellular fluid osmolarity and kidney function.