Podcast
Questions and Answers
Explain the physiological significance of low pulmonary vascular resistance (PVR) for gas exchange in the lungs.
Explain the physiological significance of low pulmonary vascular resistance (PVR) for gas exchange in the lungs.
Low PVR allows for a decrease in blood flow velocity, providing more time for gas exchange. Increased capillary distension due to lower pressure also increases surface area for efficient gas exchange.
Describe how the pulmonary circulation adapts to an increase in cardiac output during vigorous exercise.
Describe how the pulmonary circulation adapts to an increase in cardiac output during vigorous exercise.
Despite the increased blood flow and pressure, pulmonary vascular resistance decreases, reducing the right ventricular workload and preventing pulmonary edema.
What is the effect of parasympathetic nervous system stimulation on pulmonary vascular resistance, and why does this occur?
What is the effect of parasympathetic nervous system stimulation on pulmonary vascular resistance, and why does this occur?
Parasympathetic stimulation increases PVR via vasoconstriction, likely due to the release of neurotransmitters like acetylcholine, although this effect is less pronounced than sympathetic effects.
Explain the mechanism of hypoxic vasoconstriction in the pulmonary circulation and its significance.
Explain the mechanism of hypoxic vasoconstriction in the pulmonary circulation and its significance.
How does the response to low oxygen levels in the pulmonary circulation differ from that in systemic circulation?
How does the response to low oxygen levels in the pulmonary circulation differ from that in systemic circulation?
Name two potent vasoconstrictors and two vasodilators that influence pulmonary vascular resistance, and briefly explain their effects.
Name two potent vasoconstrictors and two vasodilators that influence pulmonary vascular resistance, and briefly explain their effects.
How does gravity impact pulmonary vascular pressure, and what are the implications for blood flow distribution in the lungs?
How does gravity impact pulmonary vascular pressure, and what are the implications for blood flow distribution in the lungs?
Why is it important to understand the factors affecting pulmonary blood flow when considering the impact of diseases on the lungs?
Why is it important to understand the factors affecting pulmonary blood flow when considering the impact of diseases on the lungs?
What is the primary function of the bronchial artery?
What is the primary function of the bronchial artery?
What percentage of cardiac output is typically supplied by the bronchial artery?
What percentage of cardiac output is typically supplied by the bronchial artery?
Where does the venous blood from the bronchial circulation primarily drain?
Where does the venous blood from the bronchial circulation primarily drain?
What arteries do the bronchial veins drain into on the right side of the body?
What arteries do the bronchial veins drain into on the right side of the body?
How does the blood from the distal portion of bronchial circulation differ from proximal drainage?
How does the blood from the distal portion of bronchial circulation differ from proximal drainage?
What physiological occurrence results from the mixing of venous and arterial blood in the lungs?
What physiological occurrence results from the mixing of venous and arterial blood in the lungs?
Which structures does the bronchial artery supply besides the bronchi?
Which structures does the bronchial artery supply besides the bronchi?
What type of blood does the bronchial artery carry?
What type of blood does the bronchial artery carry?
What is the relationship between the volume of the pulmonary capillary and the stroke volume of the right ventricle?
What is the relationship between the volume of the pulmonary capillary and the stroke volume of the right ventricle?
How can blood volume in the lungs change in response to systemic hemorrhage?
How can blood volume in the lungs change in response to systemic hemorrhage?
What is the primary function of pulmonary lymphatics?
What is the primary function of pulmonary lymphatics?
Compare the distensibility of pulmonary blood vessels to systemic blood vessels.
Compare the distensibility of pulmonary blood vessels to systemic blood vessels.
What are the mean pressures in the pulmonary artery and systemic artery?
What are the mean pressures in the pulmonary artery and systemic artery?
State the systolic and diastolic pulmonary arterial pressures.
State the systolic and diastolic pulmonary arterial pressures.
What is the mean pressure in the left atrium and major pulmonary veins?
What is the mean pressure in the left atrium and major pulmonary veins?
Explain the significance of the driving pressure in both pulmonary and systemic circulation.
Explain the significance of the driving pressure in both pulmonary and systemic circulation.
What is the primary physiological effect of administering diuretics in cases of pulmonary edema?
What is the primary physiological effect of administering diuretics in cases of pulmonary edema?
How does the composition of fresh water aspirated during drowning lead to different physiological effects compared to saltwater?
How does the composition of fresh water aspirated during drowning lead to different physiological effects compared to saltwater?
What role does pleural fluid play in maintaining lung expansion?
What role does pleural fluid play in maintaining lung expansion?
What is a likely cause of pleural effusion related to cardiac failure?
What is a likely cause of pleural effusion related to cardiac failure?
Describe the connection between hyperkalaemia, hyponatremia, and drowning in fresh water.
Describe the connection between hyperkalaemia, hyponatremia, and drowning in fresh water.
What occurs in Zone 2 of the lungs regarding pulmonary blood flow?
What occurs in Zone 2 of the lungs regarding pulmonary blood flow?
Describe the average ventilation/perfusion (V/Q) ratio at rest.
Describe the average ventilation/perfusion (V/Q) ratio at rest.
What happens to the PO2 and PCO2 in the alveoli if ventilation exceeds perfusion?
What happens to the PO2 and PCO2 in the alveoli if ventilation exceeds perfusion?
How does the supine position affect pulmonary blood flow in the lungs?
How does the supine position affect pulmonary blood flow in the lungs?
What is the significance of the arterial to venous pressure gradient in pulmonary blood flow?
What is the significance of the arterial to venous pressure gradient in pulmonary blood flow?
What occurs in the pulmonary circulation when there is left-sided heart failure?
What occurs in the pulmonary circulation when there is left-sided heart failure?
Why is pulmonary capillary pressure lower than systemic capillary pressure?
Why is pulmonary capillary pressure lower than systemic capillary pressure?
What happens to the perfusion and ventilation in the alveoli if perfusion exceeds ventilation?
What happens to the perfusion and ventilation in the alveoli if perfusion exceeds ventilation?
What role does pulmonary interstitial negative pressure play in keeping the alveoli dry?
What role does pulmonary interstitial negative pressure play in keeping the alveoli dry?
How does increased lymphatic drainage contribute to fluid management in the lungs?
How does increased lymphatic drainage contribute to fluid management in the lungs?
What causes pulmonary edema according to the mechanisms described?
What causes pulmonary edema according to the mechanisms described?
Describe how high interstitial compliance affects fluid dynamics in the lungs.
Describe how high interstitial compliance affects fluid dynamics in the lungs.
What happens to interstitial oncotic pressure when lymph flow drains albumin from pulmonary capillaries?
What happens to interstitial oncotic pressure when lymph flow drains albumin from pulmonary capillaries?
Why can alveolar walls become easily ruptured by positive interstitial pressure?
Why can alveolar walls become easily ruptured by positive interstitial pressure?
What are two physiological consequences of increased alveolar space tension?
What are two physiological consequences of increased alveolar space tension?
How does the leaky nature of pulmonary capillaries affect interstitial oncotic pressure?
How does the leaky nature of pulmonary capillaries affect interstitial oncotic pressure?
Flashcards
Volume of pulmonary capillary
Volume of pulmonary capillary
Approximately equal to the stroke volume of the right ventricle.
Compensation by blood shift
Compensation by blood shift
Blood can shift from lungs to systemic vessels during hemorrhage.
Pulmonary lymphatics
Pulmonary lymphatics
Lymphatic vessels in lung tissues, important for cleaning fluid.
Pulmonary blood pressure
Pulmonary blood pressure
Signup and view all the flashcards
Systolic pulmonary arterial pressure
Systolic pulmonary arterial pressure
Signup and view all the flashcards
Diastolic pulmonary arterial pressure
Diastolic pulmonary arterial pressure
Signup and view all the flashcards
Mean pulmonary arterial pressure
Mean pulmonary arterial pressure
Signup and view all the flashcards
Left atrial and pulmonary venous pressure
Left atrial and pulmonary venous pressure
Signup and view all the flashcards
Bronchial artery
Bronchial artery
Signup and view all the flashcards
Function of bronchial arteries
Function of bronchial arteries
Signup and view all the flashcards
Bronchial veins
Bronchial veins
Signup and view all the flashcards
Physiological shunt
Physiological shunt
Signup and view all the flashcards
Pulmonary veins
Pulmonary veins
Signup and view all the flashcards
Azygos vein
Azygos vein
Signup and view all the flashcards
Left bronchial veins
Left bronchial veins
Signup and view all the flashcards
Contribution to cardiac output
Contribution to cardiac output
Signup and view all the flashcards
Zone 2 of lungs
Zone 2 of lungs
Signup and view all the flashcards
Zone 3 of lungs
Zone 3 of lungs
Signup and view all the flashcards
Ventilation/Perfusion (V/Q) ratio
Ventilation/Perfusion (V/Q) ratio
Signup and view all the flashcards
Effects of gravity on V/Q ratio
Effects of gravity on V/Q ratio
Signup and view all the flashcards
Supine position on blood flow
Supine position on blood flow
Signup and view all the flashcards
Arterial to venous pressure gradient
Arterial to venous pressure gradient
Signup and view all the flashcards
Left atrial pressure rise
Left atrial pressure rise
Signup and view all the flashcards
Pulmonary capillary pressure
Pulmonary capillary pressure
Signup and view all the flashcards
Pulmonary Distension
Pulmonary Distension
Signup and view all the flashcards
Decreased PVR
Decreased PVR
Signup and view all the flashcards
Pulmonary Edema
Pulmonary Edema
Signup and view all the flashcards
Nervous Factors
Nervous Factors
Signup and view all the flashcards
Hypoxia Effect
Hypoxia Effect
Signup and view all the flashcards
Systemic vs Pulmonary Response
Systemic vs Pulmonary Response
Signup and view all the flashcards
Vasoconstrictors
Vasoconstrictors
Signup and view all the flashcards
Gravity and Hydrostatic Pressure
Gravity and Hydrostatic Pressure
Signup and view all the flashcards
Neurogenic shock
Neurogenic shock
Signup and view all the flashcards
Pulmonary oedema treatment
Pulmonary oedema treatment
Signup and view all the flashcards
Freshwater drowning vs. Saltwater drowning
Freshwater drowning vs. Saltwater drowning
Signup and view all the flashcards
Pleural effusion causes
Pleural effusion causes
Signup and view all the flashcards
Negative pleural pressure
Negative pleural pressure
Signup and view all the flashcards
Pulmonary Interstitial Pressure
Pulmonary Interstitial Pressure
Signup and view all the flashcards
Interstitial Oncotic Pressure
Interstitial Oncotic Pressure
Signup and view all the flashcards
Mechanisms keeping alveoli dry
Mechanisms keeping alveoli dry
Signup and view all the flashcards
Role of Lymphatic Drainage
Role of Lymphatic Drainage
Signup and view all the flashcards
Causes of Pulmonary Edema
Causes of Pulmonary Edema
Signup and view all the flashcards
Capillary Hydrostatic Pressure
Capillary Hydrostatic Pressure
Signup and view all the flashcards
Interstitium Compliance
Interstitium Compliance
Signup and view all the flashcards
Study Notes
Pulmonary Circulation and Ventilation and Perfusion
- Pulmonary circulation involves the same blood volume as systemic circulation.
- Pulmonary vascular capacity is lower than systemic, but the pulmonary vascular bed regulates cardiac output to prevent excessive pressure.
- Pulmonary vascular resistance is one-tenth the systemic vascular resistance.
- Total blood volume in lungs is 500mL, which is 10% of overall body blood volume.
Learning Outcomes
- Discuss the physiology of bronchial circulation.
- Understand the significance of the ventilation-perfusion ratio.
- Explain the variations in ventilation-perfusion ratio between lung apex and base.
- Explain the filtration mechanisms in pulmonary capillaries and the genesis of pulmonary edema.
Blood Circulation
- Blood pumped into pulmonary circulation equals blood pumped into systemic circulation.
- Pulmonary vascular bed regulates cardiac output, ensuring less pressure compared to systemic circulation.
- Systemic blood pressure is high due to systemic vessel resistance, while pulmonary pressure is low due to low resistance in pulmonary vessels.
- Pulmonary circulation resistance is one-tenth that of systemic circulation.
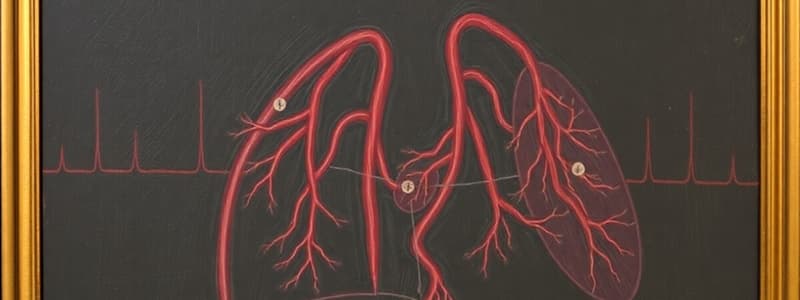
Blood Supply to the Lungs
- Lungs receive blood via pulmonary arteries and bronchial arteries.
- Pulmonary arteries deliver blood to the lungs for gas exchange.
- Bronchial arteries supply blood to lung tissue structures and are a branch off of the descending thoracic aorta.
- Pulmonary blood vessel volume in the lung accounts for ~40% of the total lung weight.
- Blood is distributed segmentally from the pulmonary arteries into the bronchi
Bronchial Artery
- Arise from the descending thoracic aorta.
- Supplies bronchi, connective tissue, and other lung structures.
- Drains into pulmonary veins or drains into the azygos vein (right side) or hemiazygos/superior intercostal veins (left side).
Blood Supply to the Lungs (cont.)
- Deoxygenated blood from the pulmonary artery delivers the required blood flow to all parts of the lung for gas exchange.
- Oxygenated blood is collected and delivered to the left atrium via one pulmonary vein from each lung.
Physiological Shunt
- Diversion where venous blood mixes with arterial blood.
- Has two components:
- Flow of deoxygenated blood from bronchial circulation into pulmonary veins (without oxygenation) - normal part of pulmonary circulation (1-2% of CO).
- Flow of deoxygenated blood from Thebesian veins directly into cardiac chambers.
Physiological Features of Pulmonary Blood Vessels
- Pulmonary artery and large branches are 30% thinner than the aorta wall.
- Small arterial vessels have little muscle in their walls.
- Post-capillary vessels have smooth muscle.
- Pulmonary vascular bed enables compliance to accommodate large stroke volumes.
- Large numbers of capillaries provide ample surface area.
- Each alveolus is surrounded by a capillary network.
Function of Pulmonary Circulation
- Gas exchange: Blood is brought from systemic circulation to contact with alveoli. Oxygenated blood is then collected and returned via pulmonary veins.
- Filtering: Pulmonary vessels filter thrombi and emboli originating from the venous compartment and right side of the heart. Removing clots or emboli from blood helps prevent them from reaching coronary or cerebral vessels.
- Metabolic regulation: Pulmonary vessels metabolize vasoactive hormones via ACE. They control blood vessel tone through inactivation of bradykinin, serotonin, prostaglandins (E1, E2, E2a), and norepinephrine.
- Blood reservoir: The lungs hold about 500 mL of blood, which is approximately equal to the right ventricle stroke volume. This acts as a reservoir, compensating for blood loss elsewhere in the body.
Pulmonary Lymphatics
- Lymphatic vessels are present in supporting structures beginning in tissues around terminal bronchioles.
- Lymphatic vessels drain into the right thoracic duct (hilum of lungs).
- Functions:
- Remove particulate matter from alveoli.
- Remove leaked plasma proteins from lung capillaries. (important for maintaining a healthy interstitial area). This helps prevent edema (fluid buildup in air sacs).
Pulmonary Blood Pressure
- Pulmonary blood vessels are more distensible than systemic vessels.
- Thus, pulmonary blood pressure is lower than systemic pressure.
Pressure in the Pulmonary Circulation
- Pulmonary artery pressure: 15 mmHg
- Systemic artery pressure: 100mmHg
- Other values for pressures at each point in the pulmonary circulation are provided in the text.
- This section presents a comparison of pressures in pulmonary and systemic circulation, including pressures in arteries, capillaries, and veins for both circulations.
Left Atrial and Pulmonary Venous Pressure
- Mean left atrium pressure and major pulmonary veins approximately 2 mmHg (range 1-5 mmHg)
Pressure Differences in Lung Vessels
- Pressure is highest at the pulmonary artery level, then gradually drops to the lowest pressure at the left atrium level as the blood makes its way through the capillaries.
Shift of the Blood Indicates Cardiac Pathology
- Left-sided heart failure or increased mitral valve resistance can lead to increased pulmonary vascular pressure.
Distribution of Blood Flow Through the Lungs
- Pulmonary capillaries, which act as a "sheet" of blood flow efficiently across alveolar surfaces, create less resistance to blood flow.
- Systemic capillaries have a tighter structure and represent a high resistance to blood flow.
Special Feature of Pulmonary Circulation
- Pulmonary circulation has lower pressure (15 mmHg) and low resistance compared to systemic circulation.
- Pulmonary vessels(arteries, veins, and branches) are compliant due to thin walls and less smooth muscle.
- The lungs' large volume capacity allows them to continuously receive all cardiac output and accommodate variations in blood volume associated with posture changes such as standing and lying down).
Factors Affecting Pulmonary Blood Flow
- Cardiac Output: This is directly proportional and regulated by factors such as venous return, force of contraction, rate of contraction, and peripheral vascular resistance.
- Vascular Resistance: Affected by respiratory phases; inspiration (increased flow) and expiration (reduced flow). Exercise leads to lowered vascular resistance and increased flow. Variations in oxygen and carbon dioxide levels also impact vascular resistance.
- Nervous Factors: Parasympathetic stimulation increases vascular resistance, while sympathetic stimulation decreases it.
- Chemical Factors: Hypoxia (low oxygen) causes vasoconstriction in pulmonary vessels, while elevated oxygen levels cause vasodilation. Hormones, including serotonin, norepinephrine, histamine, thromboxane A2, leukotrienes, adenosine, acetylcholine, prostacyclin (PG-12), and isoproterenol, also affect blood flow and resistance.
- Gravity/Hydrostatic Pressure: Blood flow is highest at the base and lowest at the apex of the lungs due to gravity. Alveolar pressure, blood flow, and pressure differentials vary throughout the lungs. This is grouped into 3 zones. The sections provide a visual analogy for understanding
- Arterial to Venous Pressure Gradient: Arterial-venous pressure differences regulate blood flow determined by alveolar pressures throughout the lungs.
Abnormalities of Pulmonary Circulation
- High left atrial pressure (left-sided heart failure) causes small pressure changes affecting pulmonary circulation due to pulmonary venule expansion and opening, allowing for continued blood flow.
- High left atrial pressure exceeding 7-8 mmHg causes pulmonary edema.
Capillary Exchange of Fluid and Pulmonary Interstitial Fluid Dynamics
- Pulmonary capillaries have relatively low pressure compared to systemic capillaries - 7 mmHg vs 17 mmHg.
- Interstitial pressure in the lungs is more negative than peripheral tissues, favoring fluid movement into the capillaries.
- Pulmonary capillaries are more permeable to proteins, increasing interstitial oncotic pressure.
- Alveolar walls are thin and weak, potentially susceptible to rupture with high interstitial pressure. Fluid is subsequently moved to the alveoli, facilitating lung drainage via lymphatic system.
Forces Tending to Cause Fluid Movement
- Capillary pressure, interstitial fluid colloid osmotic pressure, and negative interstitial fluid pressure contribute to fluid movement outward.
- Plasma osmotic pressure and inward interstitial forces (of equal magnitude to outward forces) work toward fluid absorption.
- Net fluid filtration pressure is typically positive, leading to fluid outward from capillaries into the pulmonary interstitial space.
Pulmonary Exchange of Fluid
- Negative interstitial pressure keeps alveoli dry by preventing fluid accumulation in the interstitial spaces.
- Small openings between alveolar epithelial cells allow passage of water and electrolytes, but not large proteins. Pulmonary lymphatics help to prevent fluid buildup in the lungs.
Principle of Lungs Being Kept Dry
- Lymphatic drainage is crucial in maintaining oedema-free pulmonary interstitium.
- High interstitial compliance and lowered oncotic pressure help fluid absorption, which together limit oedema development.
Pulmonary Oedema Causes and Treatment
- Causes include: increased capillary hydrostatic pressure (e.g., left-sided heart failure, mitral valve disease); increased alveolar space tension; decreased oncotic pressure; and increased capillary permeability (e.g., inflammatory reactions, toxic exposures).
- Treatment aims to reduce pulmonary capillary hydrostatic pressure (e.g., diuretics, digitalis).
Drowning
- Fresh water drowning: death from ventricular fibrillation due to aspirated water entering alveoli and causing low hydrostatic pressure and high oncotic pressure in systemic circulation.
- Saltwater drowning: death from asphyxia (inadequate breathing) due to hypertonic water content causing pulmonary edema and aspiration (inhalation) of water.
Negative Pressure in Pleural Fluid
- Negative pleural pressure is maintained by the pumping activity of the lymphatic system (vital for keeping lungs expanded).
- The thin layer of mucoid fluid in the pleura acts as lubrication. Prevents the lungs from sticking to the chest cavity during inhalation).
Pleural Effusion
- Collection of excessive fluid in the pleural space, a condition known as pleural effusion.
- Causes include: lymphatic drainage blockage, high peripheral/pulmonary capillary pressure, low oncotic pressure, or inflammation/breakdown of capillary membranes.
Ventilation/ Perfusion Ratio
- V/Q ratio varies throughout the lungs, with the highest at the base and lowest at the apex, due to gravity and positioning.
- Average V/Q = 0.8 (4.2mL /5.5mL)
- Normal ventilation > perfusion (V/Q >1): higher oxygen in alveoli.
- Normal perfusion > ventilation (V/Q <1 ): higher CO2 in alveoli.
What about the Supine Position?
- Lungs become zone 3 in this position: uniform blood flow throughout the entirety of the lungs, without the influence of gravity.
Arterial to Venous Pressure Gradient
- Pressure difference between arterial and venous blood in different pulmonary zones determines blood flow rate. Alveolar pressure influences this gradient.
Additional Note:
- The factors determining blood flow are complex and interconnected, requiring a detailed comprehension of the underlying mechanisms for a full grasp of the topic.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.