Podcast
Questions and Answers
What does event related packaging assume?
What does event related packaging assume?
- Contents will remain sterile indefinitely unless compromised (correct)
- Contents need constant monitoring for sterility
- Contents will never remain sterile
- Contents will remain sterile for 30 days only
What is a sterilant?
What is a sterilant?
An agent capable of killing all organisms.
What is an autoclave?
What is an autoclave?
Equipment used for sterilizing by means of moist heat under pressure.
What are biologic indicators?
What are biologic indicators?
What is a chemical vapor sterilizer?
What is a chemical vapor sterilizer?
What is a critical instrument?
What is a critical instrument?
What are semi-critical instruments?
What are semi-critical instruments?
What are non-critical instruments?
What are non-critical instruments?
What is the clean area in a sterilization center?
What is the clean area in a sterilization center?
What is the contaminated area?
What is the contaminated area?
How does a dry heat sterilizer work?
How does a dry heat sterilizer work?
What is the use-life of a germicidal solution?
What is the use-life of a germicidal solution?
What does a biologic monitor verify?
What does a biologic monitor verify?
What are multi-parameter indicators?
What are multi-parameter indicators?
What is an endospore?
What is an endospore?
What does an ultrasonic cleaner do?
What does an ultrasonic cleaner do?
What is a single parameter indicator?
What is a single parameter indicator?
What are the methods of pre-cleaning instruments?
What are the methods of pre-cleaning instruments?
What is the least desirable method of pre-cleaning instruments?
What is the least desirable method of pre-cleaning instruments?
How does an ultrasonic cleaner work?
How does an ultrasonic cleaner work?
Kitchen dishwashers are FDA approved for pre-cleaning instruments.
Kitchen dishwashers are FDA approved for pre-cleaning instruments.
What is the purpose of lubricants in instrument processing?
What is the purpose of lubricants in instrument processing?
What should be ensured before wrapping instruments for sterilization?
What should be ensured before wrapping instruments for sterilization?
What is biological monitoring?
What is biological monitoring?
What causes sterilization failures?
What causes sterilization failures?
What are common forms of heat sterilization?
What are common forms of heat sterilization?
What is the primary disadvantage of flash sterilization?
What is the primary disadvantage of flash sterilization?
What is a major advantage of chemical vapor sterilization?
What is a major advantage of chemical vapor sterilization?
What is static air?
What is static air?
What type of water is used to rinse instruments processed in a liquid chemical sterilant?
What type of water is used to rinse instruments processed in a liquid chemical sterilant?
What should be done to prepare a high-speed handpiece for sterilization?
What should be done to prepare a high-speed handpiece for sterilization?
What type of heat sterilization is appropriate for high-speed handpieces?
What type of heat sterilization is appropriate for high-speed handpieces?
What are examples of semi-critical instruments?
What are examples of semi-critical instruments?
How can a dental assistant be exposed to microorganisms?
How can a dental assistant be exposed to microorganisms?
What is cavitation?
What is cavitation?
How does an ultrasonic cleaner work?
How does an ultrasonic cleaner work?
What is the result of inadequate instrument cleaning?
What is the result of inadequate instrument cleaning?
What are examples of improper packaging for sterilization?
What are examples of improper packaging for sterilization?
What happens if there is excessive wrapping of instruments?
What happens if there is excessive wrapping of instruments?
What can result from using closed containers in vapor or autoclave?
What can result from using closed containers in vapor or autoclave?
What is the result of overloading a sterilizer?
What is the result of overloading a sterilizer?
What can happen if there is a lack of separation between packages in the sterilizer?
What can happen if there is a lack of separation between packages in the sterilizer?
What can result from improper timing of sterilization?
What can result from improper timing of sterilization?
What do examples of improper sterilization technique include?
What do examples of improper sterilization technique include?
Flashcards are hidden until you start studying
Study Notes
Instrument Processing and Sterilization
- Event Related Packaging: Sterility of package contents is maintained indefinitely unless the package is compromised.
- Sterilant: An agent that kills all microorganisms, ensuring complete sterilization.
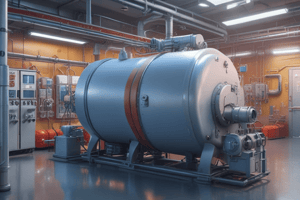
- Autoclave: A sterilization device that uses moist heat and pressure to eliminate organisms.
- Biologic Indicators: Also known as spore tests, these contain harmless spores to verify the effectiveness of sterilizers.
- Chemical Vapor Sterilizer: Utilizes hot formaldehyde vapors under pressure for sterilization purposes.
- Critical Instruments: Tools that penetrate soft tissue or bone; they must always be heat sterilized.
- Semi-Critical Instruments: Tools that contact oral tissues without penetrating; they should be heat sterilized.
- Non-Critical Instruments: Items that only touch intact skin; sterilization requirements are less stringent.
- Clean Area: A designated space for storing sterilized instruments and supplies.
- Contaminated Area: The section of the sterilization center dedicated to precleaning contaminated instruments.
- Dry Heat Sterilizer: A sterilization method that uses heated air to achieve sanitation.
- Use-Life: The effective time span for a prepared germicidal solution.
- Biologic Monitor: Confirms sterilization by ensuring all spore-forming organisms are eliminated.
- Multi-Parameter Indicators: Items like tapes or strips that change color based on exposure to specific conditions.
- Endospore: A resilient, dormant structure in some bacteria that withstands harsh environments.
- Ultrasonic Cleaner: A device using sound waves in liquids to dislodge debris from instruments.
- Single Parameter Indicator: Devices that respond to specific sterilization conditions such as time or temperature.
- Instrument Classification: Based on sterilization needs: Critical, Semi-Critical, Non-Critical.
- Goggle Type Eyewear: Essential personal protective equipment (PPE) during instrument processing.
- Single-Loop Workflow: Recommended workflow pattern to ensure efficiency in the processing area.
- Holding Solution: Where instruments unable to be processed immediately are placed.
- Precleaning Methods: Include hand scrubbing, ultrasonic cleaning, and thermal washer disinfector.
- Hand Scrubbing: Considered the least effective method for precleaning instruments.
- Kitchen Dishwashers: Not FDA approved for instrument precleaning due to inadequate sanitization capabilities.
- Lubricants: Used on instruments to prevent rust and maintain functionality.
- Packaging for Sterilization: Essential for maintaining sterility after sterilization processes.
- Forms of Sterilization Monitoring: Involves physical, chemical, and biological methods for verifying sterility.
- Spore Testing: A method of biological monitoring to confirm effective sterilization.
- Common Heat Sterilization Methods: Include steam, chemical vapor, and dry heat.
- Flash Sterilization Disadvantage: Lacks the ability to wrap items for protection and sterility maintenance.
- Chemical Vapor Major Advantage: Prevents rusting of instruments during the sterilization process.
- Static Air Example: Type of dry heat sterilization process.
- Sterile Water: Used for rinsing instruments treated with liquid chemical sterilants.
- High-Speed Handpiece Preparation: Requires flushing water through before sterilization.
- Appropriate Heat Sterilization for Handpieces: Steam, chemical vapor, and liquid chemical sterilants are suitable.
- Examples of Semi-Critical Instruments: Include plastic-handled brushes, HVE tips, rubber dam forceps, and amalgam carriers.
- Microorganism Exposure for Dental Assistants: Can occur through contact with contaminated instruments via percutaneous or permucosal means.
- Cavitation: The formation of bubbles in a liquid, a principle used in ultrasonic cleaning.
- Ultrasonic Cleaner Function: Uses inaudible sound waves to create cavitation for debris removal.
- Ultrasonic Cleaner Solution: Highly contaminated and needs to be replaced daily or when visibly cloudy.
- Chemical Vapor Sterilization Benefits: Prevents rust, dulling, and corrosion of metal instruments.
- Endospores Characteristics: They exhibit resistance and dormancy enabling survival under harsh conditions.
- Recommended Sterilizing Techniques: Steam and chemical vapor sterilization are preferred for longevity and effectivity.
- Instrument Preparation for Sterilization: Must ensure cleanliness and dryness to avoid rusting.
- Importance of Cleaning Before Wrapping: Avoiding rust is crucial—clean and dry instruments ensure effective sterilization.
- Consequences of Inadequate Cleaning: Residual organisms may shield themselves from sterilizing agents.
- Improper Packaging Examples: May include excessive wrapping or using incompatible materials.
- Excessive Wrapping Impact: Blocks sterilizing agents from contacting instruments effectively.
- Wrong Packaging Materials: Can lead to melting or hinder penetration of sterilizing agents.
- Closed Containers Use: In vapor or autoclave processes, they prevent sterilizing agents from reaching interior surfaces.
- Improper Sterilizer Loading Examples: Issues include overloading and failure to separate packaging adequately.
- Overloading Results: Can delay reaching proper temperatures and hinder sterilizing agent penetration.
- Lack of Separation Consequences: Hinders effective sterilization as agents may not contact all items.
- Improper Timing Examples: Can involve starting timers incorrectly or premature door openings.
- Consequences of Improper Timing: Insufficient time during sterilization can prevent effectiveness.
- Improper Sterilization Techniques: Errors in method operation can result in malfunction and ineffective sterilization.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.