Podcast
Questions and Answers
Which of the following treatments is NOT recommended for chronic musculoskeletal pain?
Which of the following treatments is NOT recommended for chronic musculoskeletal pain?
- Massage therapy
- Opioids (correct)
- Trigger point injections
- NSAIDs
What is a characteristic feature of osteoarthritis pathology?
What is a characteristic feature of osteoarthritis pathology?
- Bone collapse and wear (correct)
- Excessive cartilage production
- Chronic inflammation of synovial fluid
- Increased joint lubrication
Which diagnostic criteria is NOT used for osteoarthritis?
Which diagnostic criteria is NOT used for osteoarthritis?
- Age greater than 45
- Morning stiffness
- Persistent joint pain in multiple joints
- Evidence of inflammation in synovial fluid (correct)
What is commonly observed in the synovial fluid of a patient with osteoarthritis?
What is commonly observed in the synovial fluid of a patient with osteoarthritis?
Which of the following factors can contribute to the progression of osteoarthritis?
Which of the following factors can contribute to the progression of osteoarthritis?
What is one key element that should be included during the disclosure of complications to patients and their families?
What is one key element that should be included during the disclosure of complications to patients and their families?
Which of the following should be included when disclosing complications to families?
Which of the following should be included when disclosing complications to families?
What is a potential consequence of delivering life-altering news without empathic communication skills?
What is a potential consequence of delivering life-altering news without empathic communication skills?
When should error disclosure ideally take place after an incident?
When should error disclosure ideally take place after an incident?
Which setting is recommended for disclosing complications to minimize interruptions?
Which setting is recommended for disclosing complications to minimize interruptions?
What is the significance of the phrase 'bad news' in patient-doctor communications?
What is the significance of the phrase 'bad news' in patient-doctor communications?
What is an essential moment in empathic communication?
What is an essential moment in empathic communication?
What is recommended regarding the attendees present during the disclosure of an error?
What is recommended regarding the attendees present during the disclosure of an error?
Which muscles are primarily affected in Erb-Duchenne palsy?
Which muscles are primarily affected in Erb-Duchenne palsy?
What characteristic posture of the arm is associated with Erb-Duchenne palsy?
What characteristic posture of the arm is associated with Erb-Duchenne palsy?
Which muscle group is functional in cases of Erb-Duchenne palsy?
Which muscle group is functional in cases of Erb-Duchenne palsy?
What is a common clinical finding associated with Klumpke paralysis?
What is a common clinical finding associated with Klumpke paralysis?
What signifies a poor prognosis in infants with birth-related brachial plexus injuries?
What signifies a poor prognosis in infants with birth-related brachial plexus injuries?
What is the most reliable indicator for considering surgical intervention in cases of brachial plexus injury?
What is the most reliable indicator for considering surgical intervention in cases of brachial plexus injury?
When is spontaneous recovery most likely to occur in infants with upper root paralysis?
When is spontaneous recovery most likely to occur in infants with upper root paralysis?
Which imaging technique is considered promising but not yet routine for evaluating brachial plexus injuries?
Which imaging technique is considered promising but not yet routine for evaluating brachial plexus injuries?
What is a key indication for early surgical intervention in brachial plexus injury?
What is a key indication for early surgical intervention in brachial plexus injury?
How effective is clinical assessment compared to electrical testing for determining outcomes in brachial plexus injuries?
How effective is clinical assessment compared to electrical testing for determining outcomes in brachial plexus injuries?
What is the primary mechanism of action of methotrexate in the treatment of rheumatoid arthritis?
What is the primary mechanism of action of methotrexate in the treatment of rheumatoid arthritis?
Which of the following adverse effects is associated with hydroxychloroquine?
Which of the following adverse effects is associated with hydroxychloroquine?
In the treatment of systemic lupus erythematosus, which medication is used as a combination therapy for active proliferative lupus nephritis?
In the treatment of systemic lupus erythematosus, which medication is used as a combination therapy for active proliferative lupus nephritis?
What is a primary goal in the management of rheumatoid arthritis?
What is a primary goal in the management of rheumatoid arthritis?
Which characteristic is a distinguishing feature of synovial sarcoma?
Which characteristic is a distinguishing feature of synovial sarcoma?
What complication is associated with the long-term use of biologic DMARDs like TNF inhibitors?
What complication is associated with the long-term use of biologic DMARDs like TNF inhibitors?
In the context of pediatric musculoskeletal oncology, which disease is associated with the EWS-FLI 1 mutation?
In the context of pediatric musculoskeletal oncology, which disease is associated with the EWS-FLI 1 mutation?
What is the expected clinical presentation for Erb-Duchenne palsy?
What is the expected clinical presentation for Erb-Duchenne palsy?
Which of the following conditions significantly increases the risk of developing osteosarcoma?
Which of the following conditions significantly increases the risk of developing osteosarcoma?
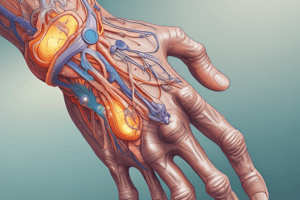
In the layered approach to anatomy, which structure is involved in dynamic stability?
In the layered approach to anatomy, which structure is involved in dynamic stability?
What is one of the primary risk factors for developing synovial sarcoma?
What is one of the primary risk factors for developing synovial sarcoma?
Which approach is crucial in the management of pelvic pain by a PM&R physician?
Which approach is crucial in the management of pelvic pain by a PM&R physician?
Which of the following components makes up the caudal part of the brachial plexus?
Which of the following components makes up the caudal part of the brachial plexus?
What is a well-known side effect of leflunomide, an immunosuppressive agent?
What is a well-known side effect of leflunomide, an immunosuppressive agent?
What does the 'N' in the NURSE mnemonic stand for?
What does the 'N' in the NURSE mnemonic stand for?
Which of the following is a key characteristic of fibromyalgia?
Which of the following is a key characteristic of fibromyalgia?
What is a clinical feature of myofascial pain syndrome (MPS)?
What is a clinical feature of myofascial pain syndrome (MPS)?
Which aspect is NOT part of the SPIKES protocol for delivering bad news?
Which aspect is NOT part of the SPIKES protocol for delivering bad news?
What should be prioritized in the non-pharmacological management of fibromyalgia?
What should be prioritized in the non-pharmacological management of fibromyalgia?
Which of the following correctly describes the treatment approach for fibromyalgia?
Which of the following correctly describes the treatment approach for fibromyalgia?
Which of the following is a symptom of both fibromyalgia and myofascial pain syndrome?
Which of the following is a symptom of both fibromyalgia and myofascial pain syndrome?
What is the primary focus of the 'E' in the SPIKES protocol?
What is the primary focus of the 'E' in the SPIKES protocol?
Patients with fibromyalgia often report high levels of what coexisting conditions?
Patients with fibromyalgia often report high levels of what coexisting conditions?
Which of the following statements accurately describes a treatment consideration for myofascial pain syndrome?
Which of the following statements accurately describes a treatment consideration for myofascial pain syndrome?
Which symptom differentiates fibromyalgia from myofascial pain syndrome?
Which symptom differentiates fibromyalgia from myofascial pain syndrome?
What is meant by 'central sensitization' in fibromyalgia?
What is meant by 'central sensitization' in fibromyalgia?
In the context of treatment for fibromyalgia, what is the role of cognitive-behavioral therapy (CBT)?
In the context of treatment for fibromyalgia, what is the role of cognitive-behavioral therapy (CBT)?
What aspect of NURSE emphasizes the necessity of good listening techniques?
What aspect of NURSE emphasizes the necessity of good listening techniques?
Flashcards
Osteoarthritis
Osteoarthritis
Chronic degenerative joint failure characterized by cartilage loss, bone changes, pain, and dysfunction.
Usage-related joint pain
Usage-related joint pain
Pain and stiffness in a joint that worsens with activity and improves with rest.
Cartilage loss in osteoarthritis
Cartilage loss in osteoarthritis
Loss of cartilage in a joint, leading to bone-on-bone contact and pain.
Synovial inflammation in osteoarthritis
Synovial inflammation in osteoarthritis
Signup and view all the flashcards
Bony sclerotic changes
Bony sclerotic changes
Signup and view all the flashcards
Bad news in medical communication
Bad news in medical communication
Signup and view all the flashcards
Importance of a respectful setting and tone
Importance of a respectful setting and tone
Signup and view all the flashcards
Empathic communication: Anticipating and imagining
Empathic communication: Anticipating and imagining
Signup and view all the flashcards
Empathic communication: Acknowledging and validating emotions
Empathic communication: Acknowledging and validating emotions
Signup and view all the flashcards
Empathic communication: Active Listening
Empathic communication: Active Listening
Signup and view all the flashcards
Error Disclosure: Error Statement
Error Disclosure: Error Statement
Signup and view all the flashcards
Error Disclosure: Error Details
Error Disclosure: Error Details
Signup and view all the flashcards
Error Disclosure: Apology and Prevention
Error Disclosure: Apology and Prevention
Signup and view all the flashcards
Erb-Duchenne Palsy
Erb-Duchenne Palsy
Signup and view all the flashcards
Klumpke's Paralysis
Klumpke's Paralysis
Signup and view all the flashcards
Spontaneous Recovery
Spontaneous Recovery
Signup and view all the flashcards
Biceps Contraction
Biceps Contraction
Signup and view all the flashcards
Lack of Biceps Contraction (by 3 months)
Lack of Biceps Contraction (by 3 months)
Signup and view all the flashcards
Complete Palsy with Flail Arm
Complete Palsy with Flail Arm
Signup and view all the flashcards
C5, C6, and C7 Palsy
C5, C6, and C7 Palsy
Signup and view all the flashcards
Electromyography (EMG)
Electromyography (EMG)
Signup and view all the flashcards
Myelography
Myelography
Signup and view all the flashcards
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI)
Signup and view all the flashcards
Fibromyalgia (FM)
Fibromyalgia (FM)
Signup and view all the flashcards
Myofascial Pain Syndrome (MPS)
Myofascial Pain Syndrome (MPS)
Signup and view all the flashcards
Central Sensitization
Central Sensitization
Signup and view all the flashcards
Tender Points
Tender Points
Signup and view all the flashcards
Widespread Pain Index (WPI)
Widespread Pain Index (WPI)
Signup and view all the flashcards
Symptom Severity (SS) Score
Symptom Severity (SS) Score
Signup and view all the flashcards
Sympathetic Overdrive
Sympathetic Overdrive
Signup and view all the flashcards
Trigger Points
Trigger Points
Signup and view all the flashcards
Pain Avoidance
Pain Avoidance
Signup and view all the flashcards
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT)
Signup and view all the flashcards
Nociception
Nociception
Signup and view all the flashcards
Pregabalin (Lyrica)
Pregabalin (Lyrica)
Signup and view all the flashcards
Duloxetine (Cymbalta)
Duloxetine (Cymbalta)
Signup and view all the flashcards
Milnacipran (Savella)
Milnacipran (Savella)
Signup and view all the flashcards
SPIKES
SPIKES
Signup and view all the flashcards
DMARDs
DMARDs
Signup and view all the flashcards
Methotrexate (MTX)
Methotrexate (MTX)
Signup and view all the flashcards
Hydroxychloroquine (HCQ)
Hydroxychloroquine (HCQ)
Signup and view all the flashcards
Leflunomide
Leflunomide
Signup and view all the flashcards
Sulfasalazine
Sulfasalazine
Signup and view all the flashcards
JAK Inhibitors
JAK Inhibitors
Signup and view all the flashcards
TNF Inhibitors
TNF Inhibitors
Signup and view all the flashcards
Rituximab
Rituximab
Signup and view all the flashcards
T cell Co-stimulation Inhibitors
T cell Co-stimulation Inhibitors
Signup and view all the flashcards
IL-6 Receptor Blockers
IL-6 Receptor Blockers
Signup and view all the flashcards
Goals of SLE Treatment
Goals of SLE Treatment
Signup and view all the flashcards
Treatment Strategies for SLE
Treatment Strategies for SLE
Signup and view all the flashcards
Rhabdomyosarcoma
Rhabdomyosarcoma
Signup and view all the flashcards
Synovial Sarcoma
Synovial Sarcoma
Signup and view all the flashcards
Genetic Predispositions for Sarcoma
Genetic Predispositions for Sarcoma
Signup and view all the flashcards
Study Notes
Pharmacology of Rheumatoid Arthritis & Systemic Lupus Erythematosus
-
Rheumatoid Arthritis (RA) Treatment Goals: Control disease activity, slow joint damage, minimize pain/stiffness/complications.
-
RA Treatment General Guidelines:
- High Disease Activity: Start with methotrexate, avoid steroids.
- Low Disease Activity: Hydroxychloroquine (HCQ), Sulfasalazine (SSZ), Methotrexate (MTX). Vaccinate before treatment.
- Symptomatic Control: Use NSAIDs or corticosteroids for flares, adjunct to DMARD therapy.
-
Disease-Modifying Anti-Rheumatic Drugs (DMARDs):
- Non-Biologic DMARDs:
- Methotrexate: First-line, folic acid antagonist, blocks purine synthesis, weekly dosing. Adverse effects: stomatitis, nausea/diarrhea, alopecia, myelosuppression, hepatic/pulmonary fibrosis. Contraindications: liver/lung disease, alcohol abuse, pregnancy.
- Hydroxychloroquine: Increases pH, inhibits immune cells, hepatic/renal excretion. Adverse effects: cardiomyopathy, ocular changes (retinal depigmentation, retinopathy, corneal deposits). Contraindications: long-term use in children.
- Leflunomide: Inhibits pyrimidine synthesis (prodrug). Adverse effects: nausea, weight loss, alopecia, hepatotoxicity, thrombocytopenia. Contraindications: pregnancy.
- Sulfasalazine: Mechanism uncertain, may be leukotriene/TNF inhibitor. Adverse effects: nausea, dyspepsia, headache, rash, fatal blood dyscrasias.
- JAK Inhibitors (Tofacitinib, Baricitinib, Upadacitinib): Block immune signaling. Used as monotherapy or with other non-biologic DMARDs. Adverse effects: infection, hypertension, anemia, hepatic injury, latent TB reactivation.
- Biologic DMARDs:
- TNF Inhibitors: Used after DMARD failure. Adverse effects: headache, infection, rash, injection site reactions, allergic reactions, demyelinating disorders, heart failure, leukemias. Contraindications: demyelinating disorders, heart failure, recent malignancy, latent TB, avoid live vaccines.
- Anti-B Cell (Rituximab): Used if TNF inhibitors fail. Adverse effects: infection, rare fatal reactions, GI perforation, interstitial pneumonitis.
- T-Cell Co-Stimulation Inhibitors: Blocks T-cell activation. Adverse effects: headache, nausea, infection, hypertension, leukemia, malignancies. Contraindications: immunocompromised patients.
- IL-6 Receptor Blockers: Reduces cytokine reactions. Adverse effects: headache, diarrhea, increased liver function tests (LFTs), LDL elevation. Contraindications: hypersensitivity, demyelinating polyneuropathies, infection, TB reactivation.
- Non-Biologic DMARDs:
-
Systemic Lupus Erythematosus (SLE) Treatment Goals: Remission with minimal adverse effects, prevention of comorbidities (e.g., osteoporosis).
-
SLE Treatment General Guidelines:
- Mild Disease: NSAIDs, low-potency immunosuppressants, HCQ.
- Organ Involvement: Prolonged steroids, potent immunosuppression (cyclosporine, mycophenolate, azathioprine). High-dose glucocorticoids + cytotoxic agents (combo therapy).
- Drug-Induced Lupus: Treat with NSAIDs, glucocorticoids (adjust dose based on affected areas).
-
SLE Risk Factors: Radiation, chemotherapy, genetics (retinoblastoma, Li-Fraumeni syndrome), Paget's disease.
Pediatric Musculoskeletal Oncology
- Key Cancers: Ewing sarcoma, Langerhans cell histiocytosis, rhabdomyosarcoma, synovial sarcoma.
- Ewing Sarcoma: Second most common childhood bone cancer. Small round blue cell tumors, arise from neural crest, commonly in diaphysis. Associated with EWS-FLI 1 mutation. Radiographic features: mixed radiolucent/radiodense, permeative destructive pattern, "onion skinning."
- Langerhans Cell Histiocytosis: Proliferation of Langerhans cells. CD1a and S100 positive, Birbeck granules on electron microscopy. Lesions in skin, lymph nodes, spleen, marrow, lungs, brain.
- Rhabdomyosarcoma: Most common soft tissue sarcoma. Originates from skeletal muscle, often in head/neck/GU. Risk factors: Li-Fraumeni syndrome, radiation. Histology: sheets of small round blue cells. Subtypes: embryonal (MYOD1, desmin, actin positive) and alveolar (PAX3/FKHR or PAX7/FKHR fusion gene).
- Synovial Sarcoma: Spindle cell carcinoma of soft tissue, in deep extremities (knees, shoulder), slow-growing. Epithelial markers (keratins, EMA, S100) positive. Associated with SYT/SSX fusion gene.
- Risk Factors for Pediatric Musculoskeletal Sarcomas: Li-Fraumeni syndrome (p53 mutation), neurofibromatosis 1 (NF1), hereditary retinoblastoma, radiation exposure.
Physiatric Approach to Non-Rheumatologic MSK Care
- MSK Anatomy: Layered approach includes osteochondral, joint congruence (static stability), arthrokinematic movement, contractile (dynamic stability), neuromechanical (mechanical rhythm, neurovascular structures).
- MSK History: Onset, provocation/palliation, quality, radiation, severity, time. Duration, disability, desire, patient goals, training changes.
- MSK Physical Exam: Visual: skin, symmetry, posture. Palpation: pain reproduction, masses, step-offs. Range of motion (ROM): active, passive. Neuro: strength, sensation, reflexes, long track signs. Functional tests (squat, step-down, gait). Special tests (provocative).
- Treatment Options: Activity modification (posture, sleep), home exercises, medications (analgesics, NSAIDs, neuropathic), orthotics, surgical interventions.
- Athlete Care: Identify operative candidates (neurologic/vascular compromise, structural damage, minimal non-surgical improvement, intractable pain, malignancy/infection).
Management of the Patient with Pelvic Pain
- PM&R Physician Role: Focus on physical impairments, restore/enhance function, maximize quality of life, support patients/families, coordinate interdisciplinary care, improve access to rehab.
- PM&R Physician Background/Training: 1 year internship, 3 year residency. Subspecialties exist in brain injury, sport medicine, pediatric rehabilitation, spinal cord injury, hospice/palliative care, neuromuscular medicine, pain medicine, pelvic health.
- Physical Therapist Role: Movement expert, improve quality of life through hands-on care, education, prescribed movement/exercise. Doctor of Physical Therapy degree, state licensure, additional fellowships/residencies.
- MSK Assessment: Global screen (UE/LE joint motion, scapular motion, function squat, heel/toe walk), spinal movement screen, single-leg stance, strength tests, peripheral nerve screen, special tests, movement screens (lunge, squat, step-up, stairs), sport/work-specific screens, balance.
- Collaboration: PM&R physician and PT utilize each other's expertise, referrals are common, early PT involvement improves outcomes.
Synthesis
- Brachial Plexus: Formed by anterior rami of C5-T1, innervating the upper limb and shoulder.
- Erb-Duchenne Palsy: Upper brachial plexus injury (C5, C6). Arm adducted, medially rotated, and elbow extended.
- Klumpke Paralysis: Lower brachial plexus injury (C8, T1). Claw hand, forearm supinated, wrist extended, fingers flexed.
- Brachial Plexus Injury Prognosis: Spontaneous recovery possible in early stages (first 3 months). Complete recovery is more likely with early biceps contraction and normal contraction by month 2. EMG and myelography are imprecise monitoring tools. Surgery is indicated for non-recovering infants, especially those with complete palsy after birth. Early intervention is key for better outcomes.
- Ethical Disclosure: Clear, objective explanation of error/complication, sincere apology, avoidance of future incidents, minimized interruptions, family support, and presence of involved personnel.
Breaking Bad News
- Bad News Definition: Serious, life-altering news impacting patient and loved-ones.
- Respectful Setting/Tone: Focus on delivering news empathetically, not methodically. Establish trust for better outcomes.
- Communication Skills: Anticipate and imagine patient/family experiences; notice and recognize emotions (body language, paralanguage, emotional statements); acknowledge and respond effectively (empathic responses).
- SPIKES Model: S - Setting, P - Perception, I - Invitation, K - Knowledge, E - Emotion.
- NURSE Model: N - Name emotions, U - Understanding, R - Respect, S - Support, E - Explore Emotions.
Fibromyalgia & Myofascial Pain
- Fibromyalgia (FM) Pathophysiology: Widespread musculoskeletal pain/tenderness, genetic predisposition, central sensitization (reduced descending pain inhibition), potential peripheral pathology (reduced nerve fibers, AV shunt changes).
- Myofascial Pain Syndrome (MPS) Pathophysiology: Regional soft tissue pain, acute/repetitive microtrauma or chronic strain, calcium release -> sustained muscle contraction, ischemia/inflammation/nociceptor sensitization, increased pro-nociceptive mediators and sympathetic activity.
- Fibromyalgia Clinical Features: Widespread pain (3+months), diffuse/bilateral, tenderness/increased sensitivity (tender points), sleep disturbance/fatigue, anxiety/depression, cognitive complaints.
- Myofascial Pain Clinical Features: Localized/regional deep pain, one/two muscles, trigger points, less systemic symptoms.
- Fibromyalgia Diagnostic Workup: Symptoms 3+ months, rule out other disorders, WPI ≥ 7 & SS ≥ 5 (or WPI 3-6 & SS ≥ 9).
- Myofascial Pain Diagnostic Workup: Suspect based on regional pattern, trigger points, persistent pain.
- Fibromyalgia Treatment: Education, pain-independent behaviors, CBT, aerobic exercise, sleep hygiene. Medications (pregabalin, duloxetine, milnacipran).
- Myofascial Pain Treatment: PT (stretching, strengthening, trigger point release), heat/cold therapy, massage, trigger point injections, NSAIDs, muscle relaxants, SNRIs, TENS.
Osteoarthritis
- Osteoarthritis Pathophysiology: Chronic degenerative joint failure; loss/failure of joint protection, cartilage loss, bony sclerosis, weakness, pain, mild-moderate inflammation, dysfunction; post trauma OA, genetics, obesity (increases incidence/progression). Loss of joint protection, accelerated wear, loss of lubricant, stress/synovial inflammation (more catabolic factors than anabolic), bone collapse, joint capsule/ligament injury, muscle weakness, peripheral neuropathy.
- Osteoarthritis Diagnostic Workup: May be diagnosed without investigations, but imaging may be useful to guide treatment; synovial fluid analysis (non-inflammatory, mostly mononuclear cells), ESR/CRP typically normal, tests for rheumatoid arthritis (RA). Persistent usage-related joint pain (one or few joints), age > 45, morning stiffness.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.