Podcast
Questions and Answers
What characterizes nociceptive pain?
What characterizes nociceptive pain?
- Results from chemical, thermal, or mechanical sources (correct)
- Is restricted to deep tissue only
- Occurs without identifiable tissue damage
- Presents as burning or numbness
Which statement accurately describes acute pain?
Which statement accurately describes acute pain?
- Is primarily felt as a burning sensation
- Displays signs such as hypertension and tachycardia (correct)
- Has no obvious relationship with stimuli
- Lasts for more than three months
What type of pain is often difficult to localize and can be described as cramping and deep squeezing?
What type of pain is often difficult to localize and can be described as cramping and deep squeezing?
- Visceral pain (correct)
- Somatic pain
- Neuropathic pain
- Similar to allodynia
Which of the following symptoms is common in chronic pain conditions?
Which of the following symptoms is common in chronic pain conditions?
Which defines neuropathic pain?
Which defines neuropathic pain?
What is the mechanism of action of baclofen?
What is the mechanism of action of baclofen?
What are common adverse effects of cyclobenzaprine?
What are common adverse effects of cyclobenzaprine?
How should capsaicin be applied for effective relief?
How should capsaicin be applied for effective relief?
Which is a potential adverse effect of tizanidine?
Which is a potential adverse effect of tizanidine?
What is the formulation of topical lidocaine available for local anesthesia?
What is the formulation of topical lidocaine available for local anesthesia?
Which local anesthetic is commonly used for regional anesthesia?
Which local anesthetic is commonly used for regional anesthesia?
What is a common adverse effect observed with corticosteroids?
What is a common adverse effect observed with corticosteroids?
What can happen with long-term use of opioid analgesics?
What can happen with long-term use of opioid analgesics?
How should topical NSAIDs be treated for mild to moderate localized pain?
How should topical NSAIDs be treated for mild to moderate localized pain?
Which medication class is used as a non-competitive NMDA receptor antagonist?
Which medication class is used as a non-competitive NMDA receptor antagonist?
Which assessment tool is appropriate for ongoing pain assessment?
Which assessment tool is appropriate for ongoing pain assessment?
What is the primary goal of therapy for chronic pain?
What is the primary goal of therapy for chronic pain?
Which statement accurately reflects a principle of pain management for mild pain (1-3)?
Which statement accurately reflects a principle of pain management for mild pain (1-3)?
What is a key characteristic of NSAIDs compared to acetaminophen?
What is a key characteristic of NSAIDs compared to acetaminophen?
What is the mechanism of action for anticonvulsants like gabapentin?
What is the mechanism of action for anticonvulsants like gabapentin?
For which condition is carbamazepine preferred?
For which condition is carbamazepine preferred?
What is a common side effect of tricyclic antidepressants?
What is a common side effect of tricyclic antidepressants?
Which pharmacologic approach is recommended for moderate pain (4-6)?
Which pharmacologic approach is recommended for moderate pain (4-6)?
What is the maximum daily dosage of acetaminophen for adults?
What is the maximum daily dosage of acetaminophen for adults?
Which of the following is NOT a common side effect of gabapentin?
Which of the following is NOT a common side effect of gabapentin?
What is the primary purpose of cognitive behavioral therapy in pain management?
What is the primary purpose of cognitive behavioral therapy in pain management?
Which medication is considered a first-line treatment for neuropathic pain?
Which medication is considered a first-line treatment for neuropathic pain?
What defines the severity of acute pain that would warrant an opioid for management?
What defines the severity of acute pain that would warrant an opioid for management?
What should be monitored when prescribing carbamazepine?
What should be monitored when prescribing carbamazepine?
Flashcards are hidden until you start studying
Study Notes
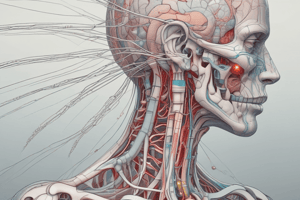
Classification of Pain
- Pain is categorized into two main types: nociceptive and neuropathic.
- Nociceptive Pain: Involves the body's transfer of information about tissue damage to the CNS.
- Occurs from chemical, thermal, or mechanical sources.
- Types:
- Somatic Pain:
- Originates in peripheral tissues; can be superficial or deep.
- Characterized by sharp, stabbing sensations or dull aches; usually located at a pinpoint site.
- Visceral Pain:
- Originates in internal organs.
- Described as cramping, deep squeezing, or pressure-like, often difficult to localize.
- Somatic Pain:
- Neuropathic Pain:
- Results from damage or disorders of the nervous system.
- Pain perception occurs without tissue damage due to factors like trauma, infection, or tumors.
- Commonly described as burning, shooting, or pricking sensations; includes allodynia and hyperalgesia.
- Pain is also classified as acute or chronic.
- Acute Pain:
- Sharp, dull, or tingling sensation; linked to identifiable stimuli; short duration.
- Signs include hypertension, tachycardia, tachypnea; may result in behavioral changes in infants/dementia.
- Examples: surgical pain, trauma.
- Chronic Pain:
- Persists for more than three months without a clear link to stimuli; may recur.
- Associated with comorbid conditions like cancer, fibromyalgia, or arthritis.
- Acute Pain:
Assessment of Pain
- Importance of thorough history and physical exams to identify underlying factors.
- Characterization tools include OLDCARTS, SOCRATES, SCHOLAR-MAC, and PQRSTU.
- OLDCARTS: Onset, Location, Duration, Characteristics, Alleviating/Aggravating factors, Radiating/Relieving factors, Timing, Severity.
- SOCRATES: Site, Onset, Character, Radiation, Associations, Time course, Exacerbating/Relieving factors, Severity.
- SCHOLAR-MAC: Symptoms, Characteristics, History, Onset, Location, Aggravating, Remitting, Medication, Allergies, Conditions.
- PQRSTU: Provoking/Palliating factors, Quality of pain, Region/Radiation, Severity, Timing, Understanding.
- Ongoing assessments include Wong-Baker Faces Scale, Brief Pain Inventory, and Numeric Rating Scale.
Goals of Therapy
- Objectives vary based on pain type:
- Acute Pain: Focus on recovery and prevention of chronic pain.
- Chronic Pain: Aim to improve function, decrease pain perception, and enhance quality of life.
Nonpharmacologic Therapy
- Approaches include exercise, physical therapy, dietary changes, weight loss, cognitive-behavioral therapy, tai chi, yoga, and acupuncture.
Principles of Pain Management
- Mild Pain (1-3):
- Treated with Acetaminophen (APAP) or NSAIDs.
- Regular dosing around the clock (ATC) is encouraged.
- Moderate Pain (4-6):
- Combination of opioids with APAP/NSAIDs.
- ATC and PRN dosing practices employed.
- Severe Pain (7-10):
- Opioids considered ATC; frequent reassessment for titration.
Pharmacologic Therapy
- Non-Opioid Analgesics:
- Includes APAP for mild to moderate pain and NSAIDs for inflammatory conditions.
- Co-Analgesics/Adjuvants:
- Anticonvulsants and antidepressants used to enhance pain management.
- Opioids:
- Morphine and its analogs are primary agents in severe cases.
Non-Opioid Analgesics for Nociceptive Pain
- Acetaminophen:
- Effective against mild to moderate pain; contraindicated in severe hepatic impairment.
- NSAIDs:
- Provide analgesic and anti-inflammatory effects; contraindications include active GI bleeding and renal impairment.
Co-Analgesics/Adjuvants
- Anticonvulsants:
- Gabapentin and pregabalin effective for neuropathic pain; renal dose adjustments necessary.
- Antidepressants:
- Enhance pain inhibition by inhibiting serotonin and norepinephrine reuptake; effective at lower doses than those used for depression.
Skeletal Muscle Relaxants
- Treat muscle spasms and spasticity; should be used cautiously and for limited durations.
- Side effects often include CNS depression and withdrawal symptoms.
Topical Agents
- Used to address localized pain with reduced systemic exposure.
- Capsaicin: Effective for neuropathic pain; requires consistent use for efficacy.
- Topical NSAIDs: Useful for localized pain like arthritis or sprains; low absorption risk.
Regional Anesthesia
- Involves local anesthetics for pain management in various forms (injections).
Miscellaneous Agents
- Corticosteroids: Used for inflammation and pain related to diseases; potential side effects including weight gain and osteoporosis.
- Cannabinoids: Indicated for chronic pain.
- Ketamine: Provides analgesic/anesthetic effects with potential CNS and psychiatric adverse events.
Opioid Analgesics
- Oral opioids have a delayed onset; morphine serves as the standard for comparison against other opioids.
- Special consideration needed for patients with renal impairment concerning morphine metabolites.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.