Podcast
Questions and Answers
A patient reports experiencing a sharp, localized pain after stubbing their toe. Which type of sensory fiber is primarily responsible for transmitting this initial, acute pain signal?
A patient reports experiencing a sharp, localized pain after stubbing their toe. Which type of sensory fiber is primarily responsible for transmitting this initial, acute pain signal?
- Aδ fibers (correct)
- C fibers
- Aα fibers
- B fibers
Which of the following is the most accurate description of the transduction phase of nociception?
Which of the following is the most accurate description of the transduction phase of nociception?
- The conversion of painful stimuli into electrical signals by nociceptors. (correct)
- The process by which the brain interprets pain signals and assigns meaning to them.
- The transmission of pain signals from the spinal cord to the thalamus and somatosensory cortex.
- The release of neurotransmitters in the spinal cord that either amplify or inhibit pain signals.
Following a sports injury, a patient is prescribed an NSAID to manage pain. How do NSAIDs exert their analgesic effects in the transduction phase of nociception?
Following a sports injury, a patient is prescribed an NSAID to manage pain. How do NSAIDs exert their analgesic effects in the transduction phase of nociception?
- By directly blocking sodium channels in the nociceptors, preventing action potential generation.
- By directly blocking the release of substance P in the spinal cord.
- By inhibiting the production of prostaglandins, reducing nociceptor activation. (correct)
- By enhancing the release of endorphins in the brain, thus diminishing pain perception.
A patient with chronic pain is found to have decreased levels of certain neurotransmitters. A deficiency in which of the following neurotransmitters would most likely impair the body's natural ability to modulate pain?
A patient with chronic pain is found to have decreased levels of certain neurotransmitters. A deficiency in which of the following neurotransmitters would most likely impair the body's natural ability to modulate pain?
A patient describes their pain as a dull, aching sensation that is difficult to pinpoint. Which specific characteristic of the nociceptive pain pathway is most closely associated with this type of pain experience?
A patient describes their pain as a dull, aching sensation that is difficult to pinpoint. Which specific characteristic of the nociceptive pain pathway is most closely associated with this type of pain experience?
A patient reports a deep, squeezing pain that is poorly localized. Based on the characteristics of nociceptive pain, which type of pain is the patient most likely experiencing?
A patient reports a deep, squeezing pain that is poorly localized. Based on the characteristics of nociceptive pain, which type of pain is the patient most likely experiencing?
Which of the following factors can influence an individual's perception of pain?
Which of the following factors can influence an individual's perception of pain?
A patient reports a pain that feels like an electric shock sensation down their leg. Which type of pain is this patient MOST likely experiencing?
A patient reports a pain that feels like an electric shock sensation down their leg. Which type of pain is this patient MOST likely experiencing?
A patient who has been on opioid medication long-term for chronic pain requires a higher dose to achieve the same level of pain relief. This phenomenon is best described as which of the following?
A patient who has been on opioid medication long-term for chronic pain requires a higher dose to achieve the same level of pain relief. This phenomenon is best described as which of the following?
Which of the following is the MOST likely treatment implication for a patient experiencing referred pain?
Which of the following is the MOST likely treatment implication for a patient experiencing referred pain?
Which of the opioid receptors listed below results in analgesia, diuresis, sedation, and pupil constriction?
Which of the opioid receptors listed below results in analgesia, diuresis, sedation, and pupil constriction?
In the context of acute pain, what is the significance of synaptic plasticity?
In the context of acute pain, what is the significance of synaptic plasticity?
A patient reports feeling pain in their left shoulder, but the examination reveals no injury to the shoulder itself. Further investigation reveals an issue with their spleen. This is an example of what kind of pain?
A patient reports feeling pain in their left shoulder, but the examination reveals no injury to the shoulder itself. Further investigation reveals an issue with their spleen. This is an example of what kind of pain?
Which of the following strategies aims to interrupt peripheral pain transmission as part of pain management?
Which of the following strategies aims to interrupt peripheral pain transmission as part of pain management?
What is the PRIMARY treatment goal for a patient experiencing chronic pain?
What is the PRIMARY treatment goal for a patient experiencing chronic pain?
Flashcards
Pain
Pain
An unpleasant sensory and emotional experience linked to tissue damage.
Nociceptive Pain
Nociceptive Pain
Pain resulting from actual or perceived tissue injury, detected by nociceptors.
Transduction
Transduction
The process of converting painful stimuli into action potentials by nociceptors.
Transmission
Transmission
Signup and view all the flashcards
Spinal Neurotransmitters
Spinal Neurotransmitters
Signup and view all the flashcards
Nociceptor pathways
Nociceptor pathways
Signup and view all the flashcards
Dermatome map
Dermatome map
Signup and view all the flashcards
Pain threshold
Pain threshold
Signup and view all the flashcards
Pain tolerance
Pain tolerance
Signup and view all the flashcards
Neuropathic pain
Neuropathic pain
Signup and view all the flashcards
Acute pain
Acute pain
Signup and view all the flashcards
Chronic pain
Chronic pain
Signup and view all the flashcards
Referred pain
Referred pain
Signup and view all the flashcards
Opioids
Opioids
Signup and view all the flashcards
Study Notes
Pain
- Pain is defined as "unpleasant sensory and emotional experience associated with actual or potential tissue damage" (IASP).
- The patient's subjective experience of pain is also considered (The Joint Commission).
- Pain serves to protect the body.
- It alerts the body to a dangerous situation.
- It allows the body to remove itself from the situation.
Types of Pain
- Nociceptive Pain:
- Treated with over-the-counter (OTC) analgesics.
- NSAIDs
- Tylenol
- Prescription analgesics, including opioids:
- Morphine
- Treated with over-the-counter (OTC) analgesics.
- Neuropathic Pain:
- Treated with anticonvulsants:
- Neurontin
- Lyrica
- Treated with anticonvulsants:
Nociceptive Pain
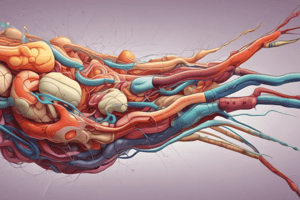
- Nociception: Pain receptors (nociceptors) respond to painful stimuli.
- Nociceptors transduce painful stimuli into action potentials.
- Chemical mediators involved in transduction include:
- Prostaglandins
- NSAIDs (inhibit prostaglandins)
- Lactate
- Kinins
- K+, H+
- Histamine
- Serotonin
Neuroanatomy of Pain
- Nociceptors are pain receptors.
- Nociceptive pain is pain resulting from actual or perceived tissue injury.
Nociceptive Pain Pathway
- Transduction: The process of converting painful stimuli to action potentials.
- Transmission: Spinal nerves transmit signals to the anterolateral tract and then to the thalamus.
- Perception: The brain interprets the signal as pain.
- Modulation: The process of suppressing or enhancing pain signals.
Transmission
- Spinal nerves transmit pain signals to the anterolateral tract, then the thalamus.
- Sensory fibers ascend.
- Aδ fibers (10%): fast, large, myelinated; sharp, stinging pain; highly localized
- C fibers (90%): slow, small, unmyelinated; dull, aching pain; poorly localized, lingering
- Spinal neurotransmitters include:
- Excitatory: Substance P, glutamate, histamine
- Inhibitory: Endorphins, norepinephrine, GABA, serotonin
How Does the Brain Localize Pain?
- Nociceptor pathways are organized in an anatomical order in the spinal cord and somatosensory cortex.
- Dermatome map
- Primary sensory cortex localizes pain.
Perception
- Neural processing of pain sensation is influenced by:
- Awareness
- Emotion/mood
- Prior experience
- Expectation
- Culture
- Physical status
- Sex/gender
Perception Concepts
- Pain threshold: The minimum intensity of a stimulus needed to produce pain.
- Pain tolerance: The maximum intensity of pain that a person can tolerate.
- Pain expression: The quantity and quality of pain.
Opioids
- Analgesia: Relieving pain
- Agents that bind to receptors: Morphine, naloxone, endorphins
- Manifestations: Diuresis, sedation, decreased respiratory rate (RR), pupil constriction, constipation, and nausea/vomiting (N/V)
- Other less common pain meds
Acute Pain
- Etiology: Tissue injury
- Characteristics: Pain resolves as injury heals; less than 3 months' duration
- Clinical Manifestations (CM): Self-report and SNS stimulation; increased heart rate (HR), RR, and blood pressure (BP); pallor/diaphoresis, hyperglycemia, dilated pupils, nausea/vomiting (N/V), and urine retention.
- Treatment Implications (TI): Short-acting opioid/non-opioid relief to maintain function/healing.
Chronic Pain
- Etiology: Underlying disease or unclear cause, comorbidities such as sleep disturbance and depression
- Characteristics: >6 months; increased peripheral transduction sensitivity, abnormal central responsiveness
- Clinical Manifestations (CM): Non-SNS responses, such as mood disturbances, inability to function, chronic hyperglycemia, fatigue/sleep problems, and weakened immune systems
- Treatment Implications (TI): Multimodal/Long-acting pain meds, including opioids, antidepressants, and anticonvulsants, to maintain function/quality of life.
Referred Pain
- Etiology: Injury at a different site.
- Characteristics: Referred to tissue in the same sensory dermatome; visceral nociceptor activity and primary somatic afferent nerves in the posterior horn of the spinal cord.
- Clinical Manifestations (CM): Various clinical manifestations
- Treatment Implications (TI): Relief of underlying injury
Treatment Implications for Pain
- Interrupt Peripheral Transmission:
- Thermal treatment: ↓ inflammation/swelling
- Local anesthetics: ↓ pain stimulus
- Splinting: ↓ further tissue injury/inflammation
- NSAIDs: ↓ prostaglandins ⇒↓ inflammation/pain
- Altering Perception & Integration:
- Medications: Opioids/Non-opioids, anticonvulsants, antidepressants
- Non-medications: Distraction, imagery, relaxation, biofeedback, hypnosis
Neuropathic Pain
- Etiology: Possible tissue injury to the nerves; nerve damage or dysfunction, altered central processing of nociceptive input
- Characteristics: Shooting, burning, electric shock-like, tingling/pins-and-needles pain
- Treatment Implications (TI): Maintain functional ability and quality of life with anticonvulsants and antidepressants (TCAs).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.