Podcast
Questions and Answers
Which statement best describes the nature of pain?
Which statement best describes the nature of pain?
- Pain can only become chronic if it is associated with nociceptive processes.
- Pain is solely a sensory experience without emotional aspects.
- Pain always arises from immediate physical injury.
- Pain is an unpleasant experience that can be linked to both actual and potential tissue damage. (correct)
What is the primary role of nociceptors in the pain experience?
What is the primary role of nociceptors in the pain experience?
- To activate mechanisms that block pain transmission.
- To process and interpret pain signals in the brain.
- To enhance the perception of pain by amplifying signals.
- To detect noxious stimuli that may cause tissue damage. (correct)
Which type of pain is characterized by damage to peripheral nerves?
Which type of pain is characterized by damage to peripheral nerves?
- Referred pain
- Nociplastic pain
- Neuropathic pain (correct)
- Secondary pain
Which of the following medications is primarily used for managing nociceptive pain?
Which of the following medications is primarily used for managing nociceptive pain?
What is a significant social consequence of pain medication misuse?
What is a significant social consequence of pain medication misuse?
Which type of pain is characterized by being caused by damage to the nervous system?
Which type of pain is characterized by being caused by damage to the nervous system?
Which symptom is classified as a positive symptom of neuropathic pain?
Which symptom is classified as a positive symptom of neuropathic pain?
What differentiates nociplastic pain from other pain types?
What differentiates nociplastic pain from other pain types?
Which of the following describes acute pain?
Which of the following describes acute pain?
What is an example of mixed pain?
What is an example of mixed pain?
What characterizes chronic primary pain?
What characterizes chronic primary pain?
Which of the following describes hyperalgesia?
Which of the following describes hyperalgesia?
What is the primary function of nociceptors?
What is the primary function of nociceptors?
Which type of pain is linked to an underlying condition?
Which type of pain is linked to an underlying condition?
Which of the following is an emotional response to pain?
Which of the following is an emotional response to pain?
What does the visual analogue scale measure?
What does the visual analogue scale measure?
Which sensory experience is defined as 'pins and needles'?
Which sensory experience is defined as 'pins and needles'?
Which of the following factors can influence the subjective experience of pain?
Which of the following factors can influence the subjective experience of pain?
What is the primary action of inflammatory mediators like prostaglandins and bradykinin?
What is the primary action of inflammatory mediators like prostaglandins and bradykinin?
Which of the following medications is specifically classified as an irreversible NSAID?
Which of the following medications is specifically classified as an irreversible NSAID?
What is a key characteristic of COX II inhibitors compared to traditional NSAIDs?
What is a key characteristic of COX II inhibitors compared to traditional NSAIDs?
What is the main therapeutic use of paracetamol?
What is the main therapeutic use of paracetamol?
Which type of receptor is not one of the five main opioid receptors?
Which type of receptor is not one of the five main opioid receptors?
What is the mechanism of action for endogenous opioids on the neuronal level?
What is the mechanism of action for endogenous opioids on the neuronal level?
What is the role of enkephalinase in pain modulation?
What is the role of enkephalinase in pain modulation?
Which of the following NSAIDs is known to have anti-pyretic properties?
Which of the following NSAIDs is known to have anti-pyretic properties?
What percentage of heroin addicts began their addiction with OxyContin?
What percentage of heroin addicts began their addiction with OxyContin?
Which medication is considered most effective for managing neuropathic pain?
Which medication is considered most effective for managing neuropathic pain?
What is a common adverse effect of nerve block procedures when local anesthetics are used?
What is a common adverse effect of nerve block procedures when local anesthetics are used?
Which statement explains the pharmacological mechanism of gabapentanoids?
Which statement explains the pharmacological mechanism of gabapentanoids?
Why was Purdue Pharma sued for bad business practices?
Why was Purdue Pharma sued for bad business practices?
What type of pain does Ciara experience after six months with no response to diclofenac?
What type of pain does Ciara experience after six months with no response to diclofenac?
What formulation did Purdue Pharma develop to deliver oxycodone effectively?
What formulation did Purdue Pharma develop to deliver oxycodone effectively?
What role do non-steroidal anti-inflammatory drugs (NSAIDs) play in nerve block procedures?
What role do non-steroidal anti-inflammatory drugs (NSAIDs) play in nerve block procedures?
What is the primary reason why visceral pain is referred to areas far from the site of the stimulus?
What is the primary reason why visceral pain is referred to areas far from the site of the stimulus?
Which neurotransmitter is NOT typically involved in pain neurotranmission?
Which neurotransmitter is NOT typically involved in pain neurotranmission?
According to the gate control theory of modulation, what influences the modulation of pain perception?
According to the gate control theory of modulation, what influences the modulation of pain perception?
In the context of visceral pain, what does the term 'dermatome' refer to?
In the context of visceral pain, what does the term 'dermatome' refer to?
Which of these statements about pain modulation is true?
Which of these statements about pain modulation is true?
What role does the NMDA receptor play in pain perception?
What role does the NMDA receptor play in pain perception?
Which type of neuron is primarily responsible for transmitting visceral pain to the spinal cord?
Which type of neuron is primarily responsible for transmitting visceral pain to the spinal cord?
What substance is associated with the modulation of pain through the descending pathways?
What substance is associated with the modulation of pain through the descending pathways?
What is the primary role of endogenous opioids in pain modulation?
What is the primary role of endogenous opioids in pain modulation?
Which neurotransmitter is primarily involved in the descending modulation of pain?
Which neurotransmitter is primarily involved in the descending modulation of pain?
Where are opioid receptors primarily located in the central nervous system?
Where are opioid receptors primarily located in the central nervous system?
What is the effect of cannabinoids like anandamide in the context of pain?
What is the effect of cannabinoids like anandamide in the context of pain?
What is a significant characteristic of the descending pain pathways?
What is a significant characteristic of the descending pain pathways?
Which type of receptor is activated by endocannabinoids to mediate pain relief?
Which type of receptor is activated by endocannabinoids to mediate pain relief?
In which area are the main types of opioid receptors found?
In which area are the main types of opioid receptors found?
What type of neuronal transmission do endogenous opioids primarily inhibit?
What type of neuronal transmission do endogenous opioids primarily inhibit?
Which of the following medications is primarily indicated for chronic migraine prevention?
Which of the following medications is primarily indicated for chronic migraine prevention?
Which mechanism of action is associated with Ubrogepant in the treatment of migraines?
Which mechanism of action is associated with Ubrogepant in the treatment of migraines?
Which of the following is NOT a type of migraine prophylaxis medication?
Which of the following is NOT a type of migraine prophylaxis medication?
What class of drugs does lasmiditan belong to in the context of migraine treatment?
What class of drugs does lasmiditan belong to in the context of migraine treatment?
Which medication is associated with chronic migraine only?
Which medication is associated with chronic migraine only?
What is the recommended first-line pharmacotherapy for chronic low back pain when NSAIDs are ineffective?
What is the recommended first-line pharmacotherapy for chronic low back pain when NSAIDs are ineffective?
Which demographic factors are associated with increased likelihood of prescription opioid use?
Which demographic factors are associated with increased likelihood of prescription opioid use?
What type of pain is chronic low back pain classified as?
What type of pain is chronic low back pain classified as?
Which of the following best describes neurogenic inflammation?
Which of the following best describes neurogenic inflammation?
What is a potential serious side effect associated with the use of duloxetine?
What is a potential serious side effect associated with the use of duloxetine?
Which component of tramadol acts as an opioid receptor agonist?
Which component of tramadol acts as an opioid receptor agonist?
What is the primary symptom associated with migraine as a result of neurogenic inflammation?
What is the primary symptom associated with migraine as a result of neurogenic inflammation?
When managing low back pain, which therapeutic approach is considered second-line treatment?
When managing low back pain, which therapeutic approach is considered second-line treatment?
What is the primary function of nalmefene?
What is the primary function of nalmefene?
Which of the following correctly describes the half-life characteristics of naltrexone?
Which of the following correctly describes the half-life characteristics of naltrexone?
What is a significant challenge in treating overdose when xylazine is involved?
What is a significant challenge in treating overdose when xylazine is involved?
Which of the following statements reflects a key concern regarding opioid use in the U.S.?
Which of the following statements reflects a key concern regarding opioid use in the U.S.?
Methylnaltrexone, a peripherally acting antagonist, is specifically approved for which condition?
Methylnaltrexone, a peripherally acting antagonist, is specifically approved for which condition?
Which of the following is true about the opioid epidemic in the U.S. as of 2023?
Which of the following is true about the opioid epidemic in the U.S. as of 2023?
Which mechanism of action is NOT clearly associated with the therapeutic effects of naltrexone?
Which mechanism of action is NOT clearly associated with the therapeutic effects of naltrexone?
What is the effect of using xylazine as an additive in opioid formulations?
What is the effect of using xylazine as an additive in opioid formulations?
What is a significant side effect of morphine that affects breathing?
What is a significant side effect of morphine that affects breathing?
Which opioid agonist is over 100 times more potent than morphine?
Which opioid agonist is over 100 times more potent than morphine?
What is the primary mechanism by which codeine alleviates pain?
What is the primary mechanism by which codeine alleviates pain?
What is one of the main reasons why novel opioids like nitazines are not clinically used?
What is one of the main reasons why novel opioids like nitazines are not clinically used?
Which receptor type does naloxone primarily act as an antagonist upon?
Which receptor type does naloxone primarily act as an antagonist upon?
What is a characteristic effect of μ opioid receptor activation?
What is a characteristic effect of μ opioid receptor activation?
Which of the following side effects is directly related to morphine's action in the gastrointestinal tract?
Which of the following side effects is directly related to morphine's action in the gastrointestinal tract?
How is the duration of action of morphine enhanced?
How is the duration of action of morphine enhanced?
Which opioid is specifically designed to prevent constipation while providing analgesic effects?
Which opioid is specifically designed to prevent constipation while providing analgesic effects?
What is an important diagnostic indicator of morphine overdose?
What is an important diagnostic indicator of morphine overdose?
Which protein is NOT part of the CGRP receptor complex?
Which protein is NOT part of the CGRP receptor complex?
Which of the following statements about migraine treatment is correct?
Which of the following statements about migraine treatment is correct?
What percentage of migraine attacks is associated with aura?
What percentage of migraine attacks is associated with aura?
Which medication is classified as an ergot alkaloid in the context of migraine treatment?
Which medication is classified as an ergot alkaloid in the context of migraine treatment?
What was the global prevalence of people affected by migraine in 2016?
What was the global prevalence of people affected by migraine in 2016?
Which receptor is NOT involved in the mechanism of action of sumatriptan?
Which receptor is NOT involved in the mechanism of action of sumatriptan?
Which is a key reason for the adverse effects of ergotamine?
Which is a key reason for the adverse effects of ergotamine?
What is a significant problem associated with migraine treatment using sumatriptan?
What is a significant problem associated with migraine treatment using sumatriptan?
Flashcards
Pain definition
Pain definition
Unpleasant sensory & emotional experience from/resembling actual or potential tissue damage.
Pain mechanism
Pain mechanism
Pain is a normal response to injury, primarily protective. It can become chronic and pathological.
Nociceptor activation
Nociceptor activation
Activation of nerve endings (nociceptors) due to noxious stimuli such as injury.
Pain pathways
Pain pathways
Signup and view all the flashcards
Pain modulation
Pain modulation
Signup and view all the flashcards
Neuropathic Pain
Neuropathic Pain
Signup and view all the flashcards
Nociceptive Pain
Nociceptive Pain
Signup and view all the flashcards
Chronic Pain
Chronic Pain
Signup and view all the flashcards
Deafferentation Pain
Deafferentation Pain
Signup and view all the flashcards
Nociplastic Pain
Nociplastic Pain
Signup and view all the flashcards
Chronic Primary Pain
Chronic Primary Pain
Signup and view all the flashcards
Chronic Secondary Pain
Chronic Secondary Pain
Signup and view all the flashcards
Pain Perception
Pain Perception
Signup and view all the flashcards
Hyperalgesia
Hyperalgesia
Signup and view all the flashcards
Allodynia
Allodynia
Signup and view all the flashcards
Paresthesia
Paresthesia
Signup and view all the flashcards
Dysesthesia
Dysesthesia
Signup and view all the flashcards
Nociceptor
Nociceptor
Signup and view all the flashcards
Visceral Pain
Visceral Pain
Signup and view all the flashcards
Referred Pain
Referred Pain
Signup and view all the flashcards
How is Referred Pain Explained?
How is Referred Pain Explained?
Signup and view all the flashcards
Substantia Gelatinosa
Substantia Gelatinosa
Signup and view all the flashcards
GABA, Opioids, eCBs
GABA, Opioids, eCBs
Signup and view all the flashcards
Gate Control Theory
Gate Control Theory
Signup and view all the flashcards
Descending Pathways
Descending Pathways
Signup and view all the flashcards
OxyContin's Promise
OxyContin's Promise
Signup and view all the flashcards
OxyContin's Impact
OxyContin's Impact
Signup and view all the flashcards
Purdue's Consequences
Purdue's Consequences
Signup and view all the flashcards
Gabapentinoids for Neuropathic Pain
Gabapentinoids for Neuropathic Pain
Signup and view all the flashcards
Nerve Blocks for Pain Relief
Nerve Blocks for Pain Relief
Signup and view all the flashcards
Opioids for Low Back Pain - OPAL Study
Opioids for Low Back Pain - OPAL Study
Signup and view all the flashcards
Local Anesthetics and Nerve Block
Local Anesthetics and Nerve Block
Signup and view all the flashcards
Inflammatory Pain
Inflammatory Pain
Signup and view all the flashcards
NSAID's Action
NSAID's Action
Signup and view all the flashcards
COXIBs
COXIBs
Signup and view all the flashcards
Paracetamol's Mystery
Paracetamol's Mystery
Signup and view all the flashcards
Opioid Definition
Opioid Definition
Signup and view all the flashcards
Enkephalinase
Enkephalinase
Signup and view all the flashcards
Opioid Receptors
Opioid Receptors
Signup and view all the flashcards
Opioids' Action
Opioids' Action
Signup and view all the flashcards
Descending Pain Modulation
Descending Pain Modulation
Signup and view all the flashcards
Where does descending pain modulation originate?
Where does descending pain modulation originate?
Signup and view all the flashcards
What neurotransmitters are involved in descending pain modulation?
What neurotransmitters are involved in descending pain modulation?
Signup and view all the flashcards
What are endogenous opioids?
What are endogenous opioids?
Signup and view all the flashcards
How do endogenous opioids work?
How do endogenous opioids work?
Signup and view all the flashcards
What are the main types of opioid receptors?
What are the main types of opioid receptors?
Signup and view all the flashcards
What are endocannabinoids?
What are endocannabinoids?
Signup and view all the flashcards
Where are cannabinoid receptors located?
Where are cannabinoid receptors located?
Signup and view all the flashcards
Naltrexone
Naltrexone
Signup and view all the flashcards
Methylnaltrexone
Methylnaltrexone
Signup and view all the flashcards
Nalmefene
Nalmefene
Signup and view all the flashcards
Xylazine
Xylazine
Signup and view all the flashcards
Opioid Epidemic
Opioid Epidemic
Signup and view all the flashcards
MME
MME
Signup and view all the flashcards
Opioid Addiction Risk Factors
Opioid Addiction Risk Factors
Signup and view all the flashcards
US Child Poverty Rate
US Child Poverty Rate
Signup and view all the flashcards
Morphine's Action
Morphine's Action
Signup and view all the flashcards
Morphine's Side Effects
Morphine's Side Effects
Signup and view all the flashcards
What is fentanyl's potency?
What is fentanyl's potency?
Signup and view all the flashcards
What is naloxone?
What is naloxone?
Signup and view all the flashcards
What is the purpose of Targin?
What is the purpose of Targin?
Signup and view all the flashcards
What is Tramadol's action?
What is Tramadol's action?
Signup and view all the flashcards
What are Nitazines?
What are Nitazines?
Signup and view all the flashcards
What is the role of the red pathway?
What is the role of the red pathway?
Signup and view all the flashcards
What's the significance of CYP2D6?
What's the significance of CYP2D6?
Signup and view all the flashcards
How are opioids broken down?
How are opioids broken down?
Signup and view all the flashcards
Chronic Low Back Pain
Chronic Low Back Pain
Signup and view all the flashcards
What are the first-line treatments for Chronic Low Back Pain?
What are the first-line treatments for Chronic Low Back Pain?
Signup and view all the flashcards
Duloxetine
Duloxetine
Signup and view all the flashcards
Tramadol
Tramadol
Signup and view all the flashcards
Neurogenic Inflammation
Neurogenic Inflammation
Signup and view all the flashcards
CGRP (Calcitonin Gene-Related Peptide)
CGRP (Calcitonin Gene-Related Peptide)
Signup and view all the flashcards
Migraines
Migraines
Signup and view all the flashcards
CGRP Receptor Complex
CGRP Receptor Complex
Signup and view all the flashcards
CGRP's Role in Migraine
CGRP's Role in Migraine
Signup and view all the flashcards
Triptan Medications
Triptan Medications
Signup and view all the flashcards
Migraine Prevalence
Migraine Prevalence
Signup and view all the flashcards
Tension Headache Prevalence
Tension Headache Prevalence
Signup and view all the flashcards
Acute Migraine Treatment
Acute Migraine Treatment
Signup and view all the flashcards
Ergotamine for Migraine
Ergotamine for Migraine
Signup and view all the flashcards
Sumatriptan for Migraine
Sumatriptan for Migraine
Signup and view all the flashcards
CGRP and Migraines
CGRP and Migraines
Signup and view all the flashcards
Migraine Prophylaxis
Migraine Prophylaxis
Signup and view all the flashcards
What are 5HT1F agonists?
What are 5HT1F agonists?
Signup and view all the flashcards
What are triptans?
What are triptans?
Signup and view all the flashcards
What are CGRP receptor antibodies?
What are CGRP receptor antibodies?
Signup and view all the flashcards
Study Notes
Course Information
- Class: MED Y2
- Module: CNS
- Facilitator: Niamh Connolly ([email protected])
- Facilitator: Dermot Cox ([email protected])
- Date: 5th November 2024
Learning Outcomes I
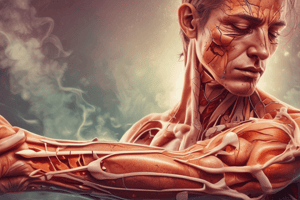
- Define and describe pain as a physiological and pathophysiological process
- Describe the mechanisms of activation of nociceptors
- Describe ascending pain pathways including specific, non-specific pathways, and areas of higher cortical processing
- Describe pain modulation at the level of spinal cord and along descending pathways
- Describe the different types of pain such as referred, primary, secondary, nociceptive, neuropathic and nociplastic
Learning Outcomes II
- Outline the use of opioids and NSAIDs in nociceptive pain
- Describe the role of a multi-disciplinary approach to managing nociplastic and chronic pain
- Describe the mechanism of action and adverse effects of:
- drugs that target neuropathic pain
- drugs that control migraine
- local anaesthetics
- general anaesthetics
- Describe the social consequences of misuse and over use of pain medication
Pain - Definition
- "An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage"
- Pain refers to noxious stimuli.
- Pain is a normal response to injury
- Primarily a protective mechanism, and can promote repair
- Can become pathological, chronic
- Pain is typically invoked by tissue damage (not always – e.g. neuropathic pain)
Types of Pain
- Nociceptive pain: Pain caused by the activation of nociceptors, e.g., trauma
- Neuropathic pain: Pain caused by damage (injury/disease) to the nervous system.
- Central, e.g., spinal cord injury, multiple sclerosis (MS)
- Peripheral, e.g., diabetic neuropathy, post-surgery neuropathic pain
- Negative symptoms: sensory loss, numbness
- Positive symptoms: spontaneous pain, increased pain sensation
- Deafferentation pain: occurs following peripheral nerve lesions such as phantom limb pain
- Nociplastic pain (psychogenic pain): Persistent pain arising from altered nociception, despite no clear evidence of activation of peripheral nociceptors.
- Examples: Fibromyalgia, migraine
- Mixed pain: Both nociceptive and neuropathic, e.g., cancer pain
Acute vs Chronic Pain
- Acute pain (seconds): Experienced with real or potential tissue damage, appropriate protective mechanism
- Sub-acute (hours-days): Associated with tissue damage and infiltration of immune cells, can promote repair
- Chronic pain - pathological (months-years): Lasts longer than damage, neither protects nor supports repair, often requires treatment.
- Chronic primary pain: unclear underlying cause
- Chronic secondary pain: linked to an underlying condition
Multiple Responses to Painful Stimuli
- Spinal withdrawal reflex
- Conscious perception of pain
- Autonomic nervous system (ANS) changes (e.g., increased alertness associated with pain)
- Emotional responses (e.g., fear, depression, anxiety, hopelessness)
- Pain behaviours (e.g., grimacing, limping, avoiding activities)
Perception of Pain
- Pain perception has informational and motivational components (location, intensity, modality)
- Pain perception can be altered, including hyperalgesia (increased sensitivity to painful stimuli) and allodynia (pain in response to non-noxious stimuli).
- Past experience, attention, interpretation, and other contextual factors influence subjective pain experience
Clinical Characterisation of Pain
- Sensations:
- Paresthesia: pins and needles
- Dysesthesia: burning sensation
- Other clinical characteristics such as burning, stabbing, electric shock-like (nerve pain) and tenderness, achiness, and stiffness (muscle pain)
Clinical Characterisation of Pain - Visual Analogue Scale
- Visual analogue scale (VAS) used to quantify pain experience
Pain Sensory Receptors = Nociceptors
- Nociceptors: Free peripheral nerve endings of Aδ and C fibres that are excited by noxious or painful stimuli
- Stimuli include mechanical (intense pressure or stretch), thermal (extremes of hot or cold), and chemical stimuli.
- Chemical stimuli can cause or potentially cause tissue damage and release substances that either activate nociceptors directly or sensitize them.
- Examples include bradykinin (BK), prostaglandins (PG), ATP, and H+.
Nociception = Transduction of Painful Stimuli
- Detection of noxious stimuli by nociceptors
- Transduction of electrical signal to the CNS
Pain Fibres (I & II)
- Aδ fibres: Thinly myelinated fibres, speed of conduction ~5-35 m/s, trigger immediate withdrawal, produce sharp, localised, immediate pain
- C fibres: Slow, unmyelinated fibres, speed of conduction 0.5-2.0 m/s, produce dull, diffuse pain (secondary pain), relay information via the thalamus to cortex, limbic system, and hypothalamus, and trigger memory of stimulus.
Pain Pathways
- Conventional pathway is a 3-neuron system
- Primary pain afferent to spinal cord, contralateral spinothalamic tract to thalamus, thalamus to sensory cortex
- Sensory neurons from one side of the body project to the sensory cortex on the contralateral side
- Pain from the face travels in cranial nerves (different pathways)
Nociceptive Fibres in Spinal Cord
- Primary afferent neurons (Aδ and C fibres): transmit from nociceptor to the spinal cord via the dorsal root.
- On entering the spinal cord, they ascend/descend in the tract of Lissauer.
- Synapse with 2nd order neurons in superficial layers (laminae) of the dorsal horn.
- Aδ fibers – synapse in layers I and V (some synapse in layer II)
- C fibers – synapse in layer II (substantia gelatinosa)
- 2nd order neurons: Axons cross(decussate), ascend in contralateral spinothalamic tract, synapse with 3rd order neurons in thalamus.
- 3rd order neurons: axons project from thalamus to somatosensory cortex.
Ascending Pain Pathways (Specific & Non-Specific)
- Specific pathways: relay information about a single type of stimulus to specific areas of the cerebral cortex involved in localization and pain perception.
- Non-specific pathways: relay information from more than one type of sensory unit to the brainstem reticular formation and regions of the thalamus that are not part of the specific pathways. Involves behavioral responses.
Visceral Pain - Referred Pain
- Visceral pain is poorly localized and felt in areas far away from the stimulus site.
- Peripheral afferent neurons from viscera converge on the same spinothalamic neurons from the same spinal segment as skin afferents
- Brain interprets visceral pain as coming from the area of skin that shares the same pathway.
- Pain is referred to somatic structures, quite far from the internal organ.
Pain - Neurotransmission
- Neurotransmitters involved in pain transmission include glutamate, NMDA, AMPA, and NK1 receptors.
- Inhibitory neurons in the substantia gelatinosa use GABA, opioids, and endocannabinoids to modulate pain.
Modulation of Pain Perception
- Pain perception can be magnified or suppressed (modulation).
- Gate control theory: somatic non-painful signals can inhibit pain signal transmission.
- Descending pathways influence dorsal horn modulation.
- Endogenous opioids play a role.
Pain Modulation: Descending/Analgesic Pathways
- Descending analgesic pathways modulate pain.
- Periaqueductal gray matter and rostroventral medulla involved.
- Endogenous opioid release from descending analgesic pathways bind with opioid receptors on afferent pain fibers inhibiting glutamate and substance p release.
Pain Modulation: Descending Control
- Pain can be modulated by descending pathways originating from the brainstem (e.g., peri-ventricular/per-aqueductal grey matter, rostroventral medulla, including raphe nuclei and locus coeruleus)
- Descending fibers reduce nociceptor transmission through neurotransmitters such as serotonin and noradrenaline.
- Endogenous opioids and endocannabinoids also involved.
Endogenous Opioids
- Neuropeptides associated with analgesic modulation (endorphins, enkephalins, dynorphins, endomorphins, orphanin-FQ/nociceptin)
- Opioid receptors (μ, δ, κ) expressed in the dorsal horn.
- Binding at presynaptic sites inhibits substance P and glutamate release; at postsynaptic sites, reduces depolarisation.
Endocannabinoids
- Anandamide and 2-arachidonylglycerol (2-AG) mediate their analgesic effect via activation of cannabinoid receptors (CB1 and CB2).
- Reduce neurotransmitter release, and attenuate nociceptive responses.
Clinical Characterisation of Pain- Visual Analogue Scale (VAS)
- Visual analogue scale (VAS) used to quantify pain experience.
Case: Spinal Injury
- Mark has a spinal injury and is experiencing neuropathic pain.
- Management includes appropriate pain treatment strategy and consideration of appropriate medications.
Inflammatory Pain
- Inflammatory mediators (e.g., prostaglandins, 5-HT, bradykinin) sensitize pain fibres.
- They don't directly cause pain but sensitize fibres, increasing their response to pain signals
NSAIDs
- Act to inhibit cyclooxygenase (COX) and prostaglandin (PG) production.
- Are anti-inflammatory, analgesic, and anti-pyretic.
- Examples: Aspirin, ibuprofen, indomethacin
Anti-inflammatory Drugs
- Inflammation is a major cause of pain
- Due to specific inflammatory mediators sensitizing pain fibres.
- Prostaglandins and calcitonin gene-related peptide primarily involved.
COXIBs
- COX-II inhibitors (celecoxib, rofecoxib) developed for protection of gastric mucosa.
- Have similar efficacy to non-selective inhibitors with reduced GI side effects (~50%).
Paracetamol
- Technically not an NSAID; used for fever and pain (not inflammation).
- Mechanism of action unclear but linked to COX II selective inhibition and its major metabolite NAPQI that activates TRPA1 in the spinal cord.
Opioid Analgesics
- Opiate: compounds related to opium poppy (e.g., morphine)
- Opioid: natural or synthetic compounds mimicking opiate-like effects
Endogenous Opioids
- Endorphins, enkephalins, dynorphins, endomorphins, orphanin-FQ/nociceptin
- Main types: μ (MOR), δ (DOR), κ (KOR).
Enkephalinase Inhibitor
- Enkephalinase breaks down enkephalins.
- Thiorphan (active metabolite of racecadotril) used as an anti-diarrheal.
- Research ongoing for enkephalinase inhibitors for pain control.
Opioid Receptors
- Five types of opioid receptor (μ, κ, δ, nociceptin/orphanin FQ, opioid growth factor receptor)
- G-protein-linked.
- Promote opening of K+ channels, reduce neuronal excitability, and inhibit opening of voltage-gated Ca2+ channels.
Case: Low Back Pain
- 39-year-old Ciara with acute lower back pain, treated with diclofenac and physiotherapy, persists with pain
- Determine the appropriate pain management strategy.
OPAL Study
- Opioids showed borderline significance in managing low back/neck pain.
Epidemiology and Public Health Aspects of Pain
- Pain is pervasive and costly in terms of human suffering and economic burden.
- Several risk factors for opioid misuse/addiction exist, including poverty and mental illness; early-onset addiction is common.
Case: Headache
- 29-year-old Shirley with recurrent headaches with visual disturbances, nausea prior to headache onset.
- Determine the appropriate pain management strategy.
Neurogenic Inflammation
- Neurogenic inflammation is due to release of inflammatory mediators (especially neuropeptides) from small-diameter primary afferent C-fibres, causing vasodilation.
- Calcitonin gene-related peptide (CGRP) a key mediator.
- Migraine is an example of neurogenic inflammation. The mechanisms of pain and inflammation are complex.
Phases of Migraine
- Migraine has different phases, including prodrome (early warning signs), aura (sensory disturbances), headache (throbbing pain), and postdrome (symptoms after headache)
Migraine Prevalence Global 2016
- Tension-type headache - 1.89 billion people affected, 7.2M years lived with disability
- Migraine - 1.04 billion people affected, 45.1M years lived with disability
Acute Migraine Treatment
- NSAIDs and/or paracetamol.
- Anti-emetics.
- Triptans (5-HT1 agonists, e.g., frovatriptan, zolmitriptan), ergotamine (ergot alkaloid, 5HT1 agonist).
- Sumatriptan (highly effective but expensive) Ubrogepant and Lasmiditan (5-HT1F agonists)
Migraine-Prophylaxis
- Treatment to prevent migraine attacks, including avoiding triggers.
- Treatments: Beta-adrenoreceptor antagonists, amitriptyline (anti-depressant), topiramate (anti-psychotic), OnabotulinumtoxinA (Botox), and Anti-calcitonin gene-related peptide treatment
Targeting CGRP
- Anti-CGRP receptor antibodies (e.g., erenumab, fremanezumab, galcanezumab, eptinezumab)
- Small molecule CGRP antagonists (e.g., ubrogepant, rimegepant)
Case: Low Back Pain (cont.)
- Determine the appropriate pain management strategy.
Managing Nociplastic Pain
- Exercise therapy is standard therapy.
- Cognitive behavioural therapy (CBT) and mind-body interventions (e.g., mindfulness-based stress reduction (MBSR)) and progressive relaxation may be needed, especially for chronic pain.
- Pharmacotherapy (NSAIDS, duloxetine, tramadol) may be considered in some cases.
Duloxetine
- Serotonin and norepinephrine reuptake inhibitor (SNRI) used in chronic pain.
- Risk of suicide ideation and suicide especially pertinent in young populations
Tramadol
- Racemic mixture of (+)- and (-)-enantiomers.
- (+) Tramadol: μ opioid agonist, inhibits serotonin reuptake
- (-) Tramadol: Inhibits Noradrenaline (NA) reuptake.
- Important to use with caution due to potential for dependence.
Nerve Block
- Injection of local anaesthetic into nerve plexus, used for pain management.
- Potentially including NSAIDs/steroid.
- Locally reduces sodium ion channel activity leading to the inhibition of nerve conduction.
Nerve Block Adverse effects
- Seizures and heart failure at higher doses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.