Podcast
Questions and Answers
The kidneys are responsible for the regulation of acid-base balance through bicarbonate and hydrogen ion regulation.
The kidneys are responsible for the regulation of acid-base balance through bicarbonate and hydrogen ion regulation.
True (A)
The bladder has a storage capacity of approximately 200-300 mL.
The bladder has a storage capacity of approximately 200-300 mL.
False (B)
Ureters are tubes that carry urine from the bladder to the outside of the body.
Ureters are tubes that carry urine from the bladder to the outside of the body.
False (B)
Urine formation involves the processes of filtration, reabsorption, and secretion.
Urine formation involves the processes of filtration, reabsorption, and secretion.
Electrolyte balance is maintained by the secretion of hydrogen ions.
Electrolyte balance is maintained by the secretion of hydrogen ions.
Urinary tract infections (UTIs) are common disorders that can cause pain and urgency.
Urinary tract infections (UTIs) are common disorders that can cause pain and urgency.
The kidneys are located in the upper abdomen.
The kidneys are located in the upper abdomen.
The urethra is longer in females than in males.
The urethra is longer in females than in males.
The renin-angiotensin system helps regulate blood pressure.
The renin-angiotensin system helps regulate blood pressure.
Reabsorption of glucose primarily occurs in the heart.
Reabsorption of glucose primarily occurs in the heart.
EPSPs result in hyperpolarization of the postsynaptic membrane.
EPSPs result in hyperpolarization of the postsynaptic membrane.
Serotonin is classified as a monoamine neurotransmitter.
Serotonin is classified as a monoamine neurotransmitter.
Dopamine is only involved in motor control.
Dopamine is only involved in motor control.
IPSPs lead to depolarization of the postsynaptic cell.
IPSPs lead to depolarization of the postsynaptic cell.
The axon initial segment is crucial for the initiation of action potentials.
The axon initial segment is crucial for the initiation of action potentials.
Norepinephrine and dopamine are both classified as amino acid neurotransmitters.
Norepinephrine and dopamine are both classified as amino acid neurotransmitters.
The function of serotonin is primarily linked to the regulation of sleep.
The function of serotonin is primarily linked to the regulation of sleep.
Calmodulin is directly responsible for releasing neurotransmitters into the synaptic cleft.
Calmodulin is directly responsible for releasing neurotransmitters into the synaptic cleft.
The activation of chemically-regulated gated ion channels leads to changes in the postsynaptic membrane potential.
The activation of chemically-regulated gated ion channels leads to changes in the postsynaptic membrane potential.
Dopamine is solely produced in the cerebellum.
Dopamine is solely produced in the cerebellum.
Flashcards are hidden until you start studying
Study Notes
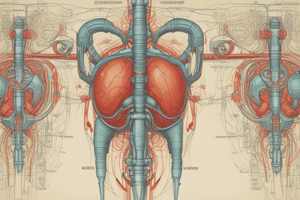
Overview of the Urinary System
- Responsible for the production, storage, and elimination of urine.
- Maintains the body's fluid balance, electrolyte levels, and acid-base balance.
Major Components
-
Kidneys
- Bean-shaped organs located in the lower back.
- Functions:
- Filtration of blood to form urine.
- Regulation of blood pressure through the renin-angiotensin system.
- Maintenance of electrolyte balance (sodium, potassium, calcium).
- Acid-base balance through bicarbonate and hydrogen ion regulation.
-
Ureters
- Two tubes connecting kidneys to the bladder.
- Function:
- Transport urine via peristaltic movements to the bladder.
-
Bladder
- Muscular sac that stores urine.
- Contains stretch receptors that signal the need to urinate.
- Has a capacity of approximately 400-600 mL.
-
Urethra
- Tube that carries urine from the bladder to the outside of the body.
- Longer in males (approximately 20 cm) than in females (approximately 4 cm).
- Contains sphincters that control urination.
Urine Formation Process
-
Filtration
- Occurs in the glomeruli of the kidneys.
- Blood plasma is filtered to remove waste products and excess substances.
-
Reabsorption
- Essential substances (water, glucose, electrolytes) are reabsorbed into the bloodstream.
- Primarily occurs in the renal tubules.
-
Secretion
- Additional waste products and excess ions are secreted into the urine.
- Helps regulate blood pH and maintain electrolyte balance.
Homeostatic Functions
- Fluid Balance: Regulates water retention and loss.
- Electrolyte Balance: Maintains optimal levels of ions (sodium, potassium, etc.).
- Acid-Base Balance: Adjusts pH through excretion of hydrogen ions and reabsorption of bicarbonate.
- Blood Pressure Regulation: Via the renin-angiotensin-aldosterone system.
Common Disorders
- Urinary Tract Infection (UTI): Infection in the urinary system, often causing pain and urgency.
- Kidney Stones: Hard deposits of minerals and salts that form in the kidneys.
- Chronic Kidney Disease (CKD): Progressive loss of kidney function over time.
- Incontinence: Loss of bladder control, leading to involuntary urination.
Diagnostic Tests
- Urinalysis: Tests urine for substances and characteristics (pH, glucose, protein).
- Blood Tests: Measures creatinine and blood urea nitrogen (BUN) levels to assess kidney function.
- Imaging Studies: Ultrasound or CT scans to visualize the kidneys and urinary tract.
Key Terms
- Nephron: The functional unit of the kidney, responsible for urine formation.
- Oliguria: Abnormally low urine output.
- Anuria: Absence of urine production.
- Dysuria: Painful urination.
Overview of the Urinary System
- Produces, stores, and eliminates urine while maintaining fluid, electrolyte, and acid-base balance.
Major Components
-
Kidneys:
- Bean-shaped organs situated in the lower back.
- Function in blood filtration to produce urine.
- Control blood pressure through the renin-angiotensin system.
- Regulate sodium, potassium, and calcium levels, as well as acid-base balance through bicarbonate and hydrogen ion management.
-
Ureters:
- Two tubes serving as pathways from the kidneys to the bladder.
- Utilize peristaltic movements to transport urine.
-
Bladder:
- A muscular sac for urine storage.
- Contains stretch receptors that signal the urge to urinate.
- Holds about 400-600 mL of urine.
-
Urethra:
- Tube carrying urine from the bladder to the external environment.
- Significantly longer in males (around 20 cm) compared to females (approximately 4 cm).
- Features sphincters that control urination.
Urine Formation Process
-
Filtration:
- Takes place in the glomeruli within the kidneys.
- Blood plasma is processed to eliminate waste and excess substances.
-
Reabsorption:
- Vital substances like water, glucose, and electrolytes are absorbed back into the bloodstream.
- Primarily executed in the renal tubules.
-
Secretion:
- Additional waste and surplus ions are directed into urine formation.
- Aids in regulating blood pH and maintaining electrolyte homeostasis.
Homeostatic Functions
- Fluid Balance: Regulates body water retention and excretion.
- Electrolyte Balance: Keeps optimal levels of essential ions such as sodium and potassium.
- Acid-Base Balance: Adjusts bodily pH through hydrogen ion excretion and bicarbonate reabsorption.
- Blood Pressure Regulation: Achieved via the renin-angiotensin-aldosterone system.
Common Disorders
- Urinary Tract Infection (UTI): Causes discomfort and urgency due to infection in the urinary system.
- Kidney Stones: Formed by mineral and salt deposits in the kidneys, leading to pain.
- Chronic Kidney Disease (CKD): Gradual decline in kidney function over time.
- Incontinence: Involuntary urination due to loss of bladder control.
Diagnostic Tests
- Urinalysis: Evaluates urine for various substances and characteristics like pH and presence of glucose or protein.
- Blood Tests: Measures creatinine and blood urea nitrogen (BUN) levels to gauge kidney function.
- Imaging Studies: Utilizes ultrasound or CT scans to visualize the anatomical structure of the kidneys and urinary tract.
Key Terms
- Nephron: Functional unit of the kidney involved in urine production.
- Oliguria: Unusually low urine output.
- Anuria: Complete lack of urine production.
- Dysuria: Experience of pain during urination.
Synapses and Neurotransmitters
- Acetylcholine (ACh) is released by somatic motor neurons to synapse with skeletal muscle fibers, leading to end-plate potential (EPSPs) and depolarization.
- Voltage-gated channels open adjacent to the end plate following depolarization.
Monoamines as Neurotransmitters
- Monoamines include epinephrine, norepinephrine, serotonin, and dopamine.
- Released by exocytosis from presynaptic vesicles and diffuse across the synaptic cleft to interact with specific postsynaptic receptors.
- Reuptake into presynaptic membrane or degradation by monoamine oxidase (MAO) occurs to inhibit their action.
Serotonin as a Neurotransmitter
- Derived from L-tryptophan, serotonin regulates mood, behavior, appetite, and cerebral circulation.
- Selective serotonin reuptake inhibitors (SSRIs) prolong serotonin action and are used to treat depression, anxiety, and migraines.
Dopamine as a Neurotransmitter
- Dopamine originates from neurons in the midbrain and is involved in two major pathways:
- The nigrostriatal system, responsible for skeletal muscle movement initiation; degeneration leads to Parkinson’s disease.
- The mesolimbic system, associated with behavior, reward, and the effects of addictive drugs.
Norepinephrine as a Neurotransmitter
- Functions in both the peripheral nervous system (smooth and cardiac muscles, glands) and central nervous system, influencing general behavior.
- Increases blood pressure through arterial constriction in PNS.
Amino Acids as Neurotransmitters
- Glutamic acid and aspartic acid serve as major excitatory neurotransmitters in the CNS.
- Glutamic acid is involved in memory storage through NMDA receptors.
- Glycine acts as an inhibitory neurotransmitter, inducing hyperpolarization by opening Cl- channels.
- GABA (gamma-aminobutyric acid) is the most prevalent brain neurotransmitter and facilitates inhibitory actions in motor functions.
Polypeptides as Neurotransmitters
- Cholecystokinin (CCK) promotes satiety and plays a role in pain sensation.
- Neurons can release either classic neurotransmitters or polypeptide neurotransmitters.
Synaptic Transmission
- Calcium ions (Ca2+) activate calmodulin, which in turn activates protein kinase, enabling synaptic vesicle fusion.
- Neurotransmitters released into the synaptic cleft bind to specific receptors, causing either excitatory (EPSP) or inhibitory (IPSP) postsynaptic potential.
- Neurotransmitter inactivation occurs to terminate the signaling process within synapses.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.