Podcast
Questions and Answers
Which structure is NOT directly involved in osteomyelitis?
Which structure is NOT directly involved in osteomyelitis?
Osteomyelitis classified as 'exogenous' originates from which source?
Osteomyelitis classified as 'exogenous' originates from which source?
Why are children aged 2-12 more susceptible to osteomyelitis?
Why are children aged 2-12 more susceptible to osteomyelitis?
Which condition commonly predisposes individuals to osteomyelitis due to foot injuries and sores?
Which condition commonly predisposes individuals to osteomyelitis due to foot injuries and sores?
Signup and view all the answers
Why are individuals with sickle cell anemia at higher risk of developing osteomyelitis?
Why are individuals with sickle cell anemia at higher risk of developing osteomyelitis?
Signup and view all the answers
What is the most frequent location of acute osteomyelitis in children?
What is the most frequent location of acute osteomyelitis in children?
Signup and view all the answers
Which age group is most likely to present osteomyelitis with a history of urinary tract infection or urological procedure?
Which age group is most likely to present osteomyelitis with a history of urinary tract infection or urological procedure?
Signup and view all the answers
What diagnostic finding is commonly associated with acute osteomyelitis?
What diagnostic finding is commonly associated with acute osteomyelitis?
Signup and view all the answers
Which imaging technique is considered the MOST sensitive for detecting osteomyelitis?
Which imaging technique is considered the MOST sensitive for detecting osteomyelitis?
Signup and view all the answers
In cases of suspected tuberculous osteomyelitis where initial tests are negative, what is the MOST appropriate next step in diagnosis?
In cases of suspected tuberculous osteomyelitis where initial tests are negative, what is the MOST appropriate next step in diagnosis?
Signup and view all the answers
What is the MOST common site affected by tuberculous osteomyelitis?
What is the MOST common site affected by tuberculous osteomyelitis?
Signup and view all the answers
What is a PRIMARY difference between tuberculous osteomyelitis and pyogenic osteomyelitis?
What is a PRIMARY difference between tuberculous osteomyelitis and pyogenic osteomyelitis?
Signup and view all the answers
What percentage of osteomyelitis cases yield positive results in blood cultures?
What percentage of osteomyelitis cases yield positive results in blood cultures?
Signup and view all the answers
Besides systemic antibiotics, what additional treatment is often required for chronic osteomyelitis?
Besides systemic antibiotics, what additional treatment is often required for chronic osteomyelitis?
Signup and view all the answers
What is the PRIMARY route of infection for tuberculous osteomyelitis?
What is the PRIMARY route of infection for tuberculous osteomyelitis?
Signup and view all the answers
Which measure is important in the PREVENTATIVE care of osteomyelitis?
Which measure is important in the PREVENTATIVE care of osteomyelitis?
Signup and view all the answers
Flashcards
Osteomyelitis
Osteomyelitis
An infection of bone involving periosteum, cortical bone, and medullary cavity.
Pyogenic bacteria
Pyogenic bacteria
Bacteria that cause pus-forming infections, key in osteomyelitis.
Acute osteomyelitis
Acute osteomyelitis
A sudden onset of bone infection with severe symptoms.
Chronic osteomyelitis
Chronic osteomyelitis
Signup and view all the flashcards
Hematogenous route
Hematogenous route
Signup and view all the flashcards
Exogenous route
Exogenous route
Signup and view all the flashcards
Common pathogens in infants
Common pathogens in infants
Signup and view all the flashcards
Diabetes and osteomyelitis
Diabetes and osteomyelitis
Signup and view all the flashcards
CBC (WBC count)
CBC (WBC count)
Signup and view all the flashcards
Blood culture
Blood culture
Signup and view all the flashcards
Magnetic resonance imaging (MRI)
Magnetic resonance imaging (MRI)
Signup and view all the flashcards
Acute osteomyelitis treatment
Acute osteomyelitis treatment
Signup and view all the flashcards
Chronic osteomyelitis symptoms
Chronic osteomyelitis symptoms
Signup and view all the flashcards
Tuberculous osteomyelitis
Tuberculous osteomyelitis
Signup and view all the flashcards
Routes of infection
Routes of infection
Signup and view all the flashcards
Prevention of osteomyelitis
Prevention of osteomyelitis
Signup and view all the flashcards
Study Notes
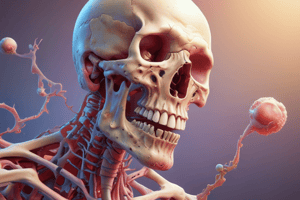
Bone Infections (Osteomyelitis)
- Suppurative bone infections, also known as osteomyelitis, are infections of the bone tissue.
- The periosteum, cortical bone, and medullary cavity (marrow cavity) can be involved.
- Common etiologic agents are pyogenic bacteria, and Mycobacterium tuberculosis.
Learning Outcomes
- Students will be able to define suppurative bone infections (osteomyelitis).
- Students will be able to describe common pathogens causing bone infections.
- Students will be able to list common pathogens causing bone infections in various age groups.
- Students will be able to describe laboratory methods used to diagnose osteomyelitis.
- Students will be able to explain the pathogenesis of osteomyelitis.
Classification of Osteomyelitis
- Based on duration and type of symptoms: acute or chronic
- Based on route of infection: hematogenous (via blood stream), exogenous (trauma or surgery), or direct spread
- Based on causative agent: specific (e.g., TB), or non-specific (most common, organisms other than TB)
Predisposing Factors
- Age: More common in children (2-12 years) and less common in adults, with possible increased occurrences in older adults.
- Sex: Boys are more susceptible than girls.
- Trauma: Injuries can introduce pathogens.
- Immunodeficiency: Conditions like AIDS.
- Diabetes Mellitus: Patients are susceptible to foot injuries and sores from chronic complications, which may become infected leading to osteomyelitis
- Renal dialysis & malnutrition: weaken the body’s ability to fight infection.
- Sickle Cell Anemia: Presence of septic foci (e.g., otitis media, tonsillitis, abscesses).
- Intravenous drug abusers: introducing pathogens through injection.
Organisms Commonly Isolated in Osteomyelitis Based on Age
- Infants (<1 year): Group B-β hemolytic streptococci, Staphylococcus aureus, Escherichia coli
- Children (1 to 16 years): Staphylococcus aureus, Streptococcus pyogenes, Haemophilus influenzae (50% in children <4 yrs), Kingella kingae.
- Adults (>16 years): Staphylococcus epidermidis, Staphylococcus aureus, Pseudomonas aeruginosa, Serratia marcescens, E. coli. (Staphylococcus aureus is responsible for 80-90% of cases)
Routes of Infection
- Hematogenous: Infection spreads through the bloodstream from another site (e.g., infected tooth, sinus). This is most common.
- Direct extension: Infection spreads directly from neighboring infected tissues (e.g., a tooth abscess).
- Direct inoculation: Infection introduced during surgical procedures or trauma
Sites of Osteomyelitis
- Occurs in the metaphysis of long bones (distal femur, proximal humerus, proximal tibia, distal radius) due to high vascularity.
- Other sites include vertebrae, clavicle, and ribs.
Pathogenesis of Acute Osteomyelitis (stages)
- Microorganisms enter the bone and are phagocytosed.
- Phagocytes release enzymes to lyse (break down) the bone.
- Pus spreads into vascular channels.
- Raising intraosseous pressure impairs blood flow in the bones. This causes chronic ischemic necrosis. As a result, large devascularized fragments are separated (sequestra).
- New bone formation, called involucrum, surrounds the area.
Acute Hematogenous Osteomyelitis
- Most common type in children under 12 years old.
- Often caused by a history of trauma.
- Males are more commonly affected.
- The metaphysis of rapidly growing long bones are most frequently involved.
Clinical Picture of Acute Osteomyelitis (Symptoms)
- Infant: History of septic focus, failure to thrive, drowsiness, irritability, metaphyseal tenderness, decreased range of movement (especially around the knee).
- Adult: History of UTI, immunosuppression, old age, diabetes, local pain, redness, tendernss, reluctance to move, fever, malaise, toxemia, leucocytosis, pus discharge.
Diagnosis
- Clinical: Based on patient's symptoms and physical examination.
- Laboratory: CBC (White Blood Cell count), ESR (Erythrocyte Sedimentation Rate), CRP (C-reactive protein), Blood culture (identifies pathogens), X-ray (initial evaluation), tissue samples (bone biopsy, smear), culture & sensitivity.
- Imaging: Bone scan, CT (computed tomography), MRI (magnetic resonance imaging) is highly sensitive.
Treatment of Osteomyelitis
- Acute: Prolonged antibiotic therapy (weeks or months). Surgical debridement may be required.
- Chronic: Systemic antibiotics and surgical treatment.
Tuberculosis of Bone (Tuberculous Osteomyelitis)
-
Affects children and young adults.
-
Insidious onset and chronic course.
-
More destructive than pyogenic osteomyelitis, and resistant to treatments.
-
Affects the spine (50% of cases), followed by the hips and knees.
-
Routes of Infection: hematogenous spread (from a focus of active pulmonary disease), direct extension (from caseous focus in lung to surrounding tissues.. or lymph nodes to vertebrae)
-
Symptoms: Fever, chills anorexia, Weight loss, local swelling
-
Treatment: The same anti-TB medications used for pulmonary TB.
Laboratory Findings in Tuberculous Osteomyelitis
- CBC: anemia, Leukocytosis.
- ESR, CRP increased.
- Blood culture.
- Tuberculin skin test.
- MRI spine
- If initial tests are negative but suspicion is high: nuclear medicine scan, CT guided bone biopsy, histological examination.
Prevention of Osteomyelitis
- Appropriate diagnosis and treatment of bacterial infections.
- Effective wound management.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on osteomyelitis, including its causes, at-risk populations, and diagnostic methods. This quiz covers essential information about the condition and its implications, especially in children and individuals with certain health issues.