Podcast
Questions and Answers
Which microscopic change is commonly observed in osteoarthritic joints?
Which microscopic change is commonly observed in osteoarthritic joints?
- Decreased bone density in the subchondral region
- Thickening of the synovial membrane
- Increased vascularization of the cartilage
- Focal loss of articular cartilage (correct)
What is a common risk factor for developing osteoarthritis?
What is a common risk factor for developing osteoarthritis?
- Infrequent joint use
- Obesity (correct)
- High levels of physical activity
- Female gender in adolescence
Which term best describes the diagnosis method for osteoarthritis?
Which term best describes the diagnosis method for osteoarthritis?
- Absolute diagnosis requiring laboratory tests
- Diagnosis based solely on imaging studies
- Clinical diagnosis based on symptoms and examination (correct)
- Diagnosis requiring biopsy of joint tissue
What principle is important in managing osteoarthritis?
What principle is important in managing osteoarthritis?
Which characteristic is associated with osteophyte formation in osteoarthritis?
Which characteristic is associated with osteophyte formation in osteoarthritis?
Which of the following is a significant risk factor associated with osteoarthritis?
Which of the following is a significant risk factor associated with osteoarthritis?
What does degeneration of articular cartilage in osteoarthritis primarily result in?
What does degeneration of articular cartilage in osteoarthritis primarily result in?
Which of the following is NOT a developmental abnormality related to osteoarthritis?
Which of the following is NOT a developmental abnormality related to osteoarthritis?
In osteoarthritis, which condition leads to abnormal proliferation of chondrocytes?
In osteoarthritis, which condition leads to abnormal proliferation of chondrocytes?
What is a common biomechanical factor contributing to osteoarthritis?
What is a common biomechanical factor contributing to osteoarthritis?
Which of the following hormones is commonly associated with risk factors for osteoarthritis?
Which of the following hormones is commonly associated with risk factors for osteoarthritis?
What are CPP and basic calcium phosphate crystals associated with in osteoarthritis?
What are CPP and basic calcium phosphate crystals associated with in osteoarthritis?
Which population is most likely to be exposed to repetitive loading, increasing their risk for osteoarthritis?
Which population is most likely to be exposed to repetitive loading, increasing their risk for osteoarthritis?
What is a likely contributing factor to osteoarthritis (OA) in individuals with developmental dysplasia of the hip?
What is a likely contributing factor to osteoarthritis (OA) in individuals with developmental dysplasia of the hip?
Which of the following factors is NOT associated with an increased risk of knee OA?
Which of the following factors is NOT associated with an increased risk of knee OA?
How does obesity contribute to the risk of OA, particularly in the hip and knee?
How does obesity contribute to the risk of OA, particularly in the hip and knee?
In which demographic is it speculated that squatting might increase the prevalence of knee OA?
In which demographic is it speculated that squatting might increase the prevalence of knee OA?
Which intervention appears to be associated with lower rates of OA in women?
Which intervention appears to be associated with lower rates of OA in women?
What abnormality in subchondral bone is associated with osteoarthritis?
What abnormality in subchondral bone is associated with osteoarthritis?
Which statement best describes the clinical features of osteoarthritis?
Which statement best describes the clinical features of osteoarthritis?
What is a characteristic symptom of osteoarthritis?
What is a characteristic symptom of osteoarthritis?
How does osteoarthritis affect the shape of the joint over time?
How does osteoarthritis affect the shape of the joint over time?
What process occurs at the joint margin in osteoarthritis?
What process occurs at the joint margin in osteoarthritis?
Flashcards
Epiphyseal Dysplasia
Epiphyseal Dysplasia
A group of disorders causing structural abnormalities in the growth plates of bones.
OA (Osteoarthritis) Risk Factors
OA (Osteoarthritis) Risk Factors
Several factors increase the likelihood of developing OA, including genetics, biomechanics, lifestyle, and injuries.
Slipped Femoral Epiphysis
Slipped Femoral Epiphysis
A condition where the head of the femur (thigh bone) slips out of place, increasing OA risk.
Paget's Disease of Bone
Paget's Disease of Bone
Signup and view all the flashcards
Biomechanical Factors (OA)
Biomechanical Factors (OA)
Signup and view all the flashcards
Obesity and OA
Obesity and OA
Signup and view all the flashcards
Estrogen and OA
Estrogen and OA
Signup and view all the flashcards
Squatting and OA
Squatting and OA
Signup and view all the flashcards
Cruciate Ligament Rupture
Cruciate Ligament Rupture
Signup and view all the flashcards
Meniscectomy
Meniscectomy
Signup and view all the flashcards
Osteoarthritis Risk Factors
Osteoarthritis Risk Factors
Signup and view all the flashcards
Genetic Factors (OA)
Genetic Factors (OA)
Signup and view all the flashcards
Repetitive Loading (OA)
Repetitive Loading (OA)
Signup and view all the flashcards
Adverse Biomechanics (OA)
Adverse Biomechanics (OA)
Signup and view all the flashcards
Obesity (OA)
Obesity (OA)
Signup and view all the flashcards
Trauma (OA)
Trauma (OA)
Signup and view all the flashcards
Hormonal Factors (OA)
Hormonal Factors (OA)
Signup and view all the flashcards
Cartilage Degradation (OA)
Cartilage Degradation (OA)
Signup and view all the flashcards
Chondrocyte Activity (OA)
Chondrocyte Activity (OA)
Signup and view all the flashcards
Osteoarthritis (OA)
Osteoarthritis (OA)
Signup and view all the flashcards
Osteophytes
Osteophytes
Signup and view all the flashcards
Subchondral sclerosis
Subchondral sclerosis
Signup and view all the flashcards
Subchondral cyst
Subchondral cyst
Signup and view all the flashcards
Fibrocartilage
Fibrocartilage
Signup and view all the flashcards
Endochondral ossification
Endochondral ossification
Signup and view all the flashcards
Joint enlargement in OA
Joint enlargement in OA
Signup and view all the flashcards
Common OA locations
Common OA locations
Signup and view all the flashcards
OA symptoms
OA symptoms
Signup and view all the flashcards
Osteoarthritis
Osteoarthritis
Signup and view all the flashcards
Pathophysiology of OA
Pathophysiology of OA
Signup and view all the flashcards
Risk factors for OA
Risk factors for OA
Signup and view all the flashcards
Microscopic changes in OA
Microscopic changes in OA
Signup and view all the flashcards
Clinical presentation of OA
Clinical presentation of OA
Signup and view all the flashcards
Joint distribution of OA
Joint distribution of OA
Signup and view all the flashcards
Clinical examination findings
Clinical examination findings
Signup and view all the flashcards
Clinical diagnosis
Clinical diagnosis
Signup and view all the flashcards
Differential diagnoses
Differential diagnoses
Signup and view all the flashcards
Disability in OA
Disability in OA
Signup and view all the flashcards
Biopsychosocial model
Biopsychosocial model
Signup and view all the flashcards
Diagnostic investigations
Diagnostic investigations
Signup and view all the flashcards
OA management principles
OA management principles
Signup and view all the flashcards
OA analgesics
OA analgesics
Signup and view all the flashcards
Joint replacement
Joint replacement
Signup and view all the flashcards
Study Notes
Osteoarthritis Learning Outcomes
- Osteoarthritis is the most common form of arthritis
- Understand the pathophysiology of Osteoarthritis
- List risk factors for osteoarthritis
- Describe common microscopic changes in osteoarthritic joints
- Recognise common features in the presentation of osteoarthritis
- Describe joint distribution of osteoarthritis
- Outline findings of osteoarthritis on clinical examination
- Understand the term 'clinical diagnosis'
- List common differential diagnoses for presentations of osteoarthritis
- Understand terms related to disability
- Describe components of a biopsychosocial model in healthcare
- Describe the role of investigations in the diagnosis of osteoarthritis
- Outline principles of management of osteoarthritis
- Describe common analgesics and their mechanism of action in the treatment of osteoarthritis
- Outline the principles of joint replacement
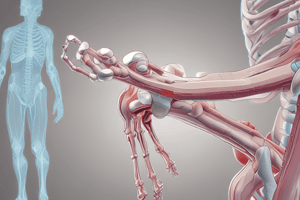
Pathophysiology of Osteoarthritis
- Characterized by focal loss of articular cartilage, subchondral sclerosis, osteophyte formation at the joint margin, and remodeling of the joint contour.
- Can be asymptomatic in some cases
- Inheritance is polygenic, mediated by several genetic variants
- Component of multiple epiphyseal dysplasias caused by single gene mutations affecting cartilage matrix
- Structural abnormalities (e.g., slipped femoral epiphysis) increase OA risk due to abnormal load distribution
- Biomechanical factors (e.g., occupations requiring repetitive squatting, injury to the cruciate ligament, meniscectomy operations), obesity increase risk of OA
- Estrogen is important; lower rates in women using hormone replacement therapy (HRT)
- Cytokines from adipose tissue may play a role in OA
Genetics
- Skeletal dysplasias
- Polygenic inheritance
- Developmental dysplasia of the hip
- Slipped femoral epiphysis
- Repetitive loading
- Farmers, miners, elite athletes, adverse biomechanics, meniscectomy, ligament rupture, Paget's disease, obesity, trauma, estrogen deficiency, aromatase inhibitors
Degeneration of Articular Cartilage
- Chondrocytes are terminally differentiated cells in normal cartilage
- In OA, chondrocytes divide and produce more cartilage matrix but also accelerate degradation of major structural components (aggrecan and type II collagen)
- Increased concentration of aggrecan in cartilage matrix leads to cartilage vulnerability to load-bearing injury
- Initial focal damage (maximum load-bearing part of joint) then progresses to larger cartilage surface areas
- CPP and basic calcium phosphate crystals deposit in abnormal cartilage.
- Fibrocartilage is produced at joint margin and forms osteophytes via endochondral ossification
- Bone remodeling and cartilage thinning alters shape of the joint, increasing its surface area.
Clinical Features of Osteoarthritis
- Characteristic distribution: hips, knees, PIP and DIP joints
- Main Presenting symptoms: pain and functional restriction
- Pain may relate to increased pressure in subchondral bone, microfractures, capsular distension, and low-grade synovitis
- Symptoms and signs of osteoarthritis (pain, insidious onset, variable or intermittent nature) can be relieved by rest.
- Mild morning stiffness (<15 minutes), inactivity gelling (<5 minutes)
- Usually only one or a few joints affected
- Clinical signs: restricted movement, palpable/audible crepitus, bony swelling around margins, deformity, and joint line/periarticular tenderness.
- Generalised nodal OA: Affected joints enlarged due to osteophyte formation with characteristic lateral deviation
- Involvement of the first CMC joint causing pain and functional impairment (e.g., opening bottles).
- Polyarticular finger interphalangeal joint OA, Heberden's/Bouchard's nodes, marked female preponderance, peak onset in middle age.
- Good functional outcome for hands, predispositions to other joints, genetic predisposition.
- OA typically targets the patello-femoral and medial tibio-femoral compartments, but eventually spreads to the whole of the joint.
- Most patients have bilateral and symmetrical involvement.
- In men, trauma is a more important risk factor and may result in unilateral OA.
Knee Specific OA features
- Pain usually localized to anterior or medial aspect of the knee/upper tibia
- Patello-femoral pain is worse during stairs/inclines
- Posterior knee pain suggests a popliteal cyst
- Prolonged walking, rising from a chair, getting in/out of car difficult; bending to put on shoes and socks
- Local examination findings may include jerky/asymmetric gait, varus/valgus deformity, fixed flexion deformities, joint-line tenderness Weakness and wasting of the quadriceps muscles
Hip Specific OA Features
- Pain usually maximal deep in the anterior groin, radiating to buttock, anterolateral thigh, knee or shin.
- Often bilateral at presentation, may be associated with generalized nodal OA
- Better prognosis than superior hip OA; progression to axial migration of femoral head is uncommon
Investigations
- X-rays of affected joints are used to assess severity of structural changes
- X-rays can help with prognosis in patients with severe symptoms
- MRI scan may be used if diagnosis is uncertain
- Routine biochemistry, haematology checks, and autoantibody tests are generally normal, though mild acute phase response is possible.
- Synovial fluid aspirated from an affected joint is viscous with a low cell count.
Management
- Pain and disability is a primary cause in older adults; Calcium phosphate deposition, and falls are risk factors. OA is associated with lower limb osteoarthritis, making it more likely that people will fall.
- Muscle-strengthening exercises improve balance and reduce falls risk
- Oral paracetamol and topical non-steroidal anti-inflammatory drugs (NSAIDs) are generally safe for older people
- Intra-articular glucocorticoid injections may be useful for patients experiencing special events
- Total joint replacement surgery is a cost-effective treatment for severe, disabling OA of the hip/knee (no age limit)
- Lifestyle advice: weight loss, strengthening and aerobic exercises. Quadriceps strengthening useful for knee OA.
- Shock-absorbing footwear, pacing activities, use of walking stick, built-up shoes (for hip/knee OA)
- Non-pharmacological therapies: acupuncture, TENS, heat or cold
- Pharmacological therapies (paracetamol, topical NSAIDs, capsaicin, strong opiates, antineuropathic drugs, intra-articular glucocorticoid/hyaluronic acid injections), if symptoms don't resolve.
Summary of Osteoarthritis
- Common condition with a variable presentation
- Symptoms don't always correlate with the degree of pathological changes
- Diagnosis primarily based on clinical presentation, often supplemented with X-ray imaging
- Treatment requires holistic patient support (education, lifestyle, support, analgesia)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.