Podcast
Questions and Answers
What is a common cause of strep pharyngitis?
What is a common cause of strep pharyngitis?
- Staphylococcus aureus
- Haemophilus influenzae
- Streptococcus pyogenes (correct)
- Streptococcus pneumoniae
Which symptom is NOT associated with infectious mononucleosis caused by EBV?
Which symptom is NOT associated with infectious mononucleosis caused by EBV?
- Severe fatigue
- Raspberry tongue (correct)
- Lymphadenopathy
- Fever
Which condition is characterized by inflammatory processes affecting the supporting structures of the teeth?
Which condition is characterized by inflammatory processes affecting the supporting structures of the teeth?
- Pyogenic granuloma
- Periodontitis (correct)
- Gingivitis
- Irritation fibroma
What is a common presentation of rheumatic fever?
What is a common presentation of rheumatic fever?
What triggers the formation of irritation fibromas in the oral cavity?
What triggers the formation of irritation fibromas in the oral cavity?
Which feature describes a pyogenic granuloma?
Which feature describes a pyogenic granuloma?
Which condition is characterized by a 'fiery red tongue' with prominent papillae?
Which condition is characterized by a 'fiery red tongue' with prominent papillae?
What describes the main cause of periodontitis?
What describes the main cause of periodontitis?
Which characteristic is NOT associated with aphthous ulcers?
Which characteristic is NOT associated with aphthous ulcers?
What distinguishes a mucocele from aphthous ulcers?
What distinguishes a mucocele from aphthous ulcers?
Which pathogen is most commonly associated with pseudomembranous thrush in the oral cavity?
Which pathogen is most commonly associated with pseudomembranous thrush in the oral cavity?
Which symptom is characteristic of Herpes Simplex Virus (HSV) infections?
Which symptom is characteristic of Herpes Simplex Virus (HSV) infections?
Which of the following factors can lead to the manifestation of symptoms differently with various oral pathogens?
Which of the following factors can lead to the manifestation of symptoms differently with various oral pathogens?
What is a common presentation for a mucocele?
What is a common presentation for a mucocele?
Which statement accurately describes aphthous ulcers?
Which statement accurately describes aphthous ulcers?
What prompts the size change of a mucocele around meals?
What prompts the size change of a mucocele around meals?
What is a notable characteristic of Peripheral Ossifying Fibroma?
What is a notable characteristic of Peripheral Ossifying Fibroma?
Which of the following is a clinical manifestation of Behcet's Disease?
Which of the following is a clinical manifestation of Behcet's Disease?
What is the primary cause of Hairy Leukoplakia?
What is the primary cause of Hairy Leukoplakia?
Which symptom is NOT typically associated with Behcet's Disease?
Which symptom is NOT typically associated with Behcet's Disease?
What best describes the presentation of Hairy Leukoplakia?
What best describes the presentation of Hairy Leukoplakia?
What is the primary pathological process leading to the formation of a cholesteatoma?
What is the primary pathological process leading to the formation of a cholesteatoma?
What type of lesions are associated with Peripheral Ossifying Fibroma?
What type of lesions are associated with Peripheral Ossifying Fibroma?
What long-term effect is associated with Hairy Leukoplakia?
What long-term effect is associated with Hairy Leukoplakia?
What is the primary distinguishing feature of closed-angle glaucoma compared to open-angle glaucoma?
What is the primary distinguishing feature of closed-angle glaucoma compared to open-angle glaucoma?
Which of the following is NOT a risk factor for developing closed-angle glaucoma?
Which of the following is NOT a risk factor for developing closed-angle glaucoma?
What symptom is commonly associated with closed-angle glaucoma?
What symptom is commonly associated with closed-angle glaucoma?
Which of the following factors contributes to the development of cataracts?
Which of the following factors contributes to the development of cataracts?
Which clinical manifestation is commonly seen in patients with cataracts?
Which clinical manifestation is commonly seen in patients with cataracts?
What is the primary cause of open-angle glaucoma?
What is the primary cause of open-angle glaucoma?
Which symptom is NOT associated with acute otitis media?
Which symptom is NOT associated with acute otitis media?
In which condition can bone reabsorption, followed by fibrosis, lead to significant hearing loss?
In which condition can bone reabsorption, followed by fibrosis, lead to significant hearing loss?
Which pathogen is particularly aggressive in causing necrotizing otitis media in diabetic patients?
Which pathogen is particularly aggressive in causing necrotizing otitis media in diabetic patients?
Which of the following is a risk factor for open-angle glaucoma?
Which of the following is a risk factor for open-angle glaucoma?
What ocular symptom is typically associated with advanced open-angle glaucoma?
What ocular symptom is typically associated with advanced open-angle glaucoma?
Which clinical manifestation is common in anterior blepharitis?
Which clinical manifestation is common in anterior blepharitis?
Which of the following is NOT a symptom of chronic otitis media?
Which of the following is NOT a symptom of chronic otitis media?
Which of the following is NOT a common cause of retinal detachment?
Which of the following is NOT a common cause of retinal detachment?
What symptom is associated specifically with retinal detachment?
What symptom is associated specifically with retinal detachment?
Which factor is linked to an increased risk of macular degeneration?
Which factor is linked to an increased risk of macular degeneration?
What can cause light sensitivity, especially at night?
What can cause light sensitivity, especially at night?
Seeing double images can be a symptom of which condition?
Seeing double images can be a symptom of which condition?
What is a common symptom of anterior blepharitis?
What is a common symptom of anterior blepharitis?
What causes a chalazion to develop?
What causes a chalazion to develop?
Which of the following is NOT typically associated with blepharitis?
Which of the following is NOT typically associated with blepharitis?
What is the recommended treatment for acute cases of anterior blepharitis?
What is the recommended treatment for acute cases of anterior blepharitis?
Which type of chalazion is caused by inflammation of the Zeiss gland?
Which type of chalazion is caused by inflammation of the Zeiss gland?
What is the most common first sign of retinoblastoma?
What is the most common first sign of retinoblastoma?
Which symptom is most likely to occur in the late stage of retinal detachment?
Which symptom is most likely to occur in the late stage of retinal detachment?
In the context of proliferative diabetic retinopathy, what happens in later stages when blood vessels bleed into the vitreous?
In the context of proliferative diabetic retinopathy, what happens in later stages when blood vessels bleed into the vitreous?
Which of the following is characteristic of intermediate stage retinal detachment?
Which of the following is characteristic of intermediate stage retinal detachment?
What is a potential symptom of retinoblastoma that involves the physical appearance of the eye?
What is a potential symptom of retinoblastoma that involves the physical appearance of the eye?
What is a characteristic feature of a pinguecula?
What is a characteristic feature of a pinguecula?
Which factor increases the risk of developing pterygium?
Which factor increases the risk of developing pterygium?
What role does atherosclerosis play in retinal arteriolosclerosis?
What role does atherosclerosis play in retinal arteriolosclerosis?
Which statement accurately describes a pterygium?
Which statement accurately describes a pterygium?
What is the primary cause for retinal artery blockages?
What is the primary cause for retinal artery blockages?
What type of immune reaction is primarily involved in allergic rhinitis?
What type of immune reaction is primarily involved in allergic rhinitis?
Which cells are responsible for the immediate hypersensitivity response?
Which cells are responsible for the immediate hypersensitivity response?
What is the role of IL-4 in the immune response to allergens?
What is the role of IL-4 in the immune response to allergens?
Which component is NOT involved in the late-phase reaction of allergic rhinitis?
Which component is NOT involved in the late-phase reaction of allergic rhinitis?
What triggers the degranulation of mast cells during an allergic reaction?
What triggers the degranulation of mast cells during an allergic reaction?
In the context of allergic reactions, what do excessive Th2 cells stimulate?
In the context of allergic reactions, what do excessive Th2 cells stimulate?
Which cytokine is primarily responsible for activating eosinophils during allergic reactions?
Which cytokine is primarily responsible for activating eosinophils during allergic reactions?
What time frame defines the late-phase allergic reaction in allergic rhinitis?
What time frame defines the late-phase allergic reaction in allergic rhinitis?
Flashcards are hidden until you start studying
Study Notes
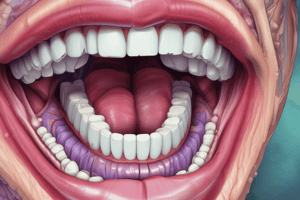
Oral Pathologies
-
Aphthous Ulcers
- Clustered, recurrent oral lesions associated with immunologic disorders like celiac disease and IBS.
- Appear as shallow ulcerations with a red halo, painful, affecting up to 40% of the population, often resolving in 7-10 days.
-
Mucocele
- Common salivary gland lesion caused by saliva leakage due to trauma, often located on the lower lip.
- Fluid-filled, blue translucent swelling that changes size, particularly around meals.
Oral Infections
-
Candida albicans
- Causes "Thrush," presenting as a gray-white membrane easily scraped off, revealing an inflammatory base.
- Promoted by antibiotic usage that reduces beneficial oral bacteria.
-
Strep Pharyngitis
- Caused primarily by Streptococcus pyogenes, associated with symptoms of fiery red tongue and can lead to rheumatic fever.
Oral Manifestations of Systemic Diseases
- Initial infection symptoms in children manifest with oral vesicles, fever, and lymphadenopathy.
- Adults may experience recurrent acute herpes pharyngitis.
Periodontal Diseases
-
Gingivitis
- Inflammatory response due to plaque buildup, leading to redness, bleeding, and contour changes.
-
Periodontitis
- Affects supporting structures of teeth and can lead to serious conditions like endocarditis and abscesses.
-
Irritation Fibroma
- Traumatic fibroma due to repetitive trauma, presenting as a hard mass, primarily in the buccal mucosa.
-
Pyogenic Granuloma
- Highly vascular growth, often seen in children and pregnant women.
Oral Lesions
-
Factors like hypertrophy and neoplasia contribute to oral lesions' development, often presenting as red, ulcerated nodular lesions.
-
Peripheral Ossifying Fibroma
- Reactive lesion observed mainly in young females, recurring in 15-20% of cases.
Behcet's Disease
- A rare autoimmune disorder presenting with recurrent mouth sores, eye inflammation, and vascular complications.
Hairy Leukoplakia
- An EBV-associated oral lesion primarily in immunocompromised individuals, presenting as white, "hairy" patches on the tongue.
Ear Conditions
-
Cholesteatoma
- Non-neoplastic cystic lesions resulting from chronic otitis media.
-
Otosclerosis
- Progressive condition causing hearing loss, linked to age and familial history.
-
Otitis Media
- Caused by pathogens like Pseudomonas aeruginosa in diabetic patients, presenting with acute or chronic symptoms.
Blepharitis
- Inflammation of eyelid margins, with anterior blepharitis linked to staphylococcal infections and seborrheic conditions.
Ophthalmology
-
Glaucoma Types
- Open-Angle: Chronic optic neuropathy with peripheral vision loss; common causes include age and family history.
- Closed-Angle: Rare, acute increase in eye pressure distinguished by blocked aqueous outflow, risk factors include older age and certain medical conditions.
-
Cataracts
- Clouding of the lens leading to blurred vision; risk factors include aging, genetics, and certain medications.
Retinal Detachment and Macular Degeneration
-
Causes of Detachment
- More prevalent in older populations, associated with eye injuries and diabetic retinopathy.
-
Signs and Symptoms
- Flashes of light, floaters, and blurred vision are indicative of retinal detachment.
Retinoblastoma
- Malignant eye tumor in young children, often presenting with leukocoria and related symptoms like eye pain and vision problems.
Proliferative Diabetic Retinopathy
- Advanced form characterized by abnormal blood vessels leading to potential vision loss; early stages typically asymptomatic.
Anterior Blepharitis and Chalazion
- Anterior blepharitis can be associated with skin bacteria; treatment often requires topical antibiotics.
- Chalazion is a non-tender, slow-growing lump caused by blocked oil glands in the eyelid.
Pterygium and Pinguecula
- Pinguecula is a benign growth that can lead to pterygium, which grows onto the cornea and can obstruct vision, common in sun-exposed individuals.
Retinal Arteriosclerosis
- Blocked retinal arteries can lead to vision problems and are influenced by atherosclerosis and systemic conditions.
Respiratory and Immune Responses
-
Allergic Rhinitis
- IgE-mediated hypersensitivity to various allergens leading to symptoms like mucosal edema and eosinophilic infiltration.
-
Type 1 Hypersensitivity
- Immediate reaction caused by antigen binding to IgE on mast cells, resulting in symptoms such as vasodilation and vascular leakage.
-
Mast Cell Activation
- Critical for immediate hypersensitivity responses, triggered by cross-linking of IgE antibodies with antigens.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.