Podcast
Questions and Answers
Which membrane directly encloses the heart muscle itself?
Which membrane directly encloses the heart muscle itself?
- Pleural membrane
- Fibrous pericardium
- Visceral pericardium (epicardium) (correct)
- Parietal pericardium
What is the function of the serous fluid located between the parietal and visceral layers of the pericardium?
What is the function of the serous fluid located between the parietal and visceral layers of the pericardium?
- To provide nutrients to the myocardium
- To facilitate electrical impulse transmission
- To cushion the heart against external impacts
- To prevent friction as the heart beats (correct)
The smooth epithelial tissue lining the heart chambers and blood vessels, preventing abnormal blood clotting, is known as:
The smooth epithelial tissue lining the heart chambers and blood vessels, preventing abnormal blood clotting, is known as:
- Myocardium
- Pericardium
- Endocardium (correct)
- Epicardium
Which heart chamber receives deoxygenated blood from the superior and inferior vena cava and the coronary sinus?
Which heart chamber receives deoxygenated blood from the superior and inferior vena cava and the coronary sinus?
What is the function of the tricuspid valve?
What is the function of the tricuspid valve?
Which valve prevents backflow of blood from the pulmonary artery into the right ventricle?
Which valve prevents backflow of blood from the pulmonary artery into the right ventricle?
Oxygenated blood from the lungs enters which chamber of the heart?
Oxygenated blood from the lungs enters which chamber of the heart?
The mitral valve, also known as the bicuspid valve, prevents backflow of blood into the:
The mitral valve, also known as the bicuspid valve, prevents backflow of blood into the:
Which heart valve controls the flow of oxygenated blood from the left ventricle to the systemic circulation?
Which heart valve controls the flow of oxygenated blood from the left ventricle to the systemic circulation?
Compared to the right ventricle, the left ventricle has:
Compared to the right ventricle, the left ventricle has:
What is the primary pacemaker of the heart?
What is the primary pacemaker of the heart?
If the SA node fails, which of the following can take over as a secondary pacemaker, albeit at a slower rate?
If the SA node fails, which of the following can take over as a secondary pacemaker, albeit at a slower rate?
During the cardiac cycle, the 'lub' sound is caused by:
During the cardiac cycle, the 'lub' sound is caused by:
The 'dub' heart sound is created by:
The 'dub' heart sound is created by:
Cardiac output is calculated by multiplying:
Cardiac output is calculated by multiplying:
According to Starling's law of the heart, increased venous return leads to:
According to Starling's law of the heart, increased venous return leads to:
Epinephrine affects the heart by:
Epinephrine affects the heart by:
Atrial natriuretic peptide (ANP) is released in response to:
Atrial natriuretic peptide (ANP) is released in response to:
The middle layer of arteries, composed of smooth muscle and elastic tissue, primarily contributes to:
The middle layer of arteries, composed of smooth muscle and elastic tissue, primarily contributes to:
Valves in veins are most numerous in the veins of:
Valves in veins are most numerous in the veins of:
Precapillary sphincters regulate blood flow into:
Precapillary sphincters regulate blood flow into:
Exchange of gases, nutrients, and wastes between blood and tissues primarily occurs in:
Exchange of gases, nutrients, and wastes between blood and tissues primarily occurs in:
Edema, or tissue swelling, can result from:
Edema, or tissue swelling, can result from:
Peripheral resistance, which helps maintain blood pressure, is primarily regulated by the:
Peripheral resistance, which helps maintain blood pressure, is primarily regulated by the:
Which of the following factors does NOT directly contribute to venous return?
Which of the following factors does NOT directly contribute to venous return?
The renin-angiotensin-aldosterone mechanism is initiated by:
The renin-angiotensin-aldosterone mechanism is initiated by:
Antidiuretic hormone (ADH) affects blood pressure by:
Antidiuretic hormone (ADH) affects blood pressure by:
Pulmonary circulation is characterized by:
Pulmonary circulation is characterized by:
The hepatic portal circulation allows the liver to:
The hepatic portal circulation allows the liver to:
Atherosclerosis is characterized by:
Atherosclerosis is characterized by:
Which of the following is NOT a typical age-related change in the cardiovascular system?
Which of the following is NOT a typical age-related change in the cardiovascular system?
In older adults, a myocardial infarction (MI) may present atypically, with which symptom being the sole indicator?
In older adults, a myocardial infarction (MI) may present atypically, with which symptom being the sole indicator?
Orthostatic hypotension is defined as a drop in systolic blood pressure greater than:
Orthostatic hypotension is defined as a drop in systolic blood pressure greater than:
A pulse deficit, the difference between apical and radial pulse rates, indicates:
A pulse deficit, the difference between apical and radial pulse rates, indicates:
A 'thrill' palpated over an artery signifies:
A 'thrill' palpated over an artery signifies:
A 'bruit' auscultated over an artery is caused by:
A 'bruit' auscultated over an artery is caused by:
Clubbing of the nailbeds is a sign of:
Clubbing of the nailbeds is a sign of:
Dependent rubor, redness in the lower extremities when dependent, suggests:
Dependent rubor, redness in the lower extremities when dependent, suggests:
Pitting edema is assessed by:
Pitting edema is assessed by:
An S3 heart sound in older adults is often associated with:
An S3 heart sound in older adults is often associated with:
A pericardial friction rub is caused by:
A pericardial friction rub is caused by:
The fibrous pericardium, parietal pericardium, and visceral pericardium (epicardium) enclose the heart. What is the arrangement of these membranes from outermost to innermost?
The fibrous pericardium, parietal pericardium, and visceral pericardium (epicardium) enclose the heart. What is the arrangement of these membranes from outermost to innermost?
Why is the endocardium's smooth epithelial tissue important for cardiovascular function?
Why is the endocardium's smooth epithelial tissue important for cardiovascular function?
Deoxygenated blood from the myocardium is returned to the right atrium via what vessel?
Deoxygenated blood from the myocardium is returned to the right atrium via what vessel?
Which structural feature prevents the hyperextension of the atrioventricular (AV) valves during ventricular systole?
Which structural feature prevents the hyperextension of the atrioventricular (AV) valves during ventricular systole?
What is the functional significance of the thicker myocardium found in the left ventricle compared to the right ventricle?
What is the functional significance of the thicker myocardium found in the left ventricle compared to the right ventricle?
If the sinoatrial (SA) node is damaged and nonfunctional, what heart rate would you expect if the atrioventricular (AV) node takes over as the heart's pacemaker?
If the sinoatrial (SA) node is damaged and nonfunctional, what heart rate would you expect if the atrioventricular (AV) node takes over as the heart's pacemaker?
What phase of the cardiac cycle corresponds to the contraction and emptying of the atria and ventricles?
What phase of the cardiac cycle corresponds to the contraction and emptying of the atria and ventricles?
How does an increased venous return affect the stroke volume, according to Starling's law of the heart?
How does an increased venous return affect the stroke volume, according to Starling's law of the heart?
How does epinephrine affect cardiac output and blood pressure?
How does epinephrine affect cardiac output and blood pressure?
What is the impact of atrial natriuretic peptide (ANP) on blood volume and blood pressure?
What is the impact of atrial natriuretic peptide (ANP) on blood volume and blood pressure?
How does the sympathetic division of the autonomic nervous system primarily regulate arterial diameter and blood pressure?
How does the sympathetic division of the autonomic nervous system primarily regulate arterial diameter and blood pressure?
Why are valves more numerous in the veins of the extremities, especially the legs?
Why are valves more numerous in the veins of the extremities, especially the legs?
How do precapillary sphincters regulate blood flow within capillary networks?
How do precapillary sphincters regulate blood flow within capillary networks?
What is the relationship between increased blood pressure within capillaries and edema?
What is the relationship between increased blood pressure within capillaries and edema?
How does the renin-angiotensin-aldosterone mechanism respond to decreased blood flow through the kidneys, and what is its overall effect?
How does the renin-angiotensin-aldosterone mechanism respond to decreased blood flow through the kidneys, and what is its overall effect?
How does antidiuretic hormone (ADH) raise blood pressure?
How does antidiuretic hormone (ADH) raise blood pressure?
What prevents filtration in the capillaries in pulmonary circulation?
What prevents filtration in the capillaries in pulmonary circulation?
In the hepatic portal circulation, why does blood from the digestive organs and spleen pass through the liver before returning to the heart?
In the hepatic portal circulation, why does blood from the digestive organs and spleen pass through the liver before returning to the heart?
How does atherosclerosis affect blood flow to organs and tissues, and what potential complication can arise from it?
How does atherosclerosis affect blood flow to organs and tissues, and what potential complication can arise from it?
What are the expected effects of aging on maximum cardiac output and heart rate?
What are the expected effects of aging on maximum cardiac output and heart rate?
What is the significance of chest pain radiating to the shoulders, neck, jaw, arms, or back in the context of cardiovascular assessment?
What is the significance of chest pain radiating to the shoulders, neck, jaw, arms, or back in the context of cardiovascular assessment?
In cardiovascular assessment, what might intermittent claudication suggest, and what typically provokes this symptom?
In cardiovascular assessment, what might intermittent claudication suggest, and what typically provokes this symptom?
What could palpitations or irregular heartbeats indicate in a cardiovascular assessment?
What could palpitations or irregular heartbeats indicate in a cardiovascular assessment?
In a patient with cardiovascular issues, what could edema in the lower extremities indicate?
In a patient with cardiovascular issues, what could edema in the lower extremities indicate?
What might crackles or wheezes in the breath sounds indicate in a patient with suspected cardiovascular issues?
What might crackles or wheezes in the breath sounds indicate in a patient with suspected cardiovascular issues?
What underlying condition should be suspected in light-skinned individuals presenting with cyanosis?
What underlying condition should be suspected in light-skinned individuals presenting with cyanosis?
What is the likely cause of a cool temperature in an extremity during a cardiovascular assessment?
What is the likely cause of a cool temperature in an extremity during a cardiovascular assessment?
What does an increased capillary refill time exceeding 3 seconds typically suggest?
What does an increased capillary refill time exceeding 3 seconds typically suggest?
In assessing jugular venous distention, at what angle should the patient be positioned?
In assessing jugular venous distention, at what angle should the patient be positioned?
During palpation of arterial pulses, what does a 'thready' pulse indicate?
During palpation of arterial pulses, what does a 'thready' pulse indicate?
When is the third heart sound (S3) considered a normal finding?
When is the third heart sound (S3) considered a normal finding?
What cardiac condition could be indicated by the presence of an S4 heart sound?
What cardiac condition could be indicated by the presence of an S4 heart sound?
Where is Erb's point located, and why is it significant in cardiac auscultation?
Where is Erb's point located, and why is it significant in cardiac auscultation?
What findings would indicate the need to report a pulse deficit to the health care provider?
What findings would indicate the need to report a pulse deficit to the health care provider?
If a patient has acute heart failure, what is an expected characteristic of their sputum?
If a patient has acute heart failure, what is an expected characteristic of their sputum?
During the collection of subjective data, which of the following childhood diseases can lead to heart disease?
During the collection of subjective data, which of the following childhood diseases can lead to heart disease?
Which of the following lifestyle factors is NOT a modifiable risk factor for cardiovascular disease?
Which of the following lifestyle factors is NOT a modifiable risk factor for cardiovascular disease?
Which of the following best describes the purpose of the serous fluid located within the pericardial sac?
Which of the following best describes the purpose of the serous fluid located within the pericardial sac?
The walls of arteries are composed of 3 layers of tissue. Which layer is primarily responsible for the vasoconstriction and vasodilation?
The walls of arteries are composed of 3 layers of tissue. Which layer is primarily responsible for the vasoconstriction and vasodilation?
Why are valves more prevalent in veins of the lower extremities compared to veins in other parts of the body?
Why are valves more prevalent in veins of the lower extremities compared to veins in other parts of the body?
What is the physiological consequence of increased blood pressure within capillaries, exceeding the capacity of lymph vessels to collect excess fluid?
What is the physiological consequence of increased blood pressure within capillaries, exceeding the capacity of lymph vessels to collect excess fluid?
Which mechanism is triggered when blood flow to the kidneys decreases, and what is its primary outcome?
Which mechanism is triggered when blood flow to the kidneys decreases, and what is its primary outcome?
How does antidiuretic hormone (ADH) contribute to the regulation of blood pressure?
How does antidiuretic hormone (ADH) contribute to the regulation of blood pressure?
What characteristic of pulmonary capillaries prevents fluid accumulation in the alveoli of the lungs?
What characteristic of pulmonary capillaries prevents fluid accumulation in the alveoli of the lungs?
Why is it important for blood from the digestive organs and spleen to pass through the liver via the hepatic portal circulation before returning to the heart?
Why is it important for blood from the digestive organs and spleen to pass through the liver via the hepatic portal circulation before returning to the heart?
How does atherosclerosis reduce blood flow to organs and tissues, and what is a potential complication?
How does atherosclerosis reduce blood flow to organs and tissues, and what is a potential complication?
What are the anticipated effects of aging on maximum cardiac output and heart rate?
What are the anticipated effects of aging on maximum cardiac output and heart rate?
What might chest pain radiating to the shoulders, neck, jaw, arms, or back suggest during a cardiovascular assessment?
What might chest pain radiating to the shoulders, neck, jaw, arms, or back suggest during a cardiovascular assessment?
What does intermittent claudication suggest, and what typically provokes it?
What does intermittent claudication suggest, and what typically provokes it?
What physiological processes might palpitations or irregular heartbeats indicate during a cardiovascular assessment?
What physiological processes might palpitations or irregular heartbeats indicate during a cardiovascular assessment?
What lung sounds might indicate a cardiac cause?
What lung sounds might indicate a cardiac cause?
What does a cool temperature in an extremity during a cardiovascular assessment typically indicate?
What does a cool temperature in an extremity during a cardiovascular assessment typically indicate?
Flashcards
Cardiovascular System Function
Cardiovascular System Function
The cardiovascular system's role is to supply blood to organs and tissues.
Pericardium
Pericardium
A sac around the heart composed of the fibrous, parietal, and visceral layers.
Myocardium
Myocardium
The heart wall's middle layer, made of cardiac muscle.
Endocardium
Endocardium
Signup and view all the flashcards
Coronary Circulation
Coronary Circulation
Signup and view all the flashcards
Atria
Atria
Signup and view all the flashcards
Ventricles
Ventricles
Signup and view all the flashcards
Tricuspid Valve
Tricuspid Valve
Signup and view all the flashcards
Pulmonary Semilunar Valve
Pulmonary Semilunar Valve
Signup and view all the flashcards
Mitral (Bicuspid) Valve
Mitral (Bicuspid) Valve
Signup and view all the flashcards
Aortic Semilunar Valve
Aortic Semilunar Valve
Signup and view all the flashcards
Chordae Tendineae & Papillary Muscles
Chordae Tendineae & Papillary Muscles
Signup and view all the flashcards
Cardiac Conduction Pathway
Cardiac Conduction Pathway
Signup and view all the flashcards
Sinoatrial (SA) Node
Sinoatrial (SA) Node
Signup and view all the flashcards
Atrioventricular (AV) Node
Atrioventricular (AV) Node
Signup and view all the flashcards
Cardiac Cycle
Cardiac Cycle
Signup and view all the flashcards
Systole
Systole
Signup and view all the flashcards
Diastole
Diastole
Signup and view all the flashcards
First Heart Sound (S1)
First Heart Sound (S1)
Signup and view all the flashcards
Second Heart Sound (S2)
Second Heart Sound (S2)
Signup and view all the flashcards
Cardiac Output
Cardiac Output
Signup and view all the flashcards
Stroke Volume
Stroke Volume
Signup and view all the flashcards
Ejection Fraction
Ejection Fraction
Signup and view all the flashcards
Starling’s Law of the Heart
Starling’s Law of the Heart
Signup and view all the flashcards
Nervous System Regulation
Nervous System Regulation
Signup and view all the flashcards
Epinephrine
Epinephrine
Signup and view all the flashcards
Aldosterone
Aldosterone
Signup and view all the flashcards
Atrial Natriuretic Peptide
Atrial Natriuretic Peptide
Signup and view all the flashcards
Arteries and Arterioles
Arteries and Arterioles
Signup and view all the flashcards
Veins and Venules
Veins and Venules
Signup and view all the flashcards
Capillaries
Capillaries
Signup and view all the flashcards
Precapillary Sphincter
Precapillary Sphincter
Signup and view all the flashcards
Blood Pressure
Blood Pressure
Signup and view all the flashcards
Peripheral Resistance
Peripheral Resistance
Signup and view all the flashcards
Venous Return
Venous Return
Signup and view all the flashcards
Pulse Pressure
Pulse Pressure
Signup and view all the flashcards
Renin-Angiotensin-Aldosterone
Renin-Angiotensin-Aldosterone
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Systemic Circulation
Systemic Circulation
Signup and view all the flashcards
Hepatic Portal Circulation
Hepatic Portal Circulation
Signup and view all the flashcards
Atherosclerosis
Atherosclerosis
Signup and view all the flashcards
MI Symptoms in Older Adults
MI Symptoms in Older Adults
Signup and view all the flashcards
Pain Assessment
Pain Assessment
Signup and view all the flashcards
Orthostatic Hypotension
Orthostatic Hypotension
Signup and view all the flashcards
Pulse Deficit
Pulse Deficit
Signup and view all the flashcards
Thrill
Thrill
Signup and view all the flashcards
Bruit
Bruit
Signup and view all the flashcards
Cyanosis
Cyanosis
Signup and view all the flashcards
Clubbing
Clubbing
Signup and view all the flashcards
Pitting Edema
Pitting Edema
Signup and view all the flashcards
Study Notes
Normal Cardiovascular System
- The cardiovascular system perfuses organs and tissues with blood and consists of the heart, blood, and blood vessels.
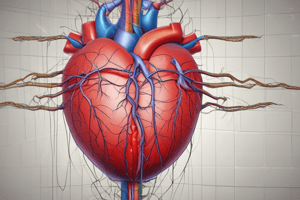
Cardiac Structure and Function
- The heart resides in the mediastinum within the thoracic cavity.
- The heart is enclosed by the fibrous pericardium, parietal pericardium serous membrane, and visceral pericardium (epicardium).
- Serous fluid between the parietal and visceral layers prevents friction during heartbeats.
- The heart chamber walls consist of cardiac muscle (myocardium), lined with endocardium to prevent abnormal clotting.
- Epithelium covering the heart valves and blood vessels is referred to as endothelium.
- Coronary circulation delivers oxygenated blood to the myocardium and returns deoxygenated blood to the right atrium via the coronary sinus.
- The two main coronary arteries branch off the ascending aorta just outside the left ventricle.
- The interatrial septum separates the right and left atria (superior chambers), while the interventricular septum separates the right and left ventricles (lower chambers).
- Both septa consist of myocardium.
Coronary Blood Flow
- The right atrium receives deoxygenated blood from the coronary sinus, superior vena cava (upper body), and inferior vena cava (lower body).
- Blood flows from the right atrium, through the tricuspid valve, and into the right ventricle.
- The tricuspid valve prevents backflow during ventricular systole.
- The right ventricle pumps blood through the pulmonary semilunar valve to the lungs via the pulmonary trunk and arteries.
- The pulmonary semilunar valve prevents backflow during ventricular diastole.
- The left atrium receives oxygenated blood from the lungs via the four pulmonary veins.
- Blood flows through the mitral (bicuspid) valve into the left ventricle.
- The mitral valve prevents backflow during ventricular systole.
- The left ventricle pumps blood through the aortic semilunar valve to the body via the aorta.
- The aortic valve prevents backflow during ventricular diastole.
- Chordae tendineae and papillary muscles anchor the tricuspid and mitral valves to the ventricle floor, preventing hyperextension during ventricular systole.
- The left ventricle pumps with approximately five times the force of the right ventricle to circulate blood throughout the body, resulting in a large difference between systemic and pulmonary blood pressure.
Cardiac Conduction Pathway and Cardiac Cycle
- The cardiac conduction pathway is the route of electrical impulses that generate each heartbeat.
- The sinoatrial (SA) node in the right atrium wall depolarizes about 100 times per minute, initiating each heartbeat.
- Parasympathetic fibers slow the SA node to about 75 beats per minute at rest.
- The SA node is known as the pacemaker, producing a normal sinus rhythm.
- Impulses travel from the SA node along a specific path.
- If the SA node is nonfunctional, the AV node can initiate heartbeats at a slower rate of 40 to 60 beats per minute.
- The bundle of His can generate ventricular beats, but at an even slower rate of about 20 to 35 beats per minute.
- A cardiac cycle involves the simultaneous contraction of both atria, followed by the simultaneous contraction of both ventricles.
- Systole is the contraction/emptying phase, while diastole is the relaxation/filling phase for each set of chambers.
- The first major heart sound ("lub") is caused by the closure of the AV valves during ventricular systole.
- The second sound ("dub") is created by the closure of the aortic and pulmonary semilunar valves.
Cardiac Output
- Cardiac output is the amount of blood ejected from the left ventricle in 1 minute.
- Cardiac output is calculated by multiplying stroke volume by heart rate.
- Stroke volume is the amount of blood ejected by a ventricle in one contraction.
- Stroke volume It averages 60 to 80 mL/beat.
- Average resting cardiac output is 5 to 6 L, which is approximately the total blood volume, with an average resting heart rate of 75 beats per minute.
- Ejection fraction measures ventricular efficiency, normally 55% to 70%.
- Starling’s law of the heart explains that during exercise, increased venous return stretches the ventricular myocardium, causing more forceful contractions and increased stroke volume.
- During exercise, heart rate increases, resulting in a cardiac output increase by as much as four times the resting level (or more for athletes).
Regulation of Heart Rate
- The heart generates its electrical impulse at the SA node.
- The nervous system can modify the heart rate in response to environmental factors.
- The medulla oblongata in the brain processes sensory input and regulates heart function.
Hormones and the Heart
- Epinephrine, secreted by the adrenal medulla during stress, increases heart rate and contraction force, and dilates coronary vessels, leading to increased cardiac output and systolic blood pressure.
- Aldosterone, from the adrenal cortex, regulates blood levels of sodium and potassium, which are essential for normal myocardial electrical activity.
- Atrial natriuretic peptide/hormone, secreted by the atria, increases sodium excretion by the kidneys by inhibiting aldosterone secretion.
- Atrial natriuretic peptide is secreted in response to higher blood pressure or blood volume stretching the atrial walls, which leads to increased water loss in urine and decreased blood volume and blood pressure.
Blood Vessels
- Arteries and arterioles carry blood from the heart to capillaries and have relatively thick walls composed of three layers, which carry blood under high pressure.
- The outer layer of fibrous connective tissue prevents arterial rupture.
- The middle layer of smooth muscle and elastic connective tissue contributes to blood pressure, specifically diastolic pressure, by altering the artery's diameter.
- The sympathetic nervous system primarily regulates artery diameter.
- Arteries can direct blood volume using smooth muscle.
- The inner layer, or lining, of the artery is simple squamous epithelium called endothelium to prevent abnormal clotting.
- Veins and venules carry blood from capillaries to the heart.
- Veins have thinner walls with less smooth muscle than arteries, but sympathetic impulses can constrict them.
- Vein linings have endothelium to prevent abnormal clotting and valves to prevent backflow, especially in the extremities.
- Capillaries connect arterioles to venules, forming networks in most tissues except cartilage, covering/lining epithelia, and the lens and cornea of the eye.
- Capillary walls consist of a single cell layer to facilitate gas, nutrient, and waste exchange between blood and tissues.
- Precapillary sphincters regulate blood flow through capillary networks, contracting or relaxing based on tissue needs.
- Active tissues cause dilation of precapillary sphincters to increase blood flow.
- Inactive tissues cause constriction of precapillary sphincters to reduce blood flow.
- The redirection of blood flow ensures that the fixed blood volume is directed to where it is most needed.
- Exchange between blood and tissue fluids primarily involves diffusion of gases and filtration for extracellular fluid homeostasis.
- Tissue fluid returns to the capillaries and lymph capillaries, with lymph returned to the blood via lymph vessels.
- Increased capillary blood pressure can lead to excess tissue fluid formation, potentially causing edema if lymph vessels cannot collect it all.
Blood Pressure
- Blood pressure refers to the force of blood against blood vessel walls, measured in millimeters of mercury (mm Hg), systolic over diastolic.
- The standard average systemic arterial pressure is 120/80 mm Hg.
- Blood pressure decreases in arterioles and capillaries, merging systolic and diastolic pressures.
- Blood pressure falls further as blood enters the veins, approaching zero as it flows into the right ventricle.
- Normal capillary blood pressure permits appropriate tissue nourishment via filtration, while being low enough to prevent rupture.
- Arterioles (and veins during sympathetic stimulation) are usually slightly constricted, maintaining normal blood pressure, especially diastolic pressure.
- Peripheral resistance is regulated by the vasomotor center of the medulla, which receives input via the glossopharyngeal and vagus nerves.
- Blood pressure is also affected by heart rate and force.
- Rapid heart rates can decrease cardiac output and blood pressure because the ventricles do not fill completely.
- Adequate venous return ensures strong heart contractions, while decreased venous return results in weaker contractions.
- Venous return relies on constriction of the veins, skeletal muscle pumping, and the diaphragm's pressure during inhalation.
- Venous valves prevent backflow and aid in blood return to the heart.
- Arterial elasticity absorbs some force during ventricular contraction and exerts pressure during ventricular relaxation, contributing to normal blood pressure and pulse pressure.
- Normal systolic to diastolic to pulse pressure ratio is 3:2:1.
Renin-Angiotensin-Aldosterone Mechanism
- Decreased blood flow through the kidneys triggers renin secretion, initiating the renin-angiotensin-aldosterone mechanism to raise blood pressure.
- Other hormones affecting blood pressure include norepinephrine and epinephrine from the adrenal medulla, which increase cardiac output and cause vasoconstriction.
- Antidiuretic hormone, released from the posterior pituitary, increases water reabsorption by the kidneys, increasing blood volume and blood pressure.
- Atrial natriuretic peptide, secreted by the heart's atria, inhibits aldosterone secretion, increasing renal excretion of sodium and water, decreasing blood volume and subsequently blood pressure.
Circuits of Circulation
- Pulmonary circulation begins at the right ventricle, which pumps deoxygenated blood toward the lungs for gas exchange, and oxygenated blood returns to the left atrium via the pulmonary veins.
- Low pressure in the pulmonary capillaries prevents filtration and keeps fluid from accumulating in the alveoli of the lungs.
- Systemic circulation starts in the left ventricle, pumping oxygenated blood into the aorta, which branches into capillaries within tissues, and deoxygenated blood returns to the right atrium via the vena cava and coronary sinus.
- The hepatic portal circulation is a part of the systemic circulation where blood from the digestive organs and spleen flows through the portal vein into the sinusoids in the liver before returning to the heart.
- The liver regulates blood levels of nutrients and removes potential toxins.
Aging and the Cardiovascular System
- Aging of blood vessels, particularly arteries, begins in childhood, with effects becoming apparent later in life.
- Atherosclerosis is the deposition of lipids in artery walls over years, which narrows the lumens and forms surfaces that may stimulate intravascular clot formation.
- Atherosclerosis decreases blood flow to affected organs.
- With age, the heart muscle becomes less efficient, decreasing maximum cardiac output and heart rate.
- Valves may thicken due to fibrosis, causing heart murmurs.
Cardiovascular Disease
- An estimated 121.5 million American adults have one or more types of cardiovascular disease.
- Lifestyle and access to health care greatly influence cardiovascular disease risk factors.
- Ways to improve cardiovascular health include not smoking, exercising, eating healthy, and maintaining normal blood pressure, blood glucose, total cholesterol levels, and weight.
- Culturally competent engagement in health promotion and disease prevention education is important to address and reduce heart disease risk in all racial and ethnic groups.
- Cardiovascular disease is the greatest cause of death in women.
Cardiovascular System Data Collection
- Data collection for cardiovascular disorders entails a patient health history and physical examination.
- Focus on the most serious signs, symptoms, and physical findings until the patient is stabilized if they have an acute problem.
- Older adults may show atypical signs and symptoms of myocardial infarction.
- Data collection focuses on allergies, medications, medical disorders, surgeries, and functional limitations.
- Observe the patient’s general appearance and record height, weight, and vital signs.
Health History Questions
- Focus on pain WHAT'S UP: where, how, aggravating/alleviating factors, timing, severity, useful data, perception.
- Assess dyspnea: what increases or relieves shortness of breath?
- Assess palpitations or irregular heartbeats: heart racing, pounding, or skipping beats?
- Assess fatigue: change in energy level? Ability to perform activities?
- Assess edema: swelling in feet, legs, or hands? Weight gain?
- Assess paresthesia: numbness, tingling, or abnormal sensations in extremities?
- Ask about childhood diseases: rheumatic fever or scarlet fever?
- Assess modifiable risk factors: diet, exercise, smoking, and stressors.
- Ask about family history: cardiovascular disorders in family?
Physical Examination
- Bradycardia, tachycardia, hypotension, and hypertension may indicate cardiovascular problems.
- Crackles and wheezes may indicate left-sided heart failure.
- Jugular vein distention and edema may indicate right-sided heart failure.
- Heart sounds, such as S3 and S4, may indicate heart failure or other cardiac issues.
- Murmurs may indicate valvular disease.
- Skin discoloration may indicate tissue hypoxia or blood flow problems.
- Normal blood pressure is considered less than 120/80 mm Hg.
- Compare readings in both arms, and report differences to the health-care provider (HCP).
Accurate Blood Pressure Measurements
- The patient should avoid exercise, caffeine, and smoking for 30 minutes before the blood pressure (BP) measurement.
- The patient should void before taking the BP measurement.
- Use the auscultatory method with a properly calibrated and validated BP instrument.
- Seat the patient quietly for at least 5 minutes in a chair (not on an examination table) with feet on the floor and arm supported at heart level before the BP measurement.
- Use the appropriate-sized cuff so that the cuff bladder encircles at least 80% of arm when placed 1 inch above the antecubital fossa.
- Ask the patient to remain still and quiet during BP measurement, as motion alters reading.
- Determine the patient’s baseline blood pressure by inflating cuff and noting the reading when the radial pulse is no longer felt. When taking BP, inflate the cuff to 20 numbers above the obtained baseline reading. (Overinflation may cause inaccurate reading.)
- During BP measurement, deflate the cuff slowly at rate of 2 mm Hg/second.
- Take at least two BP measurements and average them.
- Systolic BP is the first of two or more sounds heard and that diastolic BP is the final sound before the disappearance of sounds.
- Provide patients, verbally and in writing, with their specific BP reading.
Orthostatic Blood Pressure
- In response to the drop in blood pressure, the pulse increases 15 to 20 beats per minute to maintain cardiac output.
- Orthostatic hypotension (postural hypotension) is a drop in systolic blood pressure greater than 15 mm Hg, a drop or slight increase in diastolic blood pressure greater than 10 mm Hg, and an increase in heart rate greater than 20 beats per minute in response to the drop in blood pressure.
- It indicates a problem that should be investigated by the HCP.
- The patient often reports lightheadedness or syncope because the drop in blood pressure decreases the amount of oxygen-rich blood traveling to the brain.
- Factors that may cause orthostatic hypotension include deficient fluid volume, diuretics, analgesics, or pain.
- Anticipate orthostatic hypotension with position changes to reduce risk of falls
Pulses
- Auscultate the apical pulse for 1 minute to identify rate and regularity.
- Normal heart rate is 60 to 100 beats per minute.
- The heart rate is often slower, around 50 beats per minute in athletic people.
- Compare the apical rate with the radial rate for equality.
- Fewer radial beats than apical beats indicate a pulse deficit.
- Palpate arterial pulses bilaterally for volume and pressure quality and compare for equality and described on a four-point scale: 0 absent; 1+ weak, thready; 2+ normal; and 3+ bounding.
- A normal vessel feels soft and springy; a sclerotic vessel feels stiff.
- A vibration is felt, called a thrill in abnormal vessels.
- Humming is heard because of turbulent blood flow through the vessel, called a bruit when auscultating an abnormal vessel.
Respirations
- Observe the rate and ease of respirations and auscultate breath sounds.
- Note sputum characteristics such as amount, color, and consistency.
- Pink, frothy sputum indicates acute heart failure.
Inspection
- Note shortness of breath when the patient speaks or moves.
- Note the patient’s oxygenation status through skin, mucous membrane, lip, and nailbed color.
- Pallor may indicate anemia or lack of arterial blood flow.
- Distention of the internal and external jugular neck veins indicates an increase in the venous volume, often caused by right-sided heart failure.
- A capillary refill time is normally 3 seconds or less
- Capillary refill time briefly squeeze the patient’s nailbed
- Clubbing of the nailbeds occurs from oxygen deficiency
Learning Tip Ps of peripheral vascular disease:
- Pain
- Paresthesia (decreased sensation)
- Pallor
- Pulselessness
- Paralysis
- Poikilothermia (assumes temperature of the environment)
Palpation
- An enlarged heart may shift the PMI to the left of the midclavicular line.
- Palpate the temperature of the extremities bilaterally for comparison to determine sufficient arterial blood flow.
- If the finger imprint or indentation remains, the edema is pitting
Auscultation
- Normal heart sounds are produced by the closing of the heart valves.
- Erb’s point is where S2 is best heard.
- S1 is heard at the beginning of systole as “lub” when the tricuspid and mitral (AV) valves close.
- S2 is heard at the start of diastole as “dub” when the aortic and pulmonic semilunar valves close.
- With the bell of the stethoscope placed at the apex, a third heart sound (S3) or a fourth heart sound (S4) may be heard.
- The S3 heart sound is normal for younger adults sounds like a gallop and is a low-pitched sound heard early in diastole.
- The S4 heart sound is also a low-pitched sound, similar to a gallop but heard late in diastole.
Learning Tip:
- This sentence can help you remember the heart’s auscultation points:
- All (aortic)
- People (pulmonic)
- Eat (Erb’s point)
- Three (tricuspid)
- Meals (mitral)
- Murmurs are caused by a narrowed valve opening or a valve that does not close tightly and is a prolonged, swishing sound that ranges in intensity from faint to very loud.
- A pericardial friction rub occurs from inflammation of the pericardium and has a grating sound that occurs when the pericardial surfaces rub together during a heartbeat.
Diagnostic Tests
- Diagnostic test results are combined with the health history and physical data collection to diagnose disorders and plan care for the patient.
- Additional tests can identify genetic and inflammation factors contributing to cardiovascular risk to develop a preventive plan of care for the patient.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.