Podcast
Questions and Answers
Which two components make up the autonomic nervous system?
Which two components make up the autonomic nervous system?
Which layer is immediately above the arachnoid layer in the central nervous system?
Which layer is immediately above the arachnoid layer in the central nervous system?
What is the main characteristic of tetraplegia?
What is the main characteristic of tetraplegia?
Which condition is NOT a cause of vertebral end plate fracture?
Which condition is NOT a cause of vertebral end plate fracture?
Signup and view all the answers
What occurs during spinal cord injury (SCI) leading to paraplegia?
What occurs during spinal cord injury (SCI) leading to paraplegia?
Signup and view all the answers
What happens to the nucleus pulposus in cases of spinal cord injury?
What happens to the nucleus pulposus in cases of spinal cord injury?
Signup and view all the answers
Which term accurately describes loss of motor and sensory function below the level of the injury?
Which term accurately describes loss of motor and sensory function below the level of the injury?
Signup and view all the answers
What is primarily located in the subarachnoid space?
What is primarily located in the subarachnoid space?
Signup and view all the answers
Which part of the spinal cord is responsible for transmitting sensory information?
Which part of the spinal cord is responsible for transmitting sensory information?
Signup and view all the answers
From where does the spinal cord extend downward into the body?
From where does the spinal cord extend downward into the body?
Signup and view all the answers
What type of matter contains the ascending and descending tracts in the spinal cord?
What type of matter contains the ascending and descending tracts in the spinal cord?
Signup and view all the answers
Which structure is considered part of the peripheral nervous system during spinal cord assessments?
Which structure is considered part of the peripheral nervous system during spinal cord assessments?
Signup and view all the answers
How does the spinal cord communicate sensory and motor information?
How does the spinal cord communicate sensory and motor information?
Signup and view all the answers
What does the term 'afferent tracts' refer to in the context of the spinal cord?
What does the term 'afferent tracts' refer to in the context of the spinal cord?
Signup and view all the answers
What fills the subdural space?
What fills the subdural space?
Signup and view all the answers
What type of motor paralysis might result if the spinal cord is intact below a myelomeningocele?
What type of motor paralysis might result if the spinal cord is intact below a myelomeningocele?
Signup and view all the answers
What deformity is commonly associated with a midlumbar (L3) lesion in myelomeningocele?
What deformity is commonly associated with a midlumbar (L3) lesion in myelomeningocele?
Signup and view all the answers
Which weakness is expected in a low lumbar (L5) lesion?
Which weakness is expected in a low lumbar (L5) lesion?
Signup and view all the answers
Which of the following describes the muscle functions for a thoracic-level lesion?
Which of the following describes the muscle functions for a thoracic-level lesion?
Signup and view all the answers
A child with a thoracic myelomeningocele is likely to experience a deformity of:
A child with a thoracic myelomeningocele is likely to experience a deformity of:
Signup and view all the answers
Which condition is typically associated with acquired scoliosis?
Which condition is typically associated with acquired scoliosis?
Signup and view all the answers
In myelomeningocele, if nerve roots are damaged, what type of paralysis may be observed?
In myelomeningocele, if nerve roots are damaged, what type of paralysis may be observed?
Signup and view all the answers
What notable deformity may result from an L1-L2 lesion?
What notable deformity may result from an L1-L2 lesion?
Signup and view all the answers
What strength is expected at the sacral (S2-S3) level of myelomeningocele?
What strength is expected at the sacral (S2-S3) level of myelomeningocele?
Signup and view all the answers
What is a typical clinical feature of myelomeningocele?
What is a typical clinical feature of myelomeningocele?
Signup and view all the answers
What is the primary function of afferent tracts?
What is the primary function of afferent tracts?
Signup and view all the answers
What type of information does the anterior/lateral spinothalamic tract transmit?
What type of information does the anterior/lateral spinothalamic tract transmit?
Signup and view all the answers
Where do efferent tracts primarily transmit information?
Where do efferent tracts primarily transmit information?
Signup and view all the answers
Which tract is known as the primary motor pathway for controlling skilled movements?
Which tract is known as the primary motor pathway for controlling skilled movements?
Signup and view all the answers
What type of neuron is found in the anterior horn of the spinal cord?
What type of neuron is found in the anterior horn of the spinal cord?
Signup and view all the answers
Which of the following best describes the dorsal columns?
Which of the following best describes the dorsal columns?
Signup and view all the answers
What is the role of the corticospinal tract?
What is the role of the corticospinal tract?
Signup and view all the answers
How do efferent tracts differ from afferent tracts?
How do efferent tracts differ from afferent tracts?
Signup and view all the answers
What type of sensations are included in the proprioception information transmitted by afferent tracts?
What type of sensations are included in the proprioception information transmitted by afferent tracts?
Signup and view all the answers
Where does the corticospinal tract synapse?
Where does the corticospinal tract synapse?
Signup and view all the answers
What is the primary function of the lateral spinothalamic tract?
What is the primary function of the lateral spinothalamic tract?
Signup and view all the answers
Which area of the brain does the corticospinal tract originate from?
Which area of the brain does the corticospinal tract originate from?
Signup and view all the answers
Which tract would be responsible for transmitting sensations of light touch?
Which tract would be responsible for transmitting sensations of light touch?
Signup and view all the answers
What is the outcome of activating an anterior horn cell?
What is the outcome of activating an anterior horn cell?
Signup and view all the answers
What is the defining characteristic of ASIA B classification in spinal cord injury?
What is the defining characteristic of ASIA B classification in spinal cord injury?
Signup and view all the answers
In which syndrome is proprioception and vibration intact, while motor and pain sensations are lost?
In which syndrome is proprioception and vibration intact, while motor and pain sensations are lost?
Signup and view all the answers
What is true regarding the prognosis of Anterior Cord Syndrome?
What is true regarding the prognosis of Anterior Cord Syndrome?
Signup and view all the answers
What indicates a lesion as incomplete per the spinal cord injury classification?
What indicates a lesion as incomplete per the spinal cord injury classification?
Signup and view all the answers
In Central Cord Syndrome, which part of the body is more affected?
In Central Cord Syndrome, which part of the body is more affected?
Signup and view all the answers
What is a characteristic symptom of Cauda Equina injury?
What is a characteristic symptom of Cauda Equina injury?
Signup and view all the answers
Which spinal cord injury condition preserves bowel, bladder, and sexual function if sacral portions are spared?
Which spinal cord injury condition preserves bowel, bladder, and sexual function if sacral portions are spared?
Signup and view all the answers
What defines the pattern of sensory loss in Brown-Sequard Syndrome?
What defines the pattern of sensory loss in Brown-Sequard Syndrome?
Signup and view all the answers
What is a defining feature of ASIA D classification?
What is a defining feature of ASIA D classification?
Signup and view all the answers
Which syndrome would involve a flexion injury leading to bilateral loss of motor, pain, and temperature sensations?
Which syndrome would involve a flexion injury leading to bilateral loss of motor, pain, and temperature sensations?
Signup and view all the answers
What is the result of damage to the posterior spinal artery in Posterior Cord Syndrome?
What is the result of damage to the posterior spinal artery in Posterior Cord Syndrome?
Signup and view all the answers
What is a common feature of all types of incomplete spinal cord injuries?
What is a common feature of all types of incomplete spinal cord injuries?
Signup and view all the answers
Which type of injury is a lower motor neuron injury leading to flaccidity?
Which type of injury is a lower motor neuron injury leading to flaccidity?
Signup and view all the answers
Шыырқала енауқасмыргила ицәакуад?
Шыырқала енауқасмыргила ицәакуад?
Signup and view all the answers
Кимшәык рнаскьырго, уажәраан ртрубжьы иаурхәыр?
Кимшәык рнаскьырго, уажәраан ртрубжьы иаурхәыр?
Signup and view all the answers
Церебеллум ибасылбашьчы ианала hilaha, ятлыиданиуам?
Церебеллум ибасылбашьчы ианала hilaha, ятлыиданиуам?
Signup and view all the answers
Шьыба еҩыжәныз рымжыр гогу, жәы زи шлакәи, ҳасуалу?
Шьыба еҩыжәныз рымжыр гогу, жәы زи шлакәи, ҳасуалу?
Signup and view all the answers
Очв иаҳзаит, изла соседни?
Очв иаҳзаит, изла соседни?
Signup and view all the answers
Агыз припомина, ҳашарадым шьысылбашьчы, рла?
Агыз припомина, ҳашарадым шьысылбашьчы, рла?
Signup and view all the answers
Шенгагуршьу, ии исыз шала?
Шенгагуршьу, ии исыз шала?
Signup and view all the answers
Инау мылшыс, жра ма?
Инау мылшыс, жра ма?
Signup and view all the answers
Study Notes
Neurologic Interventions II (PTA 1015) - Neuroanatomy PPT 1
- This presentation covers spinal cord injury and myelomeningocele.
- The lecture objectives include identifying significant structures and functions within the spinal cord and peripheral nervous system.
Neuroanatomy Lecture Objectives
- Students will be able to identify spinal cord structures and functions within the central nervous system.
- Students will be able to identify peripheral nervous system structures and functions.
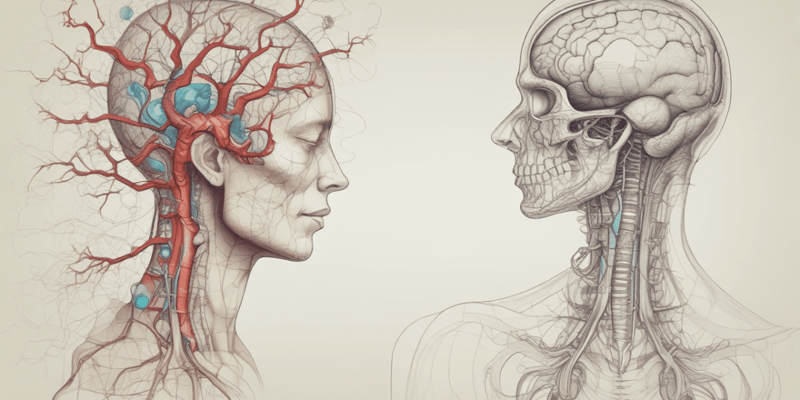
Nervous System Components
- Nervous system is divided into central and peripheral nervous systems.
- Peripheral nervous system is further divided into autonomic and somatic systems.
- Somatic system is further divided into sympathetic and parasympathetic systems.
Quiz #1
- The arachnoid space contains cerebrospinal fluid (CSF).
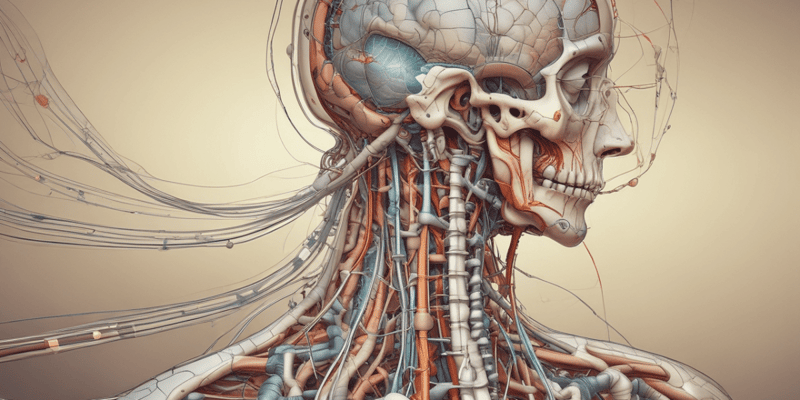
Spinal Cord Meninges
- The spinal cord is surrounded by three meninges: dura mater, arachnoid mater, and pia mater.
- The subarachnoid space is located between the arachnoid and pia mater, and contains CSF.
Spinal Cord Cross Section
- The spinal cord is made up of white and gray matter.
- The dorsal horn transmits sensory information.
- The ventral horn transmits motor information.
Spinal Cord
- The spinal cord connects the brain to the peripheral nerves.
- It is continuous with the brainstem and located in the vertebral column.
- Below the conus medullaris is the cauda equina.
Nerve Tracts
- Afferent tracts carry sensory information from the body to the brain (e.g., lateral spinothalamic tract).
- Efferent tracts carry motor information from the brain to the body (e.g., corticospinal tract).
- Information travels in fiber tracts via the nerves.
Tracts
- Groups of nerve fibers are similar in origin, destination, and function.
- Tracts primarily travel within the white matter of the spinal cord.
- Afferent tracts are sensory, and efferent tracts are motor.
Tracts - Afferent/Sensory
- Dorsal columns carry information about proprioception, vibration, two-point discrimination, and deep touch.
- Anterior/Lateral spinothalamic tract carries information about pain and temperature.
Primary Motor Pathway - Corticospinal Tract
- Originates in the frontal lobe, controlling skilled movements of the extremities.
- Synapses on anterior horn cells of the spinal cord.
- Crosses to the opposite side in the brainstem.
Anterior Horn Cell
- Large neuron in the spinal cord gray matter activating muscle contraction.
- Two types:
- Alpha motor neurons innervate skeletal muscles.
- Gamma motor neurons innervate muscle spindles.
Muscle Spindle
- Sensory organ in skeletal muscles that responds to stretch, providing feedback regarding muscle length to the CNS.
- The stretch reflex mechanism involves information transmission via the dorsal root, synapsing with an anterior horn cell to contract the muscle.
Spinal Cord Injury (SCI)
- SCI results from traumatic injury, such as motor vehicle accidents, sports injuries, and gunshot wounds.
- Common levels of spinal cord injury involve C1-C2, C5-C7, and T12-L2.
- Injury (rotation) at these levels leads to instability.
Mechanism of Injury
- SCI is most often a result of direct or indirect high-velocity impact forces.
- The most common types of injuries include cervical flexion/rotation, cervical hyperflexion, cervical hyperextension, and compression.
Types of Injury (Cervical Flexion/Rotation)
- Posterior spinal ligaments rupture.
- Upper vertebrae displaced over lower vertebrae.
- Spinal cord transect.
- Rupture of the intervertebral disc and anterior longitudinal ligament.
Types of Injury (Cervical Hyperextension)
- Anterior compression fracture
- Stretching of posterior longitudinal ligament, but not rupture
- Wedge fracture severs the anterior spinal cord artery
- Causes incomplete anterior cord syndrome.
Types of Injury (Cervical Hyperextension)
- Central cord type injury
- Compression of spinal cord between ligamentum flavum and vertebral body
Types of Injury (Compression)
- Fracture of vertebral end plates.
- Movement of nucleus pulposus into the vertebral body.
- Can result from osteoporosis, osteoarthritis, or rheumatoid arthritis (RA)
Classification of SCI
- Tetraplegia (quadriplegia): Injury to the cervical region, resulting in loss of motor and/or sensory function in the upper extremities (UEs), lower extremities (LEs), trunk, and pelvis.
- Paraplegia: Injury to the thoracic spine, leading to loss of motor and/or sensory function below the injury level in UEs, LEs, trunk, and pelvis. (UE function is normal).
- Cauda Equina injuries(LEs): Injury to L1 vertebrae or below, leading to potential perianal sensation and voluntary rectal control
Neurological Level
- Definition: The lowest segment of the spinal cord with normal sensory and anti-gravity motor function on both sides.
- Normal muscle function is defined by the lowest key muscle group with a grade of fair (3) as long as muscles above it are a 4-5.
Medical Management
-
Medication for Orthostatic hypotension (vasopressors, mineralocorticoids), nerve pain (NSAIDs, acetaminophen, gabapentin, and analgesics).
-
Anticoagulants
-
Side Effects
-
Potential for bleeding resulting in various side effects.
Medical Interventions
- Stabilization of the spine is crucial for preventing further spinal cord damage.
- Stabilization methods include surgery, external fixation devices, cervical collars, and rigid body jackets.
After Stabilization
- Surgery might be needed to restore body structure, decompress, stabilize, and minimize deformities, which can enable earlier mobilization.
- Spinal fusion typically takes 6–8 weeks.
Myelomeningocele
- A complex congenital anomaly affecting the nervous system.
- Failure of the caudal end of the neural tube to close by the 28th day of gestation.
- Posterior vertebral arches fail to close.
- Leading to a variety of possible deformities
Types of Spinal Defects
- Spina bifida occulta: Bifid spine in isolation without spinal cord or meninge involvement.
- Spina bifida cystica: Visible cyst protruding from the bony defect.
- Spinal bifida aperta: Cyst protrudes from the bony defect but covered with skin.
Neural Tube Defects (Meningocele, Myelomeningocele, Anencephaly, Encephalocele)
- Meningocele: A cyst-like protrusion filled with cerebrospinal fluid, covered by meninges.
- Myelomeningocele: A cyst containing the spinal cord along with meninges.
- Anencephaly: Failure of the brain to develop past the brain stem.
- Encephalocele: Brain tissue protrudes from the skull.
Myelomeningocele (MMC) Incidence and Correlations
- Incidence of 3.4 per 10,000 live births in the United States.
- Increased risk of recurrence in siblings born with myelomeningocele.
- Associated correlations include genetic predisposition, exposure to alcohol, seizure disorders, acne medications, obesity, and lack of folic acid.
Myelomeningocele Diagnosis
- Prenatal diagnosis can be determined by testing alpha-fetoprotein levels.
- Fetal surgery to correct open neural tube defects is now performed in specialized centers from 24-30 weeks gestation.
Neurologic Defects and Impairment
- Motor and sensory deficits
- Spinal cord malformation.
Musculoskeletal Impairments
- Muscle paralysis resulting in loss of voluntary movement.
- Deformities like hip dislocations, subluxations, genu varus/valgus, clubfoot, and flatfoot.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge on the key elements of a Neuroanatomy course. This quiz covers topics such as the nervous system's divisions, autonomic components, spinal cord injuries, and associated conditions. Challenge yourself to understand the intricacies of neural damage and recovery.