Podcast
Questions and Answers
What is a common cause of respiratory muscle weakness in bedridden patients?
What is a common cause of respiratory muscle weakness in bedridden patients?
- Dermatomyositis
- Infection, especially pneumonia (correct)
- Cardiomyopathy
- Hyperkalemic periodic paralysis
Which of the following is NOT a cause of myositis?
Which of the following is NOT a cause of myositis?
- Muscle overuse (correct)
- Systemic infection
- Collagen disease
- Immunization
In dermatomyositis, which symptoms are likely to be observed?
In dermatomyositis, which symptoms are likely to be observed?
- Prolonged duration of weakness beyond days
- Skin manifestations and weakness of proximal muscles (correct)
- No muscle pain or tenderness
- Only weakness of distal muscles
What is the primary treatment for acquired myositis?
What is the primary treatment for acquired myositis?
What is the serum potassium level associated with hypokalemic periodic paralysis?
What is the serum potassium level associated with hypokalemic periodic paralysis?
What is the primary genetic disorder associated with myopathies?
What is the primary genetic disorder associated with myopathies?
Which symptom is characteristic of myopathies?
Which symptom is characteristic of myopathies?
What is a common laboratory investigation used in diagnosing myopathies?
What is a common laboratory investigation used in diagnosing myopathies?
Which type of muscular dystrophy is x-linked recessive?
Which type of muscular dystrophy is x-linked recessive?
Which of the following describes the muscle weakness in myopathies?
Which of the following describes the muscle weakness in myopathies?
What kind of physical examination finding is often seen in myopathies?
What kind of physical examination finding is often seen in myopathies?
What is one of the treatment options for managing myopathies?
What is one of the treatment options for managing myopathies?
Which of the following is NOT a known etiology of myopathies?
Which of the following is NOT a known etiology of myopathies?
Flashcards
Familial Periodic Paralysis
Familial Periodic Paralysis
A group of inherited disorders that cause temporary muscle weakness due to changes in potassium levels in the blood.
Hypokalemic Periodic Paralysis
Hypokalemic Periodic Paralysis
A type of familial periodic paralysis where low potassium levels trigger muscle weakness.
Hyperkalemic Periodic Paralysis
Hyperkalemic Periodic Paralysis
A type of familial periodic paralysis where high potassium levels trigger muscle weakness.
Myositis
Myositis
Signup and view all the flashcards
Dermatomyositis
Dermatomyositis
Signup and view all the flashcards
What are myopathies?
What are myopathies?
Signup and view all the flashcards
What are muscular dystrophies?
What are muscular dystrophies?
Signup and view all the flashcards
What is proximal muscle weakness?
What is proximal muscle weakness?
Signup and view all the flashcards
What is pseudohypertrophy?
What is pseudohypertrophy?
Signup and view all the flashcards
Why is serum creatinine phosphokinase (CPK) used in myopathy diagnosis?
Why is serum creatinine phosphokinase (CPK) used in myopathy diagnosis?
Signup and view all the flashcards
How does electromyography (EMG) help diagnose myopathies?
How does electromyography (EMG) help diagnose myopathies?
Signup and view all the flashcards
What is Fascioscapulohumeral muscular dystrophy?
What is Fascioscapulohumeral muscular dystrophy?
Signup and view all the flashcards
What is Limb Girdle Muscular Dystrophy?
What is Limb Girdle Muscular Dystrophy?
Signup and view all the flashcards
Study Notes
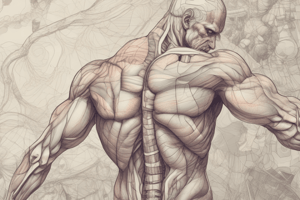
Myopathies
- Myopathies are gradual, progressive, degenerative disorders affecting muscles.
- Muscular dystrophies are a genetically determined type of myopathy, featuring a gradual, progressive degeneration of muscles.
Etiology of Myopathies
- Genetic disorders: Muscular dystrophies are one example.
- Endocrine disorders: Thyrotoxicosis, acromegaly, Cushing's syndrome
- Carcinomatous conditions: Bronchogenic and ovarian tumors
- Metabolic conditions: Periodic paralysis
- Drug-induced: Steroids, chloroquine, vincristine
- Toxic agents: Alcohol
- Infections: Trichinella spiralis
Clinical Picture of Myopathies
- Symptoms:
- Clumsy gait
- Inability to climb stairs
- Protuberant abdomen
- Weakness and wasting of specific muscle groups (selectivity)
- Signs:
- Weakness of skeletal muscles, specifically proximal muscles are affected more severely than distal muscles
- Loss of muscle tone (hypotonia), diminished reflexes (hyporeflexia) in lower motor neuron type
- Bilateral and symmetrical muscle involvement
- Winging of scapulae, pot-belly abdomen, exaggerated lumbar lordosis, waddling gait, and positive Gower's sign (indicates proximal muscle weakness) can be associated with specific types of myopathies
- Selectivity: In some dystrophies, specific muscle parts, like the sternal head of pectoralis major, are weaker than the clavicular head.
- Facial muscles: Can be affected bilaterally in some types of myopathies
- Pseudohypertrophy: Enlargement of certain muscles in some types, like quadriceps and gastrocnemius muscles in lower limbs, and deltoid, supraspinatus, and infraspinatus muscles in upper limbs
- Contractures: Can lead to bone deformities
- ECG changes: May be seen in specific types, like Duchenne muscular dystrophy
- No sensory or sphincter issues: No signs of nerve damage or issues with bladder or bowel control
Investigations
- Laboratory investigation: Serum creatine phosphokinase (CPK) levels are usually elevated in some myopathy types. Urinary creatine levels are also sometimes investigated
- Neurophysiology: Electromyography (EMG) often shows low amplitudes and durations of motor unit potentials, and early interference patterns.
- Other: Muscle biopsies (especially in dystrophinopathies) and MRI scans may also be utilized
Types of Muscular Dystrophies
- Various types exist, categorized as shoulder girdle, limb girdle, and pelvic girdle muscular dystrophies.
- Specific types include:
- Fascioscapulohumoral myopathy (AD)
- Limb girdle muscular dystrophies (AR)
- Pseudo-hypertrophic muscular dystrophy (Duchenne's and Becker's MD – X-linked recessive)
- Atrophic type (AR)
Treatment
- Physiotherapy
- Orthopedic surgery: Tenotomy for contractures
- Care of the bedridden
- Genetic counseling: To identify carriers, especially significant in familial conditions
Causes of Death in Myopathies
- Respiratory muscle weakness
- Infection (especially pneumonia)
- Cardiomyopathy
Myositis
- Definition: Acquired autoimmune inflammatory disease of skeletal muscles
- Etiology:
- Systemic infection
- Collagen disease
- Immunization
- Paraneoplastic conditions (related to cancer)
- Clinical picture:
- Acute or subacute onset with general symptoms like fatigue
- Pain and tenderness over muscles
- Weakness affecting proximal muscles of upper limbs (UL) and lower limbs (LL) , including posterior neck muscles and pharyngeal and laryngeal muscles
- Deep reflexes remain intact
- Skin manifestations may exist in dermatomyositis
- Investigations:
- Raised erythrocyte sedimentation rate (ESR)
- Raised serum CPK levels
- Electromyography (EMG) showing myopathic patterns with fibrillations
- Detection of circulating antibodies (like antinuclear antibodies, rheumatoid factor)
- Treatment:
- Prednisolone (60mg daily)
- Other immunosuppressive drugs
- Addressing the underlying cause (if any) is also crucial
Familial Periodic Paralysis
- Definition: Episodes of transient paralysis from alterations in serum potassium levels
- Hypokalaemic periodic paralysis is triggered by high carbohydrate intake, and rest after exercise, usually occurring upon waking in the morning
- Hyperkalemic periodic paralysis is triggered by cold exposure or intensive exercise immediately after exercise
- Symptoms:
- Weakness in muscles, initially in lower limbs, then upper limbs developing into quadriplegia
- Myotonia (muscle stiffness)
- Duration and intensity of paralysis: Generally hours to days in Hypokalaemic, and less then an hour in hyperkalemic types
- Serum potassium levels: Reduced in hypokalaemic and increased in hyperkalemic types
- Treatment:
- Intravenous potassium chloride (KCl) for hypokalaemia
- Calcium gluconate infusion, and oral prophylactic acetazolmide, plus glucose and insulin infusions for hyperkalemia
- Thiazide diuretics in hyperkalemia
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.