Podcast
Questions and Answers
What is the result of muscle disuse for years?
What is the result of muscle disuse for years?
- No effect on muscle function
- Immediate return of muscle function
- Decreased functional return of the muscle with no return of function after 1 to 2 years (correct)
- Complete recovery of muscle function
What happens to the number of sarcomeres per fiber in skeletal muscle remodeling?
What happens to the number of sarcomeres per fiber in skeletal muscle remodeling?
- The number is unaffected
- The number often decreases (correct)
- The number remains the same
- The number increases
What replaces muscle fibers in the final stages of skeletal muscle remodeling?
What replaces muscle fibers in the final stages of skeletal muscle remodeling?
- Fibrous and fatty tissue with abundant contractile proteins
- Fibrous and fatty tissue with little contractile proteins (correct)
- Muscle fibers with enhanced contractile proteins
- Collagen fibers
What is the outcome of muscle atrophy with fiber loss?
What is the outcome of muscle atrophy with fiber loss?
What is the typical duration for the growth back of nerve supply?
What is the typical duration for the growth back of nerve supply?
What type of receptors do prostaglandins bind to?
What type of receptors do prostaglandins bind to?
What is the role of bradykinin in pain sensation?
What is the role of bradykinin in pain sensation?
Where do peripheral afferent pain fibers of both A-δ and C types have their cell bodies?
Where do peripheral afferent pain fibers of both A-δ and C types have their cell bodies?
What is the characteristic of fast pain?
What is the characteristic of fast pain?
What is the pathway involved in the emotional distress and mood impacts of pain?
What is the pathway involved in the emotional distress and mood impacts of pain?
What is the rate-limiting step in cholesterol synthesis catalyzed by?
What is the rate-limiting step in cholesterol synthesis catalyzed by?
What is the strong association between in Myasthenia Gravis (MG)?
What is the strong association between in Myasthenia Gravis (MG)?
What is the prevalence of Myasthenia Gravis (MG)?
What is the prevalence of Myasthenia Gravis (MG)?
What is the association between age and sex in Myasthenia Gravis (MG)?
What is the association between age and sex in Myasthenia Gravis (MG)?
What is the result of the inhibition of HMG-CoA reductase?
What is the result of the inhibition of HMG-CoA reductase?
Which of the following muscles are involved in mastication?
Which of the following muscles are involved in mastication?
What is the origin of the parathyroid glands?
What is the origin of the parathyroid glands?
What is the result of the expansion of the first pharyngeal pouch?
What is the result of the expansion of the first pharyngeal pouch?
At which week of development does the thyroid gland usually reach its final site in the neck?
At which week of development does the thyroid gland usually reach its final site in the neck?
What is the connection between the tubotympanic recess and the pharynx?
What is the connection between the tubotympanic recess and the pharynx?
Flashcards are hidden until you start studying
Study Notes
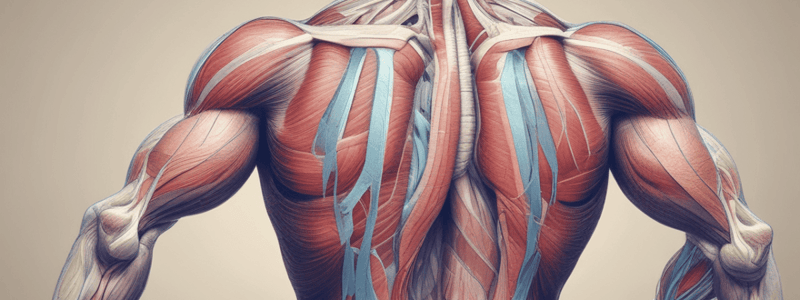
Skeletal Muscles in Action - Fiber Types
- There are two main types of muscle fibers: Type I (Slow) and Type II (Fast)
- Type I fibers:
- Smaller in size
- Innervated by smaller nerve fibers
- More capillaries to supply higher amounts of oxygen
- Lots of mitochondria to support high levels of oxidative metabolism
- Lots of myoglobin, giving a reddish appearance
- Type II fibers:
- Larger in size
- Innervated by larger nerve fibers
- Lots of SR for rapid Ca2+ release
- Lots of glycolytic enzymes present
- Energy can be derived from oxidative metabolism and anaerobic metabolism, with subtypes:
- Type IIA (Fast Oxidative Glycolytic fibers)
- Type IIB (Fast Glycolytic fibers)
Fiber Type Characteristics
- Contraction Time:
- Type I: Slow
- Type II: Faster (Type IIA), Fastest (Type IIB)
- Size of Motor Neuron:
- Type I: Small
- Type II: Bigger (Type IIA), Really big (Type IIB)
- Resistance to fatigue:
- Type I: Very resistant
- Type II: Fatigues quickly (no mitochondria)
- Activity used for:
- Type I: Low-force, endurance (postural muscles)
- Type II: High-force, quick fatigue (jumping)
- Force Production:
- Type I: Slow, lower magnitude
- Type II: Quick, higher tension
- Mitochondrial density:
- Type I: High
- Type II: Some (Type IIA), None (Type IIB)
- Capillary density:
- Type I: High
- Type II: Medium (Type IIA), Low (Type IIB)
- Oxidative capacity:
- Type I: High
- Type II: Low (Type IIA), None (Type IIB)
- Glycolytic capacity:
- Type I: Minimal
- Type II: Medium (Type IIA), High (Type IIB)
- Major Storage Fuel:
- Type I: Fat
- Type II: Glycogen (Type IIA), Glycogen (Type IIB)
Skeletal Muscle Energy Systems
- There are 3 different metabolic systems responsible for recycling AMP and ADP back into ATP:
- Phosphagen system
- Glycogen-Lactic acid system
- Aerobic system
- In the absence of oxygen, pyruvate is converted into lactate, which diffuses out of the muscle cells into the interstitial fluid and blood
- The Glycogen-Lactic acid system can sustain maximal muscle contraction for 1.3-1.6 minutes
Cori Cycle
- Glucose is converted into pyruvate in the muscle
- Pyruvate is converted into lactate, which is then transported to the liver
- In the liver, lactate is converted back into glucose through gluconeogenesis
- The Cori cycle has an overall net loss of 2 ATP
- The purpose of the Cori cycle is to recycle lactate back into glucose
Aerobic System
- In the presence of oxygen, pyruvate is broken down into carbon dioxide, water, and energy via the citric acid cycle and ETC
- The aerobic system can be used for unlimited duration, as long as nutrients in the body last
- Examples of sports that use the aerobic system include marathons and cross-country skiing
Skeletal Muscle Energy - Summary
- There are 3 different muscle metabolic systems to supply the various degrees of energy required for various activities
- The Phosphagen system provides energy for power surges (8-10 seconds)
- The Glycogen-Lactic acid system provides energy for intermediate athletic activities (60-90 seconds)
- The Aerobic system provides energy for prolonged athletic activities (unlimited duration)
Skeletal Muscle Recovery
- Energy systems must be replenished after exercise
- Phosphocreatine can be used to replenish ATP levels
- The Glycogen-Lactic acid system replenishes both phosphocreatine and ATP
- Oxidative metabolism can replenish all systems: ATP, phosphocreatine, and glycogen-lactic acid system
- Additional oxygen is needed to replenish energy stores - "oxygen debt"
Skeletal Muscle Recovery - Oxygen Debt
- After exercise, stored oxygen must be replenished by breathing extra amounts of oxygen above normal requirements
- In heavy exercise, all stored oxygen is used within ~1 minute of aerobic metabolism
- An additional 9 liters of oxygen are needed to provide for reconstituting the phosphagen system and the lactic acid system
- The total oxygen that must be "repaid" is 11.5 liters
Pain - Introduction
- Pain is an unpleasant sensation and emotional experience associated with actual or potential tissue damage.
- The emotional aspect of pain makes it unique and able to impact mood and quality of life.
- Pain perception is very subjective and can vary greatly between individuals.
Types of Pain and Abnormal Sensation
- Dysesthesia: any abnormal sensation described by a patient as unpleasant.
- Paresthesia: a sensation that is typically described as "pins-and-needles" or "prickling", but is not notably unpleasant.
- Analgesia: reduction or loss of pain perception.
- Anaesthesia: reduced perception of all touch and pain sensation.
- Hypoalgesia: decreased sensation and raised threshold to painful stimuli.
- Hyperalgesia: exaggerated pain response from a normally painful stimulus.
- Allodynia: abnormal perception of pain from a normally non-painful mechanical or thermal stimulus.
- Hyperesthesia: exaggerated perception of a touch stimulus.
- Causalgia: burning pain in the distribution of a peripheral nerve.
Physiology of Nociception
- Nociceptors are widely distributed through multiple depths in the skin and visceral organs.
- Types of nociceptors:
- Thermal nociceptors: activated by temperatures > 45 C or less than 5 C.
- Mechanical nociceptors: activated by intense pressure applied to a structure.
- Polymodal nociceptors: activated by high-intensity mechanical, chemical, or thermal stimuli.
- Silent nociceptors: receptors that are widely distributed through viscera and skin, but do not normally transmit pain information.
- Nociceptors can detect a wide range of stimuli, including:
- Cold and heat
- Low pH and free radicals
- Capsaicin
- Prostaglandins
- Bradykinin
- Histamine
- Substance P
- Serotonin
- ATP
Neuroanatomical Pain Pathways
- The spinothalamic tract is the major nociceptive sensory pathway.
- Peripheral afferent pain fibers of both A-δ and C types have their cell bodies in the dorsal root ganglia.
- The central extensions of these nerve cells project, via the dorsal root, to the dorsal horn of the spinal cord.
- Within the spinal cord, many of the thinnest fibers (C fibers) form a discrete bundle, the tract of Lissauer.
- Peripheral afferent fibers usually terminate within the same segment as their spinal nerve.
- The fibres of the spinothalamic tract usually cross over (2nd order neurons) two or three levels superior to where the 1st-order neurons enter the spinal cord.
Additional Details
- The concept of fast pain and slow pain:
- Fast pain: well-localized, sharp pain carried by A-delta fibres.
- Slow pain: poorer-localized, duller pain carried by C-fibres, tends to last longer.
Muscular Dystrophies
- Muscular dystrophies are a group of inherited muscle disorders leading to progressive weakness and muscle wasting, characterized by muscle fiber necrosis and regeneration.
- Three types of muscular dystrophies will be discussed: Duchenne Muscular dystrophy, Becker Muscular dystrophy, and Myotonic dystrophy.
Duchenne Muscular Dystrophy
- Etiology: X-linked, loss-of-function mutation of the structural protein dystrophin, typically associated with deletion or frameshift mutations resulting in a severe, progressive phenotype.
- Epidemiology: Most common muscular dystrophy, affecting 1 in 3500 live male births.
- Pathogenesis: Dystrophin is a key component of the dystrophin glycoprotein complex, which spans the plasma membrane, linking the cytoskeleton of the muscle fiber with the basement membrane.
- Pathophysiology: Defects in the complex can lead to sarcolemma tears, calcium influx, and ultimately muscle fiber necrosis.
- Pathology: Chronic muscle damage that outpaces the capacity for repair, leading to muscle fiber degeneration, regeneration, and replacement by collagen and fat cells.
Becker Muscular Dystrophy
- Less severe than Duchenne Muscular Dystrophy, with fewer extra-muscular symptoms.
- Affects more proximal-located muscles (thigh and hip), often causing myalgic pain.
Myotonic Dystrophy
- Type I: More severe, with more extra-muscular symptoms such as dysphagia, constipation, and uterine muscle abnormalities.
- Type II: Less severe, with fewer extra-muscular symptoms.
- Diagnosis: Based on history, clinical findings, and genetic testing.
- Prognosis: Reduced life expectancy, with a mean age of death of 54 years, commonly due to respiratory and cardiac disease.
Statin Myopathy
- Most common drug-related myopathy, affecting 9-17% of those on statin therapy.
- Pathophysiology: Decreased cholesterol concentrations may impact sarcolemma, and depletion of CoQ10 (Ubiquinone).
- Clinical Features: Myalgias and muscle weakness after exercise, often severe enough to discontinue or switch medication.
Myasthenia Gravis (MG)
- Etiology: Autoimmune condition associated with autoantibodies directed against acetylcholine receptors.
- Epidemiology: Prevalence of 150-200 per 1 million, more common in young females and older males.
- Thymic abnormalities (thymoma or thymic hyperplasia) are associated with MG and may contribute to immune dysregulation and development of auto-antibodies.
The Pharyngeal Arches
- A pharyngeal arch consists of a core of mesenchyme covered externally by ectoderm and internally by endoderm.
- The mesenchyme is derived from mesoderm in the third week, and later from neural crest cells that migrate into the pharyngeal arches during the fourth week.
- Each pharyngeal arch contains a pharyngeal arch artery, a cartilaginous rod, a muscular component, and sensory and motor nerves.
Pharyngeal Grooves and Pouches
- The pharyngeal endoderm lines the internal aspects of the pharyngeal arches and passes into diverticula, forming pharyngeal pouches.
- There are four pairs of pharyngeal pouches, with the fifth pair being rudimentary or absent.
- The endoderm of the pouches contacts the ectoderm of the pharyngeal grooves, forming a double-layered pharyngeal membrane.
Development of the Pharyngeal Apparatus
- The pharyngeal arches begin to develop early in the fourth week, with neural crest cells migrating into the ventral parts of the future head and neck regions.
- The first pair of pharyngeal arches, the primordium of the jaws, appears as surface elevations lateral to the developing pharynx.
- By the end of the fourth week, four pairs of pharyngeal arches are visible externally.
Bony and Cartilaginous Derivatives of the Pharyngeal Arches
- The first pharyngeal arch separates into two prominences: the maxillary prominence and the mandibular prominence.
- The maxillary prominence gives rise to the maxilla, zygomatic bone, and a portion of the vomer.
- The mandibular prominence forms the mandible and the squamous temporal bone.
- The second and third pharyngeal arches form the hyoid bone.
- The first and second pharyngeal cartilages give rise to the ossicles of the middle ear and the styloid process of the temporal bone.
- The fourth and sixth pharyngeal arches give rise to the laryngeal cartilage.
Muscular Derivatives of the Pharyngeal Arches
- The first pharyngeal arch gives rise to the muscles of mastication, muscles of the middle ear, and the tensor tympani.
- The second pharyngeal arch gives rise to the stapedius, stylohyoid, posterior belly of the digastric, auricular, and muscles of facial expression.
- The third pharyngeal arch gives rise to the stylopharyngeus.
- The fourth pharyngeal arch gives rise to the cricothyroid, levator veli palatini, and constrictors of the pharynx.
- The sixth pharyngeal arch gives rise to the intrinsic muscles of the larynx.
Pharyngeal Pouches
- The first pharyngeal pouch expands into a tubotympanic recess, which forms the tympanic cavity and mastoid antrum.
- The second pharyngeal pouch gives rise to parts of the palatine tonsils.
- The third pouch develops into parathyroid glands and a thymus.
- The fourth pouch develops into parathyroids.
Development of the Thyroid
- The thyroid gland is the first endocrine gland to develop in the embryo, forming 24 days after fertilization from a median endodermal thickening in the floor of the primordial pharynx.
- The thyroid gland descends in the neck, passing ventral to the developing hyoid bone and laryngeal cartilages.
- For a short time, the thyroid gland is connected to the tongue by a narrow tube, the thyroglossal duct.
- By 7 weeks, the thyroid gland is usually located in its final site in the neck, and the thyroglossal duct usually degenerates.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.