Podcast
Questions and Answers
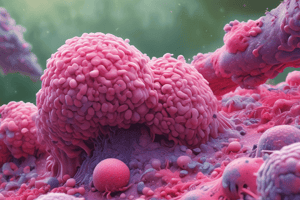
What is the primary function of mucosal-associated lymphatic tissue (MALT)?
What is the primary function of mucosal-associated lymphatic tissue (MALT)?
- Regulating systemic blood circulation
- Producing insulin in response to glucose
- Participating in the mucosal immune response (correct)
- Transporting oxygen in the bloodstream
Which cells are primarily involved in mediating mucosal immunity?
Which cells are primarily involved in mediating mucosal immunity?
- Neutrophils and eosinophils
- Macrophages and dendritic cells
- Adipocytes and fibroblasts
- B cells and T cells (correct)
What type of antibody is primarily associated with mucosal immunity?
What type of antibody is primarily associated with mucosal immunity?
- IgE
- IgA (correct)
- IgG
- IgM
How does the mucosal immune system differ from the systemic immune systems?
How does the mucosal immune system differ from the systemic immune systems?
What is one way cells and antigens are trafficked within the mucosal immune system?
What is one way cells and antigens are trafficked within the mucosal immune system?
What is the primary function of M cells in mucosal immunity?
What is the primary function of M cells in mucosal immunity?
Which antibody isotype is primarily involved in mucosal immunity due to its ability to be transcytosed through epithelial cells?
Which antibody isotype is primarily involved in mucosal immunity due to its ability to be transcytosed through epithelial cells?
How do mucosal dendritic cells contribute to oral tolerance?
How do mucosal dendritic cells contribute to oral tolerance?
Following activation in the Peyer's patches, where do B cells that have undergone isotype switching to IgA home to?
Following activation in the Peyer's patches, where do B cells that have undergone isotype switching to IgA home to?
What role does the polymeric immunoglobulin receptor (pIgR) play in mucosal immunity?
What role does the polymeric immunoglobulin receptor (pIgR) play in mucosal immunity?
Why is TLR4 expression reduced in the gut mucosa?
Why is TLR4 expression reduced in the gut mucosa?
Which anatomical feature is characteristic of the gut mucosa's adaptive immune system?
Which anatomical feature is characteristic of the gut mucosa's adaptive immune system?
What distinguishes SIgA from pIgA in mucosal immunity?
What distinguishes SIgA from pIgA in mucosal immunity?
In the context of Peyer’s patches, where are naïve B cells primarily located?
In the context of Peyer’s patches, where are naïve B cells primarily located?
What structural characteristic is unique to pIgM?
What structural characteristic is unique to pIgM?
Why are Peyer's patches considered O-MALT (organized mucosa-associated lymphoid tissue)?
Why are Peyer's patches considered O-MALT (organized mucosa-associated lymphoid tissue)?
How do antigens enter Peyer's patches?
How do antigens enter Peyer's patches?
What is the role of IgG in mucosal immunity?
What is the role of IgG in mucosal immunity?
Which of the following best describes the process of transcytosis in the context of SIgA production?
Which of the following best describes the process of transcytosis in the context of SIgA production?
What cells are found in large numbers within Peyer's Patches?
What cells are found in large numbers within Peyer's Patches?
What is the primary function of O-MALT in the mucosal immune system?
What is the primary function of O-MALT in the mucosal immune system?
Which of the following structures is NOT associated with O-MALT?
Which of the following structures is NOT associated with O-MALT?
Which type of MALT is primarily associated with antibody secretion?
Which type of MALT is primarily associated with antibody secretion?
What is one of the major differences between O-MALT and D-MALT?
What is one of the major differences between O-MALT and D-MALT?
Which component primarily makes up the effector function of D-MALT?
Which component primarily makes up the effector function of D-MALT?
What is a key characteristic of D-MALT?
What is a key characteristic of D-MALT?
What process occurs within O-MALT to create diverse antibodies?
What process occurs within O-MALT to create diverse antibodies?
Where are the majority of lymphocytes located in the body?
Where are the majority of lymphocytes located in the body?
What is primarily transcytosed across the mucosal epithelium by the pIgR?
What is primarily transcytosed across the mucosal epithelium by the pIgR?
Which type of T cells are primarily found among intraepithelial lymphocytes (IELs)?
Which type of T cells are primarily found among intraepithelial lymphocytes (IELs)?
Which structure is the main source of IgA in the oral cavity?
Which structure is the main source of IgA in the oral cavity?
What role do γδ T cells play in mucosal immunity?
What role do γδ T cells play in mucosal immunity?
What are the specialized epithelial layers that cover Peyer's patches referred to as?
What are the specialized epithelial layers that cover Peyer's patches referred to as?
What cell type is NOT found in the lamina propria of the MALT?
What cell type is NOT found in the lamina propria of the MALT?
Which proteins do γδ T cells recognize to kill infected or stressed epithelial cells?
Which proteins do γδ T cells recognize to kill infected or stressed epithelial cells?
What is the primary role of intraepithelial lymphocytes (IELs)?
What is the primary role of intraepithelial lymphocytes (IELs)?
What is the primary function of the mucus layer in the gut mucosa?
What is the primary function of the mucus layer in the gut mucosa?
Which cells are responsible for producing the main antimicrobial peptides in the small intestine?
Which cells are responsible for producing the main antimicrobial peptides in the small intestine?
How often do mucin molecules in the gut turn over?
How often do mucin molecules in the gut turn over?
What is the main role of C-type lectins secreted by Paneth cells?
What is the main role of C-type lectins secreted by Paneth cells?
What type of antimicrobial peptides are primarily produced in the large intestine?
What type of antimicrobial peptides are primarily produced in the large intestine?
What is a characteristic feature of the glycocalyx in the gut mucosa?
What is a characteristic feature of the glycocalyx in the gut mucosa?
Which cytokines play a role in the production of mucin molecules?
Which cytokines play a role in the production of mucin molecules?
Chronic disease affecting the gut may involve defects in which immune feature?
Chronic disease affecting the gut may involve defects in which immune feature?
What is the consequence of alpha-defensins on microbial membranes?
What is the consequence of alpha-defensins on microbial membranes?
What role does the thick mucus layer play in the gut's defense mechanism?
What role does the thick mucus layer play in the gut's defense mechanism?
What is the initial step for antigen uptake in the mucosal immune system?
What is the initial step for antigen uptake in the mucosal immune system?
In which location does a dendritic cell typically capture antigen after it has crossed the epithelial barrier?
In which location does a dendritic cell typically capture antigen after it has crossed the epithelial barrier?
What occurs after T cell activation in the Peyer's patch?
What occurs after T cell activation in the Peyer's patch?
Where do B cells undergo clonal proliferation after leaving the Peyer's patch?
Where do B cells undergo clonal proliferation after leaving the Peyer's patch?
What type of antibodies do memory B cells produce after returning to the lamina propria?
What type of antibodies do memory B cells produce after returning to the lamina propria?
What process occurs in the Peyer's patches that is essential for effective immune response?
What process occurs in the Peyer's patches that is essential for effective immune response?
Which of the following is true about the activated B cells in the Peyer's patch?
Which of the following is true about the activated B cells in the Peyer's patch?
What triggers isotype switching in B cells during the immune response?
What triggers isotype switching in B cells during the immune response?
Which site is responsible for antibody secretion in the mucosal immune system?
Which site is responsible for antibody secretion in the mucosal immune system?
What is the final destination of secreted pIgA after transcytosis?
What is the final destination of secreted pIgA after transcytosis?
Flashcards
Mucosal-associated lymphatic tissue (MALT)
Mucosal-associated lymphatic tissue (MALT)
MALT is a part of the immune system associated with mucosal membranes, providing defense against pathogens.
Cells of mucosal immunity
Cells of mucosal immunity
These include lymphocytes, macrophages, and specialized epithelial cells that play roles in immune defense in mucosal areas.
Mucosal immunity defenses
Mucosal immunity defenses
These include specific antibodies, enzymes, and immune cells that protect mucosal surfaces from pathogens.
Differences from humoral immunity
Differences from humoral immunity
Signup and view all the flashcards
Cell and antigen trafficking in mucosal immunity
Cell and antigen trafficking in mucosal immunity
Signup and view all the flashcards
Mucosal Immunity
Mucosal Immunity
Signup and view all the flashcards
MALT
MALT
Signup and view all the flashcards
O-MALT
O-MALT
Signup and view all the flashcards
D-MALT
D-MALT
Signup and view all the flashcards
Inductive Sites
Inductive Sites
Signup and view all the flashcards
Effector Sites
Effector Sites
Signup and view all the flashcards
GALT
GALT
Signup and view all the flashcards
NALT
NALT
Signup and view all the flashcards
Mucus in gut defense
Mucus in gut defense
Signup and view all the flashcards
Function of mucin
Function of mucin
Signup and view all the flashcards
Amount of mucus produced
Amount of mucus produced
Signup and view all the flashcards
Glycocalyx
Glycocalyx
Signup and view all the flashcards
Antimicrobial peptides in small intestine
Antimicrobial peptides in small intestine
Signup and view all the flashcards
Antimicrobial peptides in large intestine
Antimicrobial peptides in large intestine
Signup and view all the flashcards
Defects in defensins
Defects in defensins
Signup and view all the flashcards
C-type lectins
C-type lectins
Signup and view all the flashcards
Regenerating islet-derived proteins (REG III)
Regenerating islet-derived proteins (REG III)
Signup and view all the flashcards
Role of cytokines in mucin production
Role of cytokines in mucin production
Signup and view all the flashcards
Peyer’s Patch
Peyer’s Patch
Signup and view all the flashcards
pIgA
pIgA
Signup and view all the flashcards
SIgA
SIgA
Signup and view all the flashcards
Intraepithelial Lymphocytes (IELs)
Intraepithelial Lymphocytes (IELs)
Signup and view all the flashcards
γδ T cells
γδ T cells
Signup and view all the flashcards
pIgR
pIgR
Signup and view all the flashcards
Follicle Associated Epithelium (FAE)
Follicle Associated Epithelium (FAE)
Signup and view all the flashcards
Antigen uptake
Antigen uptake
Signup and view all the flashcards
M cells
M cells
Signup and view all the flashcards
APC in Peyer’s patches
APC in Peyer’s patches
Signup and view all the flashcards
T cell activation
T cell activation
Signup and view all the flashcards
Isotype switching
Isotype switching
Signup and view all the flashcards
Germinal center proliferation
Germinal center proliferation
Signup and view all the flashcards
Memory IgA B cells
Memory IgA B cells
Signup and view all the flashcards
Lamina propria function
Lamina propria function
Signup and view all the flashcards
Polymeric IgA production
Polymeric IgA production
Signup and view all the flashcards
Affinity maturation
Affinity maturation
Signup and view all the flashcards
TLR4 Expression
TLR4 Expression
Signup and view all the flashcards
Adaptive Immune Features
Adaptive Immune Features
Signup and view all the flashcards
pIgA and SIgA
pIgA and SIgA
Signup and view all the flashcards
TREG Cells and Oral Tolerance
TREG Cells and Oral Tolerance
Signup and view all the flashcards
Transcytosis
Transcytosis
Signup and view all the flashcards
IgG in Mucosal Immunity
IgG in Mucosal Immunity
Signup and view all the flashcards
Peyer's Patches
Peyer's Patches
Signup and view all the flashcards
APCs in Peyer's Patches
APCs in Peyer's Patches
Signup and view all the flashcards
Inductive & Effector Sites
Inductive & Effector Sites
Signup and view all the flashcards
CD4+ TREG Cells
CD4+ TREG Cells
Signup and view all the flashcards
Secretory IgA (SIgA)
Secretory IgA (SIgA)
Signup and view all the flashcards
Dome Area in Peyer's Patches
Dome Area in Peyer's Patches
Signup and view all the flashcards
Study Notes
Mucosal Immunity Learning Objectives
- Identify the types of mucosal-associated lymphatic tissue (MALT) and their roles in the mucosal immune response.
- Identify the cells of mucosal immunity and describe their specific roles within the mucosal immune response.
- Describe the specific defenses associated with mucosal immunity, including cells, molecules, enzymes, and types of antibodies.
- Describe how the mucosal immune system differs from humoral and cell-mediated immune systems.
- Describe how cells and antigens are trafficked within the mucosal immune system.
Mucosal Associated Lymphoid Tissues (MALT)
- Mucosal immunity is distinct from systemic immunity, with 75% of lymphocytes in mucosal tissues.
- Different antibodies, γδ T cells, physical structure, and antigen uptake mechanisms are important distinctions.
- MALT includes organized (O-MALT) and diffuse (D-MALT) tissues.
Anatomy of MALT
- O-MALT is where immune response is induced (inductive sites)
- D-MALT is where antibodies are secreted (effector sites)
- Examples of O-MALT locations include tonsils, adenoids, BALT (bronchial associated lymphoid tissue), GALT (gut associated lymphoid tissue, Peyer's patches).
- Examples of D-MALT locations include mammary glands, small intestine, large intestine, and urogenital tract.
Inductive & Effector Sites
- Inductive sites (O-MALT) are where antigen uptake, presentation, and lymphocyte activation occur.
- Effector sites (D-MALT) are where lymphocytes home back to secrete effector molecules.
- Specific examples of inductive sites and their features are provided.
- Specific examples of effector sites and their features are provided.
Innate Immune Features
- Mucous layer protects from pathogens.
- Mucin production from goblet cells provides a mucous layer that turns over every 6-12 hours.
- Various cytokines increase mucin production.
- Glycocalyx is formed by membrane-bound mucins and glycolipids, acting as a physical barrier preventing microbial contact with the epithelial layer.
- Antimicrobial peptides, such as a-defensins (small intestine) and β-defensins (large intestine), permeabilize microbial membranes and maintain gut microbial homeostasis.
- C-type lectins (REG III) block bacterial colonization and have bactericidal effects against gram-positive bacteria.
- Local PRRs (e.g., TLR5) are expressed in specific cells and areas of the gut, activated upon bacterial invasion.
- Innate lymphoid cells (ILCs) secrete cytokines in response to alarmins produced by injured or pathogen-infected epithelial cells.
- Inhibited inflammation occurs via anti-inflammatory cytokines (e.g., IL-10) and reduced TLR4 expression.
Adaptive Immune Features
- IgA plays a pivotal role in mucosal immunity (especially in the oral cavity).
- IgM is involved in mucosal immunity (and is found in oral cavity and GI tract).
- Specialized anatomy: Inductive sites and effector sites are separated anatomically.
- Specialized cells like M cells and dendritic cells (DCs) are present.
- Strong homing and lymphocyte trafficking are essential.
Oral Tolerance & Treg Cells
- M cells capture and deliver antigens to mucosal dendritic cells (DCs).
- Mucosal DCs carry food antigens to regulatory T cells (Tregs).
- This induces tolerance to food antigens by regulating inflammatory responses.
Antibodies of Mucosal Immunity
- SIgA is produced by plasma cells in the lamina propria, transcytosed through mucosal epithelium to the gut lumen by plgR.
- SIgA consists of dimeric IgA with a secretory piece for protection.
- IgG plays a role in oral cavity immunity.
- IgM and SIgM are involved in both oral cavity and GI tract immunity.
Peyer's Patches
- Found in the small intestine as O-MALT inductive sites.
- Similar to lymph node follicles, they present antigens, activate lymphocytes, and produce very little antibody.
- Covered with specialized cells different from the rest of the small intestine. Follicle-associated epithelium (FAE) and M cells are present.
- Naive B cells are located in the corona region of the Peyer's patches.
- Activated B cells (germinal centers) are located in the follicular zone below the corona.
Lamina Propria
- Part of D-MALT, it contains memory mlgA+ B cells, IgA-secreting plasma cells, and memory TH cells.
- It's where most plgA is produced and later transcytosed to become SIgA.
- DCs, macrophages, and mast cells populate it.
Salivary Glands
- Part of D-MALT.
- Produce IgA, a major source in the oral cavity.
- Most IgA secreted is in dimeric form, which becomes SIgA via plgR.
Cells of the MALT
- Mucosal epithelium organizes into villi and crypts, with lymphocytes, DCs, and macrophages interspersed.
- plgR binds plgA and plgM to enable transcytosis across the epithelium.
Intraepithelial Lymphocytes (IELs)
- Mature T cells residing in mucosal villous epithelium.
- Mostly αβ memory T cells; about 10% are γδ T cells, which recognize lipid antigens and are prevalent in mucosal tissues.
- γδ T cells play roles similar to NK cells in protecting mucosal epithelial cells from infection, injury, or stress.
Follicle Associated Epithelium (FAE)
- Specialized epithelial layer; covers Peyer's patches (Peyer's patches are also known as follicles).
- Contains M cells, which are specialized for antigen uptake.
M Cells
- Specialized antigen-uptake cells of the FAE.
- Pinocytic and have Fcα receptors to bind SIgA, transporting antigens to the Peyer's patch area.
- Ingested antigens are transcytosed and delivered to the Peyer's patch beneath.
Goblet Cells
- Secrete mucin to form mucus protecting intestinal epithelium.
- Are located on the top part (villus) and in the FAE (follicle-associated epithelium).
- Present in both small and large intestines.
Paneth Cells
- Secrete α-defensins, anti-bacterial peptides, lysozyme, and phospholipase enzymes.
- Located at the bottom of intestinal crypts.
Lymphocyte Trafficking
- In mucosal immunity, activated lymphocytes migrate to specific inductive and effector sites.
- O-MALT and D-MALT sites are linked by this homing ability, crucial for immunity.
- Lymphocytes upregulate or downregulate cell surface proteins and their ligands to enable movement into or out of mucosal tissues and lymphoid organs.
- Activated lymphocytes change their cell surface proteins to facilitate homing to specific sites by downregulating some ligands and upregulating others.
Antigen Flow in MALT
- Antigen uptake is different in mucosal immune systems.
- Antigens must be taken across the epithelial barrier by active transepithelial transport.
- Antigens are not phagocytosed until after crossing the epithelial barrier by an APC which does not migrate to a lymph node but presents antigen in local MALT tissues (e.g., Peyer's patches, tonsils) of the inductive site.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.