Podcast
Questions and Answers
What is the recommended duration for exclusive breastfeeding according to AAP?
What is the recommended duration for exclusive breastfeeding according to AAP?
- 9 months
- 6 months (correct)
- 12 months
- 4 months
What is the primary cause of jaundice in newborns?
What is the primary cause of jaundice in newborns?
- Poor feeding practices
- Overproduction of bilirubin due to liver failure
- Increased hemoglobin levels
- Shorter lifespan of RBCs (correct)
At what age does the AAP recommend introducing solid foods to infants?
At what age does the AAP recommend introducing solid foods to infants?
- 3 months
- 4 months
- 6 months (correct)
- 12 months
What are the mechanisms of neonatal heat loss?
What are the mechanisms of neonatal heat loss?
Which of the following conditions can result from untreated jaundice in newborns?
Which of the following conditions can result from untreated jaundice in newborns?
What is the purpose of the Apgar score?
What is the purpose of the Apgar score?
What is the first step in managing postpartum hemorrhage (PPH)?
What is the first step in managing postpartum hemorrhage (PPH)?
Which of the following antibiotics is commonly used to treat mastitis?
Which of the following antibiotics is commonly used to treat mastitis?
What is a common predisposing factor for mastitis in breastfeeding women?
What is a common predisposing factor for mastitis in breastfeeding women?
Which procedure is NOT part of the management for postpartum hemorrhage?
Which procedure is NOT part of the management for postpartum hemorrhage?
Which breast quadrant is most commonly affected by mastitis?
Which breast quadrant is most commonly affected by mastitis?
What is an important aspect of postpartum care to prevent infection?
What is an important aspect of postpartum care to prevent infection?
Which is NOT a symptom of mastitis?
Which is NOT a symptom of mastitis?
What should patients be taught before discharge to manage potential mastitis?
What should patients be taught before discharge to manage potential mastitis?
What is the primary consequence of hemorrhagic (hypovolemic) shock?
What is the primary consequence of hemorrhagic (hypovolemic) shock?
Which of the following is a key focus in the interprofessional care management of hemorrhagic shock?
Which of the following is a key focus in the interprofessional care management of hemorrhagic shock?
What is the role of uterine massage in the management of hemorrhage?
What is the role of uterine massage in the management of hemorrhage?
Why are postpartum urinary tract infections (UTIs) common?
Why are postpartum urinary tract infections (UTIs) common?
Which approach is most effective for preventing postpartum infection?
Which approach is most effective for preventing postpartum infection?
What is a major cause of maternal morbidity and mortality worldwide?
What is a major cause of maternal morbidity and mortality worldwide?
What condition is caused by increased amounts of glucose crossing the placenta in infants of diabetic mothers?
What condition is caused by increased amounts of glucose crossing the placenta in infants of diabetic mothers?
Which of the following is NOT a potential complication for infants of mothers with pregestational diabetes?
Which of the following is NOT a potential complication for infants of mothers with pregestational diabetes?
What distinguishes cephalhematoma from caput succedaneum?
What distinguishes cephalhematoma from caput succedaneum?
Which condition is characterized by subcutaneous edema over the presenting part of the fetal head?
Which condition is characterized by subcutaneous edema over the presenting part of the fetal head?
What is a potential volume of blood that the subgaleal compartment can hold in a 3-kg newborn?
What is a potential volume of blood that the subgaleal compartment can hold in a 3-kg newborn?
Which of these complications is NOT associated with the infant of a diabetic mother in the postnatal period?
Which of these complications is NOT associated with the infant of a diabetic mother in the postnatal period?
What is the primary goal of the interventions when managing postpartum hemorrhage?
What is the primary goal of the interventions when managing postpartum hemorrhage?
Which medication is NOT classified as a uterotonic for controlling postpartum hemorrhage?
Which medication is NOT classified as a uterotonic for controlling postpartum hemorrhage?
What is a common sign of subinvolution of the uterus?
What is a common sign of subinvolution of the uterus?
Which component is NOT part of the California Maternal Quality Care Collaborative safety bundle for obstetric hemorrhage?
Which component is NOT part of the California Maternal Quality Care Collaborative safety bundle for obstetric hemorrhage?
Which intervention is considered a surgical management option for postpartum hemorrhage?
Which intervention is considered a surgical management option for postpartum hemorrhage?
What are the 4 T's that indicate common causes of postpartum hemorrhage?
What are the 4 T's that indicate common causes of postpartum hemorrhage?
Which of the following is a symptom of inversion of the uterus?
Which of the following is a symptom of inversion of the uterus?
What is an initial nursing intervention before administering uterotonics for postpartum hemorrhage?
What is an initial nursing intervention before administering uterotonics for postpartum hemorrhage?
Flashcards are hidden until you start studying
Study Notes
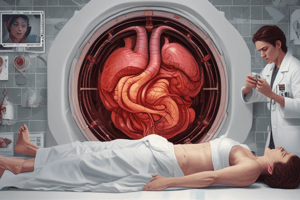
Hemorrhagic (Hypovolemic) Shock
- Emergency resulting from significant blood loss, compromising organ perfusion.
- Potentially leads to death without timely intervention.
- Interprofessional care focuses on restoring blood volume and addressing hemorrhage causes.
- Treatment includes fluid or blood replacement therapy and maintaining oxygen delivery to tissues.
Management of Hemorrhagic Shock
- Uterine massage and prompt calling of code hemorrhage are essential.
- Use a hemorrhage cart and adhere to standing orders.
- Establish large bore IV access (typically 18 or 20 gauge) for isotonic fluids.
- Ensure bladder is emptied to facilitate uterine contraction.
- Administer uterotonics such as Pitocin, Hemabate, Methergine, and Cytotec.
- Laboratory tests include CBC, Type/Screen, and preparation of blood products.
- Apply physical pressure through tamponade or devices (Foley, Bakri balloon) and remove placental products.
- Surgical options may include uterine artery embolization, removal of retained products, uterine repair, or hysterectomy.
Postpartum Hemorrhage (PPH) Management
- Importance of standardized protocols and routine emergency drills in healthcare settings.
- Utilize a safety bundle addressing readiness, recognition, prevention, response, reporting, and system learning.
- Early recognition and treatment are critical for effective management of PPH.
- Medical management includes firm uterine massage and IV oxytocin infusion.
- Surgical management may be required if medical interventions fail.
Causes of Postpartum Hemorrhage (4 T’s)
- Tone: Uterine atony due to subinvolution or inversion can lead to severe bleeding.
- Subinvolution: Delayed return of the uterus to pre-pregnancy size, often from retained placental fragments.
- Inversion: Rare but life-threatening condition where the uterus turns inside out during childbirth.
- Trauma, Tissue, Thrombin: Other potential causes of PPH requiring assessment.
Appropriate Postpartum Care
- Strict adherence to aseptic techniques during childbirth and postpartum decreases infection risks.
- Continuous vigilance and communication among healthcare personnel improve outcomes.
Newborn Nutrition and Breastfeeding
- Mastitis: infectious breast issue presenting with flu-like symptoms and localized pain, common 2-4 weeks postpartum.
- Prevention is key; educate mothers on signs of mastitis and encourage timely contact with healthcare providers.
- Treatment includes bed rest, antibiotics, and anti-inflammatory medication.
- AAP recommends exclusive breastfeeding for the first 6 months, continuing for at least 12 months, followed by solid foods introduction.
Jaundice in Newborns
- Newborns may experience jaundice at higher bilirubin levels due to shorter RBC lifespan.
- Metabolism occurs in the liver and spleen, with bilirubin binding to albumin before excretion.
- Acute bilirubin encephalopathy, or kernicterus, poses a significant risk if untreated.
Neonatal Withdrawal and Heat Loss
- Understanding of different mechanisms: conduction, convection, evaporation, and radiation critical for infant care.
Apgar Score
- Rapid assessment tool evaluating newborn health post-delivery through appearance, pulse, grimace, activity, and respiration.
- Scores of 7 or higher indicate good overall condition.
Infant of a Diabetic Mother
- Hyperinsulinemia can lead to various complications such as macrosomia, birth injuries, respiratory distress, and metabolic conditions like hypoglycemia.
- Increased bilirubin levels in neonates may arise from excessive RBCs due to maternal diabetes complications.
Neonate Head Assessment
- Caput succedaneum: subcutaneous edema from birth pressure; cephalhematoma: blood collection not crossing suture lines.
- Monitor for more serious complications like subgaleal hemorrhage, which can be life-threatening.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.