Podcast
Questions and Answers
Which component is NOT part of a comprehensive periodontal examination?
Which component is NOT part of a comprehensive periodontal examination?
- Visual inspection
- Bleeding on probing
- Probing depths
- Assessment of systemic diseases (correct)
What is the primary purpose of scaling and root planing in periodontal therapy?
What is the primary purpose of scaling and root planing in periodontal therapy?
- To promote tissue regeneration
- To remove subgingival calculus (correct)
- To assess microbial activity
- To provide oral hygiene instruction
Which of the following is an example of a surgical periodontal procedure?
Which of the following is an example of a surgical periodontal procedure?
- Scaling and root planing
- Antimicrobial therapy
- Oral hygiene instruction
- Guided tissue regeneration (correct)
How can patient education assist in the management of periodontal disease?
How can patient education assist in the management of periodontal disease?
What does outcomes-based care rely on in the treatment of periodontal diseases?
What does outcomes-based care rely on in the treatment of periodontal diseases?
Which of the following systemic diseases is NOT typically linked to periodontal disease complications?
Which of the following systemic diseases is NOT typically linked to periodontal disease complications?
What is the main role of radiographic images in periodontal examinations?
What is the main role of radiographic images in periodontal examinations?
Which therapeutic approach is aimed specifically at controlling infection during periodontal treatment?
Which therapeutic approach is aimed specifically at controlling infection during periodontal treatment?
What does periodontics primarily focus on?
What does periodontics primarily focus on?
Which of the following bacteria is NOT typically associated with periodontal disease?
Which of the following bacteria is NOT typically associated with periodontal disease?
What is a significant consequence of untreated gingivitis?
What is a significant consequence of untreated gingivitis?
Which clinical sign is characteristic of gingivitis?
Which clinical sign is characteristic of gingivitis?
What is the role of biofilms in periodontal disease?
What is the role of biofilms in periodontal disease?
Which factor is NOT typically associated with the susceptibility to periodontal diseases?
Which factor is NOT typically associated with the susceptibility to periodontal diseases?
What is a primary method for diagnosing periodontal disease?
What is a primary method for diagnosing periodontal disease?
How does chronic periodontitis differ from aggressive periodontitis?
How does chronic periodontitis differ from aggressive periodontitis?
Flashcards
What is Periodontics?
What is Periodontics?
A branch of dentistry that focuses on preventing, diagnosing, and treating gum disease.
What are the supporting structures of teeth?
What are the supporting structures of teeth?
Gingiva, cementum, periodontal ligament, and alveolar bone.
What is Periodontitis?
What is Periodontitis?
A chronic inflammatory disease that destroys the supporting structures of teeth, leading to bone loss and eventual tooth loss.
What factors contribute to periodontal disease?
What factors contribute to periodontal disease?
Signup and view all the flashcards
What is Gingivitis?
What is Gingivitis?
Signup and view all the flashcards
What are periodontal pockets?
What are periodontal pockets?
Signup and view all the flashcards
What is Chronic Periodontitis?
What is Chronic Periodontitis?
Signup and view all the flashcards
What is Aggressive Periodontitis?
What is Aggressive Periodontitis?
Signup and view all the flashcards
What does a comprehensive periodontal exam involve?
What does a comprehensive periodontal exam involve?
Signup and view all the flashcards
What do radiographs show in a periodontal exam?
What do radiographs show in a periodontal exam?
Signup and view all the flashcards
What is periodontal charting?
What is periodontal charting?
Signup and view all the flashcards
What's the goal of non-surgical periodontal therapy?
What's the goal of non-surgical periodontal therapy?
Signup and view all the flashcards
Explain scaling and root planing.
Explain scaling and root planing.
Signup and view all the flashcards
When are surgical periodontal procedures necessary?
When are surgical periodontal procedures necessary?
Signup and view all the flashcards
What is the goal of regenerative procedures?
What is the goal of regenerative procedures?
Signup and view all the flashcards
What does outcomes-based care mean for periodontal treatment?
What does outcomes-based care mean for periodontal treatment?
Signup and view all the flashcards
Study Notes
Introduction to Periodontics
- Periodontics is a specialized branch of dentistry focusing on preventing, diagnosing, and treating diseases affecting tooth supporting structures.
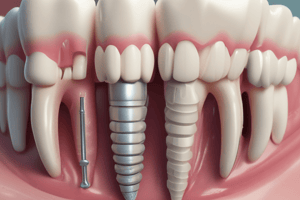
- These structures include gingiva (gums), cementum, periodontal ligament, and alveolar bone.
- Periodontitis is a chronic inflammatory disease affecting the periodontium leading to progressive destruction of tooth supporting structures.
- Preventative care, early detection, and appropriate treatment are crucial for maintaining oral health and preventing tooth loss.
Etiology and Pathogenesis of Periodontal Diseases
- Periodontal disease etiology is multifactorial, involving both host susceptibility and microbial factors.
- Microbial imbalances are key drivers of periodontal inflammation.
- Gram-negative anaerobic bacteria like Porphyromonas gingivalis and Tannerella forsythia are pivotal in periodontal disease initiation and progression.
- Biofilms, complex microbial communities, form on tooth surfaces contributing to infection.
- Host factors (genetics, systemic conditions – diabetes, smoking, hormonal changes, and immunodeficiency) influence periodontal disease susceptibility and progression.
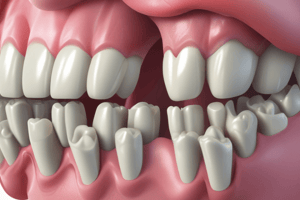
- Gingivitis (gum inflammation) is an early stage of periodontal disease.
- Untreated gingivitis can progress to periodontitis, destroying supporting ligaments and alveolar bone.
Clinical Manifestations of Periodontal Diseases
- Gingivitis presents with red, swollen, and bleeding gums.
- Periodontal pockets form as periodontal ligament and alveolar bone are destroyed, creating spaces between teeth and gums.
- Chronic periodontitis shows slowly progressive attachment and bone loss.
- Aggressive periodontitis is characterized by rapid bone loss.
- Periodontal probing measures pocket depth, indicating disease progression.
- Radiographic images assess bone loss extent.
- Clinical attachment loss (CAL) is a vital indicator of disease progression.
Diagnosis and Evaluation of Periodontal Diseases
- A detailed patient history (medical conditions, oral hygiene habits) is essential.
- Comprehensive periodontal examination includes visual inspection, probing depths, bleeding on probing, and CAL assessment.
- Radiographs evaluate alveolar bone height and bone loss.
- Periodontal charting accurately documents examination findings.
- Diagnostic aids (subgingival plaque analysis, microbial testing, genetic predisposition) assist in specific diagnostics.
Treatment Strategies for Periodontal Diseases
- Non-surgical therapies remove subgingival calculus, plaque, and biofilm.
- Scaling and root planing are crucial for removing hard and soft deposits.
- Oral hygiene instruction (proper brushing, interdental cleaning) is vital for periodontal health maintenance.
- Antimicrobials (systemic or local) control infection with other treatments.
- Surgical approaches are used for advanced periodontitis.
- Regenerative procedures restore lost periodontal tissues.
- Guided tissue regeneration guides tissue regrowth.
- Flap surgery, bone grafting, and guided tissue regeneration are examples of surgical treatments.
- Outcomes-based care evaluates treatments using parameters like probing depth and clinical attachment level.
- Active therapy and maintenance are critical for long-term periodontal health.
Patient Management and Prevention
- Patient education on proper oral hygiene is essential for disease prevention.
- Regular periodontal maintenance visits prevent disease progression.
- Assessing and communicating periodontal disease risks to patients is important.
- Patient motivation for optimal oral hygiene is crucial.
Systemic Connections
- Systemic diseases (diabetes, HIV) influence periodontal treatment response.
- Periodontal disease is linked to systemic issues like cardiovascular disease, respiratory diseases, and pregnancy complications.
- Healthy periodontal tissues are integral to overall health.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.