Podcast
Questions and Answers
What effect does exercise have on arterial blood pressure?
What effect does exercise have on arterial blood pressure?
- It has no effect on arterial blood pressure.
- It typically causes a temporary increase in blood pressure. (correct)
- It decreases arterial blood pressure for all individuals.
- It consistently increases it regardless of individual factors.
Which of the following is a characteristic of primary hypertension?
Which of the following is a characteristic of primary hypertension?
- It often presents without a specific identifiable cause. (correct)
- It is typically a result of renal failure.
- It is caused by excessive salt intake.
- It accounts for 10% of hypertension cases.
What is the primary role of veins in the circulatory system?
What is the primary role of veins in the circulatory system?
- To drain capillary blood and return it to the heart. (correct)
- To store blood and regulate pressure.
- To increase arterial blood pressure during exercise.
- To filter blood and remove waste products.
What happens when blood loss exceeds 20% of total blood volume?
What happens when blood loss exceeds 20% of total blood volume?
Which of the following does NOT affect arterial blood pressure?
Which of the following does NOT affect arterial blood pressure?
What is the correct sequence of impulse conduction in the heart?
What is the correct sequence of impulse conduction in the heart?
Which of the following factors will decrease the heart rate?
Which of the following factors will decrease the heart rate?
The cardiac output can be calculated using which formula?
The cardiac output can be calculated using which formula?
Which type of blood vessel primarily represents resistance vessels?
Which type of blood vessel primarily represents resistance vessels?
During which phase of the cardiac cycle does blood flow from the atria to the ventricles?
During which phase of the cardiac cycle does blood flow from the atria to the ventricles?
What is the average heart rate for adults?
What is the average heart rate for adults?
Which physiological change increases heart rate by 10 beats/min for every degree Celsius rise in temperature?
Which physiological change increases heart rate by 10 beats/min for every degree Celsius rise in temperature?
Which statement regarding the stroke volume is correct?
Which statement regarding the stroke volume is correct?
What is the role of the papillary muscles in the heart?
What is the role of the papillary muscles in the heart?
Which component of the heart is responsible for separating the left atrium from the left ventricle?
Which component of the heart is responsible for separating the left atrium from the left ventricle?
What is the primary function of the systemic circulation?
What is the primary function of the systemic circulation?
Which of the following factors primarily affects the stroke volume?
Which of the following factors primarily affects the stroke volume?
Which statement best describes the atrioventricular valves?
Which statement best describes the atrioventricular valves?
What is the primary purpose of the pericardium surrounding the heart?
What is the primary purpose of the pericardium surrounding the heart?
How does increasing heart rate typically influence cardiac output?
How does increasing heart rate typically influence cardiac output?
Which of the following most directly affects arterial blood pressure?
Which of the following most directly affects arterial blood pressure?
Which of the following is a characteristic of secondary hypertension?
Which of the following is a characteristic of secondary hypertension?
Which factor does NOT directly influence venous return to the heart?
Which factor does NOT directly influence venous return to the heart?
Which statement accurately describes compensatory mechanisms during hemorrhage exceeding 20% of total blood volume?
Which statement accurately describes compensatory mechanisms during hemorrhage exceeding 20% of total blood volume?
What is the primary cause of primary hypertension according to its characteristics?
What is the primary cause of primary hypertension according to its characteristics?
Which of the following best describes shock in medical terms?
Which of the following best describes shock in medical terms?
What is the primary role of the papillary muscles in the heart?
What is the primary role of the papillary muscles in the heart?
Which structure prevents the backflow of blood into the ventricles after it has entered the aorta and pulmonary artery?
Which structure prevents the backflow of blood into the ventricles after it has entered the aorta and pulmonary artery?
In which part of the circulation does deoxygenated blood enter the heart?
In which part of the circulation does deoxygenated blood enter the heart?
Which statement best describes the systemic circulation route?
Which statement best describes the systemic circulation route?
What is the function of the pericardium surrounding the heart?
What is the function of the pericardium surrounding the heart?
Which valve is located between the right atrium and right ventricle?
Which valve is located between the right atrium and right ventricle?
What role do chordae tendineae play in the heart's function?
What role do chordae tendineae play in the heart's function?
During ventricular contraction, what is prevented by the atrioventricular valves?
During ventricular contraction, what is prevented by the atrioventricular valves?
Which structure initiates the electrical impulse that causes the heart to beat?
Which structure initiates the electrical impulse that causes the heart to beat?
What is the effect of sympathetic stimulation on heart rate during stressful situations?
What is the effect of sympathetic stimulation on heart rate during stressful situations?
What is the average duration of one cardiac cycle?
What is the average duration of one cardiac cycle?
How does a fever affect heart rate, based on temperature changes?
How does a fever affect heart rate, based on temperature changes?
What is the stroke volume of the heart approximately in adults?
What is the stroke volume of the heart approximately in adults?
Which type of blood vessel is primarily known as exchange vessels?
Which type of blood vessel is primarily known as exchange vessels?
What happens during ventricular systole?
What happens during ventricular systole?
Which hormone is known to increase heart rate?
Which hormone is known to increase heart rate?
Flashcards
Arterial blood pressure function
Arterial blood pressure function
The force pushing blood through circulation, ensuring adequate tissue perfusion and capillary filtration.
Hypertension
Hypertension
High blood pressure, typically defined as a blood pressure reading above 140/90. Different classifications exist based on age groups.
Primary Hypertension
Primary Hypertension
90% of cases, occurs without an identifiable cause, characterized by narrowed arterioles.
Venous return
Venous return
Signup and view all the flashcards
Hemorrhage
Hemorrhage
Signup and view all the flashcards
Heart Chambers
Heart Chambers
Signup and view all the flashcards
Heart Valves
Heart Valves
Signup and view all the flashcards
Atrioventricular Valves
Atrioventricular Valves
Signup and view all the flashcards
Papillary Muscles
Papillary Muscles
Signup and view all the flashcards
Systemic Circulation
Systemic Circulation
Signup and view all the flashcards
Pulmonary Circulation
Pulmonary Circulation
Signup and view all the flashcards
Blood Flow Direction
Blood Flow Direction
Signup and view all the flashcards
Heart Function
Heart Function
Signup and view all the flashcards
Heart Rate
Heart Rate
Signup and view all the flashcards
Sino-atrial node (SA node)
Sino-atrial node (SA node)
Signup and view all the flashcards
Cardiac Cycle
Cardiac Cycle
Signup and view all the flashcards
Cardiac Output
Cardiac Output
Signup and view all the flashcards
Stroke Volume
Stroke Volume
Signup and view all the flashcards
Sympathetic Stimulation
Sympathetic Stimulation
Signup and view all the flashcards
Parasympathetic Stimulation
Parasympathetic Stimulation
Signup and view all the flashcards
Blood Vessel Types
Blood Vessel Types
Signup and view all the flashcards
Pericardium
Pericardium
Signup and view all the flashcards
Atrioventricular (A-V) Valves
Atrioventricular (A-V) Valves
Signup and view all the flashcards
Aortic Valve Function
Aortic Valve Function
Signup and view all the flashcards
Pulmonary Valve Function
Pulmonary Valve Function
Signup and view all the flashcards
Atrium Function
Atrium Function
Signup and view all the flashcards
What causes the heart to beat?
What causes the heart to beat?
Signup and view all the flashcards
How does exercise affect heart rate?
How does exercise affect heart rate?
Signup and view all the flashcards
What increases cardiac output?
What increases cardiac output?
Signup and view all the flashcards
What are windkessel vessels?
What are windkessel vessels?
Signup and view all the flashcards
Resistance vessels
Resistance vessels
Signup and view all the flashcards
What type of blood vessel is the aorta?
What type of blood vessel is the aorta?
Signup and view all the flashcards
Arterial Blood Pressure
Arterial Blood Pressure
Signup and view all the flashcards
What causes primary hypertension?
What causes primary hypertension?
Signup and view all the flashcards
What are the functions of veins?
What are the functions of veins?
Signup and view all the flashcards
What is the difference between external and internal hemorrhage?
What is the difference between external and internal hemorrhage?
Signup and view all the flashcards
Study Notes
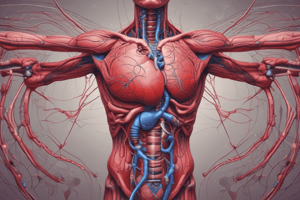
Introduction to Cardiovascular Physiology
- Presented by Dr. Sherif Diaaeldin
- Assistant Professor of Physiology
Functional Anatomy of the Heart
- The heart is a hollow muscular organ
- Surrounded by a connective tissue sac called the pericardium
- The pericardium protects the heart and minimizes friction during contraction
- The heart wall is made of cardiac muscle
- Divided into right and left halves
- Each half consists of one atrium and one ventricle
Heart Valves
- The right atrium is separated from the right ventricle by the tricuspid valve
- The left atrium is separated from the left ventricle by the bicuspid (or mitral) valve
- Both valves are called atrioventricular (A-V) valves
- In the ventricles, there are papillary muscles with tendons (chordae tendineae)
- These are attached to the A-V valves to prevent everting into the atria during ventricular contraction
Function of Heart Valves
- Allow blood flow in one direction only
Divisions of the Circulation
- Systemic Circulation:
- Begins at the left ventricle
- Aorta
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
- Superior and inferior vena cava
- Right atrium
- Pulmonary Circulation:
- Begins at the right ventricle
- Pulmonary artery
- Lungs
- Pulmonary capillaries
- Pulmonary veins (4 in number)
- Left atrium
Functions of the Atria and Ventricles
- Atria are entryways for ventricles
- Ventricles pump blood to the whole body
- The aorta pumps oxygenated blood throughout the body
- Pulmonary veins carry oxygenated blood to the heart from the lungs
- Pulmonary artery carries deoxygenated blood to the lungs
Mechanism of Heart Beating
- Heart rate: 60-90 beats/min (average 72 beats/min in adults)
- Impulse originates at the sino-atrial (SA) node (in the right atrium)
- SA node contraction of atria
- Impulse travels to the atrioventricular (AV) node
- Impulse travels to the ventricles through the His-Purkinje system
- This causes ventricular contraction
Factors Affecting Heart Rate
- Increasing Heart Rate:
- Sympathetic stimulation (e.g., fear, stress)
- Exercise
- Increased body temperature (e.g., fever)
- Thyroxin and adrenaline hormones
- Decreasing Heart Rate:
- Parasympathetic stimulation
- Sleep
- Decreased body temperature
- Drugs (e.g., beta blockers)
Normal Heart Sounds
- S1 ("Lubb"): Sound of mitral and tricuspid valve closure, start of systole, heard loudest at the apex of the heart
- S2 ("Dubb"): Sound of pulmonic and aortic valve closure, end of systole, heard loudest at the base of the heart
The Cardiac Cycle
- Consists of one systole-diastole sequence
- Duration is about 0.8 seconds
- Atrial systole: Blood flows from the atria to the ventricles
- Ventricular systole: Blood flows from the ventricles (to the lungs on the right side and to the rest of the body on the left side)
- Atrial diastole: Atria receive blood from the superior and inferior vena cava
- Ventricular diastole: Ventricles fill with blood from the atria
The Cardiac Output
- Amount of blood pumped by each ventricle per minute
- Approximately 5.5 liters per minute
- Stroke volume: Amount of blood pumped by each ventricle per beat (approximately 80 ml/beat)
- Cardiac output = heart rate x stroke volume
Factors Affecting Cardiac Output
- Sympathetic stimulation increases cardiac output
- Parasympathetic stimulation decreases cardiac output
- Catecholamines and thyroxin increase cardiac output
Blood Vessels
- Types of blood vessels :
- Elastic arteries (e.g., aorta)
- Muscular arteries (e.g., large arteries)
- Resistance vessels (e.g., arterioles)
- Exchange vessels (e.g., capillaries)
Arterial Blood Pressure
- The force that pushes blood through the circulatory system
- Ensures adequate tissue perfusion
- Responsible for capillary filtration
Determinants of Arterial Blood Pressure
- Age
- Sex
- Diurnal variations
- Sleep
- Emotions
- Exercise
- Gravity
Hypertension in Man
- High blood pressure
- Types: Primary (essential) or Secondary
- Primary (90%): Often no identifiable cause, characterized by narrowed arterioles
- Secondary (10%): Caused by other health conditions (e.g., kidney failure, endocrine disorders)
- Predisposing factors: Smoking, obesity, excess salt intake
Functions of Veins
- Passageways for blood flow to the heart, crucial for circulation
- Drain capillary blood to the heart
- Blood returned to the heart determines venous return (equal to cardiac output)
Shock & Haemorrhage
- Hemorrhage: Blood loss from the cardiovascular system (external or internal)
- Shock: Decreased tissue perfusion due to inadequate oxygen and nutrient delivery to cells (blood loss > 20% of total volume)
- Compensatory mechanisms: Increase arterial blood pressure and cardiac output (temporary measures) to restore blood volume (delayed measures)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.