Podcast
Questions and Answers
What is the primary nerve that runs below the 12th rib?
What is the primary nerve that runs below the 12th rib?
- Thoracic nerve
- Subcostal nerve (correct)
- Abdominal nerve
- Intercostal nerve
What is the most common cause of intercostal neuralgia?
What is the most common cause of intercostal neuralgia?
- Postural malalignment
- Muscle strain
- Shingles
- Compression (correct)
What is the typical description of intercostal neuralgia pain?
What is the typical description of intercostal neuralgia pain?
- Dull and aching
- Cramping and sore
- Sharp, shooting, searing, burning, stabbing, tender, gnawing (correct)
- Numb and tingling
Where do the intercostal nerves travel?
Where do the intercostal nerves travel?
What is the result of the reactivation of the dormant Chicken Pox Virus?
What is the result of the reactivation of the dormant Chicken Pox Virus?
What is the typical effect of light touch or movement over the affected area?
What is the typical effect of light touch or movement over the affected area?
What is the commonly observed facial expression in intercostal neuralgia?
What is the commonly observed facial expression in intercostal neuralgia?
Where is the pain of intercostal neuralgia most prominently felt?
Where is the pain of intercostal neuralgia most prominently felt?
What is a common symptom of shingles?
What is a common symptom of shingles?
What is a potential complication of shingles?
What is a potential complication of shingles?
What should a therapist do when treating a client with shingles?
What should a therapist do when treating a client with shingles?
What is a contraindication for massage in the acute stage of shingles?
What is a contraindication for massage in the acute stage of shingles?
What is a treatment goal for a client with shingles in the chronic stage?
What is a treatment goal for a client with shingles in the chronic stage?
What is a consideration for frequency of treatment for a client with shingles?
What is a consideration for frequency of treatment for a client with shingles?
What is a remedial exercise for a client with shingles in the acute stage?
What is a remedial exercise for a client with shingles in the acute stage?
What is a potential cause of neuralgia?
What is a potential cause of neuralgia?
What is a position that may be appropriate for a client with shingles?
What is a position that may be appropriate for a client with shingles?
What is a goal of drainage techniques in the treatment of shingles?
What is a goal of drainage techniques in the treatment of shingles?
What is the composition of the sciatic nerve?
What is the composition of the sciatic nerve?
What is the autonomic function of the leg related to?
What is the autonomic function of the leg related to?
What is the path of the sciatic nerve after exiting the sciatic foramen?
What is the path of the sciatic nerve after exiting the sciatic foramen?
What is the motor innervation of the sciatic nerve related to?
What is the motor innervation of the sciatic nerve related to?
Which muscle is innervated by the obturator nerve?
Which muscle is innervated by the obturator nerve?
What is the result of a high sciatic nerve lesion in terms of sensory loss?
What is the result of a high sciatic nerve lesion in terms of sensory loss?
What is the path of the tibial nerve after forming the neurovascular bundle?
What is the path of the tibial nerve after forming the neurovascular bundle?
What is the final destination of the tibial nerve?
What is the final destination of the tibial nerve?
Which muscle is responsible for leg and foot flexion?
Which muscle is responsible for leg and foot flexion?
Which nerve branch supplies sensation to the anterolateral surface of the lower leg and dorsum of the foot, excluding the toes?
Which nerve branch supplies sensation to the anterolateral surface of the lower leg and dorsum of the foot, excluding the toes?
Which muscle is innervated by the femoral nerve?
Which muscle is innervated by the femoral nerve?
What is the result of a high sciatic nerve injury?
What is the result of a high sciatic nerve injury?
What is the function of the Sural nerve?
What is the function of the Sural nerve?
Which nerve branch causes altered sensation only in the web space between the 1st and 2nd toes?
Which nerve branch causes altered sensation only in the web space between the 1st and 2nd toes?
What is the characteristic gait of a person with a common peroneal lesion?
What is the characteristic gait of a person with a common peroneal lesion?
Which muscle is responsible for leg and foot extension?
Which muscle is responsible for leg and foot extension?
What is the result of a tibial branch injury?
What is the result of a tibial branch injury?
Which nerve branch is responsible for supplying sensation to the medial side of the leg, medial malleolus?
Which nerve branch is responsible for supplying sensation to the medial side of the leg, medial malleolus?
What type of splint is required to protect the toes from dragging injuries on the ground?
What type of splint is required to protect the toes from dragging injuries on the ground?
Which nerve is responsible for the loss of sensation to the plantar surface of the foot in the case of a complete lesion?
Which nerve is responsible for the loss of sensation to the plantar surface of the foot in the case of a complete lesion?
What is the result of an unopposed hyperextension contracture of the MTP joints?
What is the result of an unopposed hyperextension contracture of the MTP joints?
What is the cause of massive edema in the case of an autonomic nerve lesion?
What is the cause of massive edema in the case of an autonomic nerve lesion?
What is the result of a common peroneal nerve lesion?
What is the result of a common peroneal nerve lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
What is the result of a tibial branch injury?
What is the result of a tibial branch injury?
What is the cause of Causalgia and Reflex Sympathetic Dystrophy?
What is the cause of Causalgia and Reflex Sympathetic Dystrophy?
What is the minimum time frame for which massage is contraindicated post-surgical repair?
What is the minimum time frame for which massage is contraindicated post-surgical repair?
What should a therapist do if signs of ulceration or infection appear during treatment?
What should a therapist do if signs of ulceration or infection appear during treatment?
What is the purpose of shorter treatments in the early stages of a nerve lesion?
What is the purpose of shorter treatments in the early stages of a nerve lesion?
What happens to de-innervated muscle tissue after 2 years?
What happens to de-innervated muscle tissue after 2 years?
What should a therapist avoid when working with a paralyzed or paretic muscle tissue?
What should a therapist avoid when working with a paralyzed or paretic muscle tissue?
What should a therapist do before removing a brace or splint?
What should a therapist do before removing a brace or splint?
What is the purpose of modifying hydrotherapy for a client with loss or altered sensation or autonomic dysfunction?
What is the purpose of modifying hydrotherapy for a client with loss or altered sensation or autonomic dysfunction?
What determines the prognosis of a nerve lesion?
What determines the prognosis of a nerve lesion?
What is a common cause of compartment syndromes?
What is a common cause of compartment syndromes?
What is the aim of treatment in regenerating nerve lesions?
What is the aim of treatment in regenerating nerve lesions?
When should modified hydrotherapy be applied in regenerating nerve lesions?
When should modified hydrotherapy be applied in regenerating nerve lesions?
What is the focus of treatment in permanent nerve lesions?
What is the focus of treatment in permanent nerve lesions?
What is the purpose of segmental stretching in regenerating nerve lesions?
What is the purpose of segmental stretching in regenerating nerve lesions?
What is the goal of elevation in regenerating nerve lesions?
What is the goal of elevation in regenerating nerve lesions?
What is the purpose of light, stimulating tapotement in regenerating nerve lesions?
What is the purpose of light, stimulating tapotement in regenerating nerve lesions?
What is the purpose of modified fascial techniques in regenerating nerve lesions?
What is the purpose of modified fascial techniques in regenerating nerve lesions?
What is the goal of motor re-education in regenerating nerve lesions?
What is the goal of motor re-education in regenerating nerve lesions?
What is the purpose of rhythmic mobilization techniques in regenerating nerve lesions?
What is the purpose of rhythmic mobilization techniques in regenerating nerve lesions?
What is the origin of the Sciatic Nerve?
What is the origin of the Sciatic Nerve?
What is the action of the Piriformis muscle when the hip is flexed above 90 degrees?
What is the action of the Piriformis muscle when the hip is flexed above 90 degrees?
What percentage of the population has peroneal fibres passing through the Piriformis?
What percentage of the population has peroneal fibres passing through the Piriformis?
What is the action of the Piriformis muscle when the hip is in neutral or extension?
What is the action of the Piriformis muscle when the hip is in neutral or extension?
Where does the Piriformis muscle attach to the femur?
Where does the Piriformis muscle attach to the femur?
What is the primary cause of Piriformis syndrome?
What is the primary cause of Piriformis syndrome?
What is the result of long-term irritation of the Sciatic nerve?
What is the result of long-term irritation of the Sciatic nerve?
What is a common symptom of Piriformis syndrome?
What is a common symptom of Piriformis syndrome?
What is a distinction between Piriformis syndrome and a trigger point referral of the Piriformis muscle?
What is a distinction between Piriformis syndrome and a trigger point referral of the Piriformis muscle?
What is a potential cause of sciatic-like pain?
What is a potential cause of sciatic-like pain?
Why might a doctor refer to Piriformis compression as sciatica?
Why might a doctor refer to Piriformis compression as sciatica?
What is the thickness of the sciatic nerve?
What is the thickness of the sciatic nerve?
What innervates the autonomic function of the leg?
What innervates the autonomic function of the leg?
What is the motor innervation of the sciatic nerve related to?
What is the motor innervation of the sciatic nerve related to?
Which muscle is not innervated by the sciatic nerve?
Which muscle is not innervated by the sciatic nerve?
What is the result of a high sciatic nerve lesion in terms of sensory loss?
What is the result of a high sciatic nerve lesion in terms of sensory loss?
What forms the neurovascular bundle with the tibial nerve?
What forms the neurovascular bundle with the tibial nerve?
What is the final destination of the tibial nerve?
What is the final destination of the tibial nerve?
Which muscle is innervated by the obturator nerve?
Which muscle is innervated by the obturator nerve?
Which muscle is responsible for leg and foot flexion?
Which muscle is responsible for leg and foot flexion?
What is the result of a high sciatic nerve injury?
What is the result of a high sciatic nerve injury?
Which nerve branch supplies sensation to the lateral corner of the leg, lateral foot, and 5th toe?
Which nerve branch supplies sensation to the lateral corner of the leg, lateral foot, and 5th toe?
What is the characteristic gait of a person with a common peroneal lesion?
What is the characteristic gait of a person with a common peroneal lesion?
Which muscle is responsible for leg and foot extension?
Which muscle is responsible for leg and foot extension?
What is the result of a tibial branch injury?
What is the result of a tibial branch injury?
Which nerve branch causes altered sensation only in the web space between the 1st and 2nd toes?
Which nerve branch causes altered sensation only in the web space between the 1st and 2nd toes?
What type of splint is required to protect the toes from dragging injuries on the ground?
What type of splint is required to protect the toes from dragging injuries on the ground?
Which nerve is responsible for the loss of sensation to the plantar surface of the foot in the case of a complete lesion?
Which nerve is responsible for the loss of sensation to the plantar surface of the foot in the case of a complete lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
When can light stimulating tapotement to flaccid tissue be performed during nerve lesion treatment?
When can light stimulating tapotement to flaccid tissue be performed during nerve lesion treatment?
What is the focus of treatment in permanent nerve lesions?
What is the focus of treatment in permanent nerve lesions?
Why is massage contraindicated for at least three weeks post-surgical repair?
Why is massage contraindicated for at least three weeks post-surgical repair?
What should a therapist do if signs of ulceration or infection appear during treatment?
What should a therapist do if signs of ulceration or infection appear during treatment?
Why are shorter treatments more effective in the early stages of nerve lesion treatment?
Why are shorter treatments more effective in the early stages of nerve lesion treatment?
What is the result of an unopposed hyperextension contracture of the MTP joints?
What is the result of an unopposed hyperextension contracture of the MTP joints?
What happens to de-innervated muscle tissue after 2 years?
What happens to de-innervated muscle tissue after 2 years?
What should a therapist avoid when working with a paralyzed or paretic muscle tissue?
What should a therapist avoid when working with a paralyzed or paretic muscle tissue?
What is the cause of massive edema in the case of an autonomic nerve lesion?
What is the cause of massive edema in the case of an autonomic nerve lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
What is the risk of injury to the foot if the tibial nerve is affected with a complete lesion?
Before removing a brace or splint, what should a therapist do?
Before removing a brace or splint, what should a therapist do?
What is the goal of elevation and drainage techniques in the treatment of nerve lesions?
What is the goal of elevation and drainage techniques in the treatment of nerve lesions?
What is the result of a common peroneal nerve lesion?
What is the result of a common peroneal nerve lesion?
What is the cause of Causalgia and Reflex Sympathetic Dystrophy?
What is the cause of Causalgia and Reflex Sympathetic Dystrophy?
What is the aim of treatment for a client with a nerve lesion?
What is the aim of treatment for a client with a nerve lesion?
What is the purpose of modified fascial techniques in the treatment of nerve lesions?
What is the purpose of modified fascial techniques in the treatment of nerve lesions?
What is the risk of injuries to the foot if the client has a complete lesion of the tibial nerve?
What is the risk of injuries to the foot if the client has a complete lesion of the tibial nerve?
What is the goal of segmental stretching in the treatment of nerve lesions?
What is the goal of segmental stretching in the treatment of nerve lesions?
Study Notes
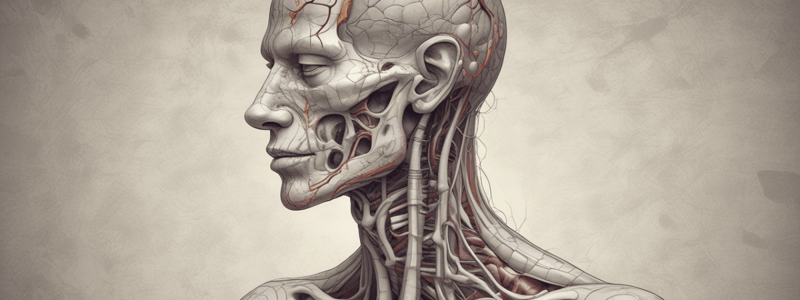
Intercostal Neuralgia
- Intercostal neuralgia is a type of neuralgia that occurs along the course of an intercostal nerve.
Anatomy
- Intercostal nerves travel as a neurovascular bundle with the intercostal artery and vein.
- Nerves 1-6 extend from the spine to the sternum.
- Nerves 7-11 run from the spine to the abdomen.
- The 12th thoracic nerve, or subcostal nerve, runs below the 12th rib.
- Intercostal nerves run between the internal and innermost intercostal muscles along the costal groove of the inferior part of the rib.
Signs and Symptoms
- Symptoms can be acute or chronic in nature.
- Pain is described as sharp, shooting, searing, burning, stabbing, or tender in the rib cage area that wraps around the chest wall like a band.
- Antalgic facial expression and posture are common.
- Breathing is short and shallow.
- Pain is felt most prominently where cutaneous branches of the nerve emerge.
- Pain is aggravated by light touch or movement over the area.
Causes
- Compression is the most common cause, which can be due to:
- Rib subluxation
- Trauma (rib fracture, bruise)
- Muscle spasm
- Surgical scarring
- Postural malalignment (e.g., scoliosis, pregnancy)
- Poorly administered high velocity adjustment
- Complication of Shingles: Post-Herpetic Neuralgia, which occurs when the dormant Chicken Pox Virus reactivates in the dorsal root ganglion of intercostal nerves.
- Diabetes, which can cause metabolic changes leading to neuralgia.
Assessment Case History
- General Health (history of chicken pox, shingles, diabetes, respiratory conditions, cardiac conditions, osteoporosis)
- Onset and location of neuralgia
- Description of pain and symptoms
- Medical history (diagnoses, medications)
- History of thoracic surgery or rib fractures
- Presence of thoracic postural deviations
- Chiropractic adjustments
- Sleeping position
- Other treatments
Treatment
- Treatment varies widely depending on the cause of the neuralgia, health of the client, and potential stage of inflammation.
- Acute treatment:
- Avoid excessive movement of the client.
- Increase relaxation with slow, predictable, indirect techniques.
- Client may need to be positioned in seated.
- Drainage above and around the area may reduce edema, pain, and SNS firing, and remove metabolic waste.
- Subacute treatment:
- Frequent position changes may be necessary.
- Light pressure and gentle kneading over the area may be tolerated to increase local circulation and reduce intercostal muscle spasms.
- Drainage on-site may begin.
- Encourage and teach full diaphragmatic breathing to return proper movement to thorax.
- Chronic treatment:
- May lay client in prone, supine, or side lying for best access.
- Full DDB is encouraged.
- Fascial, effleurage, petrissage, friction (if necessary) to scar tissue.
- Reduce hypertonicity and trigger points in neck, shoulders, and muscles of respiration.
- Abdominal massage with diaphragm release.
- Rib raking, thoracic mobilizations, and joint play to maintain thoracic mobility.
- Treat postural dysfunctions.
- Hydrotherapy may include warm to hot, or contrast applications.
Contraindications
- Acute: Massage over the trigger zone or affected area is contraindicated.
- Avoid rocking or shaking techniques.
- Chronic: No rib springing if osteoporosis is present.
Frequency and Remedial Exercise
- Initially treat for 1⁄2 an hour, 2-3 times per week.
- Progress to weekly, 2x/month, and then monthly treatment.
- Remedial exercise and self-care:
- Acute: Relaxation techniques.
- Subacute: Full diaphragmatic breathing, AF ROM to neck and shoulders, gentle stretches (Clapp’s crawl), and return to ADL within pain tolerance.
- Chronic: Continue with breathing exercises, Clapp’s crawl, and self-mobilizations with hands.
Medical Treatment
- NSAID’s can be taken to alleviate pain (outside of RMT scope of practice).
- Nerve block injections.
- In extreme cases: neurectomy.
Prognosis
- Recovery should be within weeks if the cause can be removed.
- Respiratory or postural causes may take months.
- Metabolic neuropathies and post-herpetic neuralgia may continue for 2 years or more.
Lower Limb Nerve Lesions
Sciatic Nerve
- Composed of two nerves: tibial and common peroneal nerves
- Innervated from nerve roots L4-S3
- Autonomic function of the leg follows the tibial nerve
- Exits the sciatic foramen, travels deep to piriformis, and emerges between the ischial tuberosity and greater trochanter
- Splits into two branches at the popliteal fossa
Motor Innervation of Sciatic Nerve
- Hip extensor and knee flexor group:
- Semitendinosus
- Semimembranosis
- 1⁄2 Adductor Magnus (hamstring portion)
- Other 1⁄2 (adductor portion) innervated by the Obturator nerve
Sensory Innervation of Sciatic Nerve
- No sensory loss in the back of the thigh due to a high sciatic nerve lesion
- Sensation to the back of the thigh comes from the Posterior Cutaneous Nerve
Tibial Nerve
- Joined by the tibial artery and vein at the popliteal fossa to form the neurovascular bundle
- Travels between the heads of gastrocnemius and comes around behind the medial malleolus
- Splits into two branches to supply the plantar surface of the foot
Motor Innervation of Tibial Nerve
- Leg and foot flexors:
- Biceps Femoris, Long head
- Gastrocnemius
- Plantaris
- Popliteus
- Soleus
- Tibialis Posterior
- Flexor Digitorum Longus & Brevis
- Flexor Hallucis Longus & Brevis
- Abductor & Adductor Hallicus
- Abductor Digiti Minimi
- Lumbricals & Interossei
Sensory Innervation of Tibial Nerve
- Affects sensory innervation to the posterior leg, heel, sole of the foot, including the toes
Common Peroneal Nerve
- Separates from the tibial branch in the upper popliteal fossa
- Wraps around the fibular head and neck and then into the deep and superficial branches
Motor Innervation of Common Peroneal Nerve
- Leg and foot extensors:
- Biceps Femoris, Short head
- Extensor Digitorum Longus & Brevis
- Peroneus Longus, Brevis, & Tertius
- Tibialis Anterior
- Extensor hallucis Longus & Brevis
Sensory Innervation of Common Peroneal Nerve
- Superficial branch: alters sensation to the anterolateral surface of the lower leg, and dorsum of the foot, excluding the toes
- Deep branch: causes altered sensation only in the web space between the 1st and 2nd toes
Sural Nerve
- Composed of branches of both the tibial and common peroneal nerves
- Supplies sensation to the lateral corner of the leg, lateral foot, and 5th toe
Femoral Nerve
- Emerges anteriorly around the lateral border of Psoas and enters the femoral triangle alongside the femoral artery
- Divides into branches that innervate iliopsoas, Sartorius, pectineus, and the quadriceps
Saphenous Nerve
- Supplies sensation to the medial side of the leg, medial malleolus
- Branches off from the femoral nerve
Signs and Symptoms
- Depend on which area or branch of the sciatic nerve is affected
- High sciatic nerve injury: complete loss of lower leg and foot movement, loss of lower leg sensation, muscle wasting of the hamstrings
- Tibial branch: wasting of the posterior leg and foot intrinsics
- Common peroneal branch: loss of dorsi flexion, wasting of the anterior leg
- Steppage gait or “foot slap”: type of ataxic gait resulting from complete sciatic lesion or common peroneal lesion
Sciatic Nerve Lesions
- Causes of sciatic nerve lesions: fractures to pelvis or femur, contusions to gluteals, hip dislocations, surgeries, lacerations to gluteals or hamstrings, injections in gluteal region, injuries to mother during childbirth
Tibial Nerve Lesions
- Causes of tibial nerve lesions: knee dislocations, fracture of the tibia, contusions/lacerations of the popliteal fossa, excessive knee flexion, severe sprains, long-term tarsal tunnel syndrome
Common Peroneal Nerve Lesions
- Causes of common peroneal nerve lesions: knee dislocations, fracture of the fibula, lacerations and contusions to the anterolateral leg, overly tight casts, compartment syndromes, crush injuries to the anterior leg
Assessment and Treatment
- Palpation and observation: gait analysis, strength testing, contracture, muscle wasting, edema; sensory testing of the anterior leg, web space between the 1st and 2nd toe, and heel of the foot
- Aims of treatment: decrease SNS firing and pain, decrease hypertonicity and trigger points, prevent contracture, decrease edema, maintain health of de-innervated tissue, maintain joint health, increase sensory and motor return, address compensation
Techniques for Regenerating Nerve Lesions
- Prone and sidelying positioning
- Elevation to assist in drainage
- Modified hydrotherapy to reduce edema
- Light, segmental massage and stabilization of tissue around the injury site
- Treatment of unaffected muscles with petrissage and trigger point therapy
- Segmental stretching to prevent traction on healing nerves
Techniques for Permanent Nerve Lesions
- Avoid undue pressure on reddened or fragile tissue
- Modified hydrotherapy or contraindication
- Focus on general tissue and joint health, injury prevention, maintaining circulation, and techniques for recurrent edema, compensatory issues, stress reduction, and emotional support
Contraindications and Precautions
- Massage is contraindicated for at least three weeks post-surgical repair
- Avoid traction on the nerve, introducing infection, or removing brace or splint without physician approval
- Modify hydrotherapy for loss/altered sensation or autonomic dysfunction
- Avoid deep or specific techniques on paralyzed or paretic muscle tissue
- Avoid grasping flaccid tissue to move or hold the limb
Frequency and Prognosis
- Early stages: shorter treatments (45 minutes) 2-3 times per week
- Permanent lesions: longer treatments spaced further apart (weekly to monthly)
- Prognosis varies depending on the level of the lesion, whether it is partial or complete, and whether it is regenerating or permanent
Piriformis Syndrome
- Compression of the Sciatic nerve by hypertonicity, spasming, or contracture of the Piriformis muscle causes sharp, burning, shooting pain and/or numbness and tingling in the buttock and down the distribution of the sciatic nerve.
- Compression site determines the distribution of pain and symptoms.
Causes of Sciatic Nerve Compression
- Herniated discs and osteophytes can compress the sciatic nerve, particularly at the L4-L5 level.
- Tight piriformis muscle can compress the sciatic nerve.
Differential Diagnosis
- SI joint/SI joint dysfunction, strains to the gluteals, and trigger points can mimic sciatic-like pain.
- Trigger points in the piriformis muscle can cause displacement and dysfunction of the SI joint.
True Sciatica
- Result of long-term irritation of the sciatic nerve resulting in inflammation of the nerve itself.
Anatomy of Piriformis Muscle
- Origin: Anterior Sacrum from S1-S4
- Insertion: Superior medial Border of Greater Trochanter of femur
- Actions:
- Lateral rotator when the hip is in neutral or extension
- Horizontal abductor when the hip is flexed to 90 degrees
- Medial rotator when the hip is flexed above 90 degrees
- Resists against medial rotation during walking or running (stabilizer)
- Assists in holding the femur into the acetabulum
Anatomy of Sciatic Nerve
- Originates from L4-S3 lumbo-sacral plexus
- Passes through the greater sciatic foramen
- Usually, the tibial and peroneal portions pass deep to the piriformis
- Cadaver variants:
- 88% of the population have tibial and peroneal fibres passing deep to the piriformis
- 11% of the population have peroneal fibres passing through the piriformis
Anatomy of the Sciatic Nerve
- The sciatic nerve is the largest, longest, and thickest nerve in the body, about the thickness of a thumb.
- Composed of two nerves: tibial and common peroneal nerves, encased in a single sheath until they divide at the knee.
- Innervated from nerve roots L4-S3.
- Autonomic function of the leg follows the tibial nerve.
Sciatic Nerve Pathway
- Exits the sciatic foramen and travels deep to piriformis, exiting the gluteal region between the ischial tuberosity and the greater trochanter.
- Runs down the hamstrings, splitting just proximal to the popliteal fossa, with each nerve taking a separate path down the leg to the foot.
Motor Innervation of the Sciatic Nerve
- Hip extensor and knee flexor group:
- Semitendinosus
- Semimembranosis
- 1⁄2 Adductor Magnus (hamstring portion)
- The other 1⁄2 (adductor portion) is innervated by the Obturator nerve.
Sensory Innervation of the Sciatic Nerve
- There is no sensory loss in the back of the thigh due to a high sciatic nerve lesion.
- Sensation to the back of the thigh comes from the Posterior Cutaneous Nerve.
Tibial Nerve
- Joined by the tibial artery and vein at the popliteal fossa to form the neurovascular bundle.
- Travels between the heads of gastrocnemius and comes around behind the medial malleolus.
- Splits into two branches to supply the plantar surface of the foot.
Motor Innervation of the Tibial Nerve
- Leg and foot flexors:
- Biceps Femoris, Long head
- Gastrocnemius
- Plantaris
- Popliteus
- Soleus
- Tibialis Posterior
- Flexor Digitorum Longus & Brevis
- Flexor Hallucis Longus & Brevis
- Abductor & Adductor Hallucis
- Abductor Digiti Minimi
- Lumbricals & Interossei
Common Peroneal Nerve
- Separates from the tibial branch in the upper popliteal fossa.
- Wraps around the fibular head and neck and then into the deep and superficial branches.
Motor Innervation of the Common Peroneal Nerve
- Leg and foot extensors:
- Biceps Femoris, Short head
- Extensor Digitorum Longus & Brevis
- Peroneus Longus, Brevis, & Tertius
- Tibialis Anterior
- Extensor hallucis Longus & Brevis
Sural Nerve
- Composed of branches of both the tibal and common peroneal nerves.
- Supplies sensation only to the lateral corner of the leg, lateral foot, and 5th toe.
Femoral Nerve
- Emerges anteriorly around the lateral border of Psoas and enters the femoral triangle alongside the femoral artery.
- Divides into branches that innervate iliopsoas, Sartorius, pectineus, and the quadriceps.
Saphenous Nerve
- Supplies sensation to the medial side of the leg, medial malleolus, and branches off from the femoral nerve.
Signs and Symptoms of Sciatic Nerve Lesions
- Depend on which area or branch of the sciatic nerve is affected.
- High sciatic nerve injury:
- Complete loss of lower leg and foot movement
- Loss of lower leg sensation
- Muscle wasting of the Hamstrings
- Tibial branch:
- Wasting of the posterior leg and foot intrinsics
- Common peroneal branch:
- Loss of dorsi flexion, wasting of the anterior leg
- Steppage Gait or “foot slap”:
- Type of ataxic gait resulting from a complete sciatic lesion or with a common peroneal lesion.
Causes of Sciatic Nerve Lesions
- Fractures to pelvis or femur
- Contusions to the gluteals
- Hip Dislocations
- Surgeries, lacerations to gluteals or hamstrings
- Injections in gluteal region
- Injuries to mother during childbirth
Assessment and Treatment of Sciatic Nerve Lesions
- Palpation and Observation:
- Gait analysis for foot drop and steppage gait, dorsi and or plantar flexion strength testing, contracture, muscle wasting, edema, and splint use.
- Sensory testing of the anterior leg, web space between the 1st and 2nd toe, and heel of the foot.
- Palpation of the leg musculature for wasting and contracture.
- Aims of Treatment:
- Decrease SNS firing and pain
- Decrease hypertonicity and trigger points on unaffected muscles
- Prevent contracture from unopposed muscles
- Decrease edema
- Maintain health of de-innervated tissue
- Maintain joint health
- Increase sensory and motor return
- Address compensation
Techniques for Sciatic Nerve Lesions
- Choice of techniques depends on whether the lesion is regenerating or permanent.
- Regenerating Nerve Lesion:
- Treatment will vary depending on whether the lesion is complete or partial and the stage of regeneration.
- Modified hydrotherapy may be applied to reduce edema.
- Light, segmental massage and stablization of the tissue around the injury site to prevent drag on the healing nerve.
- Treat unaffected muscles with careful petrissage and trigger point therapy.
- Permanent Nerve Lesion:
- Focus on general tissue and joint health, injury prevention, maintaining circulation to prevent thrombosis, and techniques for recurrent edema, compensatory issues, stress reduction, and emotional support.
Contraindications and Precautions
- Massage is contraindicated for at least three weeks post-surgical repair.
- Avoid undue pressure on reddened or fragile tissue and look for potential skin breakdown, cuts, or infections.
- Hydrotherapy may remain permanently modified or contraindicated.
- Avoid deep or specific techniques on paralyzed or paretic muscle tissue.
- Avoid grasping flaccid tissue to move or hold the limb.
Frequency and Prognosis of Sciatic Nerve Lesions
- In the early stages, shorter treatments (45 minutes) 2-3 times per week will be more effective for reducing edema and preventing contracture.
- In permanent lesions, longer treatments spaced further apart (weekly to monthly) will help maintain tissue health, circulation, and compensatory issues.
- Prognosis varies depending on the level of the lesion, whether it is partial or complete, and whether it is regenerating or permanent.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This lecture covers intercostal neuralgia, including the anatomy of intercostal nerves, their functions, and their relationship with arteries and veins. It explains the course of nerves 1-12 and their role in innervating muscles and receiving sensory input from the skin.