Podcast
Questions and Answers
What is a common characteristic of psoriasis?
What is a common characteristic of psoriasis?
- It primarily affects the palms of the hands.
- It causes extreme pruritus. (correct)
- It presents with a bullous rash.
- It is highly contagious.
Which of the following comorbidities is commonly associated with psoriasis?
Which of the following comorbidities is commonly associated with psoriasis?
- Erythema multiforme
- Chronic urticaria
- Rhinophyma
- Psoriatic arthritis (correct)
What triggers the symptoms of rosacea?
What triggers the symptoms of rosacea?
- Viral infections
- Cold weather
- Bacterial infections
- Direct sunlight (correct)
What is the primary treatment for severe allergic reactions characterized by urticaria?
What is the primary treatment for severe allergic reactions characterized by urticaria?
What is the main feature distinguishing the phases of rosacea?
What is the main feature distinguishing the phases of rosacea?
Which therapy is NOT commonly effective for Hidradenitis Suppurativa?
Which therapy is NOT commonly effective for Hidradenitis Suppurativa?
What is the condition known as Stevens-Johnson Syndrome primarily triggered by?
What is the condition known as Stevens-Johnson Syndrome primarily triggered by?
In which area is Hidradenitis Suppurativa most commonly found?
In which area is Hidradenitis Suppurativa most commonly found?
What is a typical feature of Erythema Multiforme?
What is a typical feature of Erythema Multiforme?
What is the initial stage of a decubitus ulcer characterized by?
What is the initial stage of a decubitus ulcer characterized by?
What does the 'D' in the ABCDEs of moles stand for?
What does the 'D' in the ABCDEs of moles stand for?
What is the main cause of malignant melanoma?
What is the main cause of malignant melanoma?
What is the 5-year survival rate if malignant melanoma is detected after metastasis?
What is the 5-year survival rate if malignant melanoma is detected after metastasis?
How does basal cell carcinoma (BCC) differ from malignant melanoma?
How does basal cell carcinoma (BCC) differ from malignant melanoma?
Which of the following describes basosquamous carcinoma (BSC)?
Which of the following describes basosquamous carcinoma (BSC)?
What is true about cutaneous papillomas?
What is true about cutaneous papillomas?
What should be observed during massage therapy for patients with a history of skin neoplasms?
What should be observed during massage therapy for patients with a history of skin neoplasms?
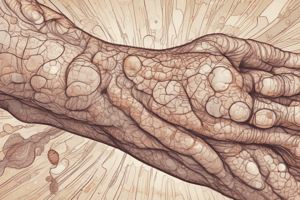
What commonly characterizes ichthyosis?
What commonly characterizes ichthyosis?
Which of the following statements is correct regarding the benign nature of sebaceous neoplasms?
Which of the following statements is correct regarding the benign nature of sebaceous neoplasms?
What is a key characteristic of basal cell carcinoma?
What is a key characteristic of basal cell carcinoma?
Which of the following is a significant characteristic of neurodermatitis?
Which of the following is a significant characteristic of neurodermatitis?
What is a common trigger for allergic contact dermatitis?
What is a common trigger for allergic contact dermatitis?
What happens during the 'itch-scratch-rash' cycle?
What happens during the 'itch-scratch-rash' cycle?
Which of the following describes Stasis Dermatitis?
Which of the following describes Stasis Dermatitis?
What is a primary treatment option for seborrheic dermatitis?
What is a primary treatment option for seborrheic dermatitis?
Which condition is characterized by erythematic vesicles and intense pruritus, appearing after a second exposure to an allergen?
Which condition is characterized by erythematic vesicles and intense pruritus, appearing after a second exposure to an allergen?
What kind of skin lesions can phototoxic dermatitis cause?
What kind of skin lesions can phototoxic dermatitis cause?
Which is NOT a treatment option for eczema?
Which is NOT a treatment option for eczema?
What distinguishing feature is associated with perioral dermatitis?
What distinguishing feature is associated with perioral dermatitis?
What characterizes phototoxic dermatitis compared to photoallergic dermatitis?
What characterizes phototoxic dermatitis compared to photoallergic dermatitis?
Flashcards
Eczema (Atopic Dermatitis)
Eczema (Atopic Dermatitis)
A chronic, itchy inflammation of the upper layers of skin, often leading to dry, scaly, leathery, or crusty skin. It can be lighter or darker than surrounding areas, and may crack, ooze fluid, and bleed.
Primary Irritant Contact Dermatitis
Primary Irritant Contact Dermatitis
Inflammation of the skin caused by direct contact with an irritant, not an allergic reaction. It is usually work-related and resolves a few days after the irritant is removed.
Allergic Contact Dermatitis (ACD)
Allergic Contact Dermatitis (ACD)
A delayed allergic reaction that causes a rash at the site of contact with an allergen. It is a cell-mediated response, meaning the immune system is involved.
Phototoxic Dermatitis
Phototoxic Dermatitis
Signup and view all the flashcards
Photoallergic Dermatitis
Photoallergic Dermatitis
Signup and view all the flashcards
Stasis Dermatitis
Stasis Dermatitis
Signup and view all the flashcards
Neurodermatitis (Localized Scratch Dermatitis or Lichen Simplex Chronicus)
Neurodermatitis (Localized Scratch Dermatitis or Lichen Simplex Chronicus)
Signup and view all the flashcards
Seborrheic Dermatitis
Seborrheic Dermatitis
Signup and view all the flashcards
Perioral Dermatitis
Perioral Dermatitis
Signup and view all the flashcards
Melanocytic Nevi (Moles)
Melanocytic Nevi (Moles)
Signup and view all the flashcards
What is Psoriasis?
What is Psoriasis?
Signup and view all the flashcards
What is the underlying cause of Psoriasis?
What is the underlying cause of Psoriasis?
Signup and view all the flashcards
What is Psoriatic Arthritis?
What is Psoriatic Arthritis?
Signup and view all the flashcards
What is Plaque Psoriasis?
What is Plaque Psoriasis?
Signup and view all the flashcards
What is Rosacea?
What is Rosacea?
Signup and view all the flashcards
What are the symptoms of Rosacea?
What are the symptoms of Rosacea?
Signup and view all the flashcards
What is Hidradenitis Suppurativa?
What is Hidradenitis Suppurativa?
Signup and view all the flashcards
What is Stevens-Johnson Syndrome (SJS)?
What is Stevens-Johnson Syndrome (SJS)?
Signup and view all the flashcards
What is Urticaria?
What is Urticaria?
Signup and view all the flashcards
What are Decubitus Ulcers?
What are Decubitus Ulcers?
Signup and view all the flashcards
Ichthyosis
Ichthyosis
Signup and view all the flashcards
Basal Cell Carcinoma (BCC)
Basal Cell Carcinoma (BCC)
Signup and view all the flashcards
Basosquamous Carcinoma (BSC)
Basosquamous Carcinoma (BSC)
Signup and view all the flashcards
Malignant Melanoma
Malignant Melanoma
Signup and view all the flashcards
Cutaneous Papilloma
Cutaneous Papilloma
Signup and view all the flashcards
Sebaceous Neoplasms
Sebaceous Neoplasms
Signup and view all the flashcards
Ichthyosis
Ichthyosis
Signup and view all the flashcards
Skin Tag
Skin Tag
Signup and view all the flashcards
ABCDEs of Moles
ABCDEs of Moles
Signup and view all the flashcards
Dysplastic Nevus
Dysplastic Nevus
Signup and view all the flashcards
Study Notes
Inflammatory Reactions of the Skin
- Psoriasis: A chronic, non-contagious, inflammatory autoimmune disease characterized by hyper-proliferation.
- Etiology: Autoimmune, often idiopathic but may be related to genetics. Smoking, obesity, alcohol use, and infections (bacterial and viral) can worsen psoriasis.
- Epidemiology: More common in some age ranges and in Caucasians.
- Signs & Symptoms: Erythematous papules and plaques covered with silvery scales; extremely pruritic. Scraping causes punctate bleeding (Auspitz's sign). New psoriasis develops at skin trauma sites (Koebner phenomenon). Common affected areas include scalp, extensor surfaces (elbows and knees), back, chest, groin, and armpits. Different classifications present with varying symptoms; plaque psoriasis is most common.
- Common Comorbidities: Psoriatic Arthritis (5-30% of psoriasis patients; ¼ develop), characterized by joint stiffness, pain, swelling, and tenderness. Nail bed involvement (1/3 of psoriasis patients) includes pitting, discoloration, and nail separation.
- Diagnosis: Clinical examination; skin biopsy for complex cases.
- Treatment: Topical corticosteroids, over-the-counter moisturizers, controlled UV light therapy (sunbathing), antihistamines for pruritus. Massage is a local contraindication if there is broken skin; light massage is permitted over intact lesions with patient consent.
- Rosacea: A chronic, progressive, erythematic skin condition causing facial redness.
- Etiology: Idiopathic; may be related to genetics or an overactive immune system.
- Epidemiology: Most common in individuals aged 30-50; more common in females and those with fair complexions.
- Signs & Symptoms: Persistent facial erythema, dryness, warmth, and swelling. Tiny pustules (acne-like). Telangiectasia (spider veins) and thickened skin can develop. Rhinophyma (erythematous, bulbous nose due to sebaceous gland hypertrophy) is a potential complication. Most common affected area: middle third of the face (nose, cheeks, chin). Symptoms often fluctuate (flare-ups/remissions); identified triggers exist.
- Rosacea Phases:
- Phase I: Pre-rosacea (redness)
- Phase II: Vascular (spider veins)
- Phase III: Inflammatory (acne)
- Phase IV: Late-stage (bulbous nose)
- Treatment: No cure; avoid triggers (sunlight, strenuous exercise, extreme temperatures, spicy foods, hot beverages, alcohol); topical antibiotics for the inflammatory phase. Massage is dependent on severity; avoid affected areas containing pustules, and inquire about sensitivity.
- Prognosis: Increased risk of migraines; linked with IBD, celiac disease, SIBO/IBS.
- Hidradenitis Suppurativa: A chronic, scarring, acne-like inflammatory process.
- Etiology: Idiopathic; hair follicle blockage is implicated, but the cause of blockage isn't fully understood. Possible connections to hormones, genetics, predisposition, cigarette smoking, and excess weight.
- Symptoms: Small, swollen, painful nodules under the skin; pain followed by pus drainage. Chronic cases develop cord-like fibrotic bands and a foul odor.
- Treatment & Prognosis: Drug therapy may not be beneficial, but consider topical antibiotics and steroids. Use warm compresses to drain pus. Laser hair removal for prevention; surgical excision might be necessary. Significant scarring is common. Massage is a local contraindication for areas with pustules, and check sensitivity.
Drug Eruptions and Reactions
- Erythema Multiforme: An inflammatory skin reaction with target-shaped lesions, involving oral mucosa. Type IV hypersensitivity (cell-mediated delayed hypersensitivity). Common triggers include drugs and infections, most significantly herpes simplex virus (~50% of cases). Symptoms include mildly itchy, symmetric red raised patches with target lesions, blisters, and mucous membrane involvement; blistering can ooze blood. Also include fatigue, joint pain, and fever. Self-limiting (2-4 weeks); antivirals may be used if HSV is the cause. Avoid massaging until lesions heal.
- Stevens-Johnson Syndrome (SJS): A life-threatening type IV hypersensitivity. Characterized by necrotic separation of the dermis from the epidermis; involves mucous membranes. Symptoms include severe blistering, difficulties with mouth opening (drooling), swallowing (dysphagia), eye involvements (painful swelling, pus-sealing), urination, and systemic symptoms like fever and fatigue. Treatment is supportive: analgesics, IV fluids, possible NG tube/parenteral nutrition. Massage is contraindicated.
- Urticaria (Hives): An inflammatory skin disorder associated with allergic reactions; Type I hypersensitivity. Transient, edematous papules (wheals) mediated by histamine. Immediate appearance. Urticaria (hives) accompanied by redness (flares). Can affect deeper tissues leading to angioedema (warm, red, painful skin). Triggers include allergens (medications, insect bites, foods, or idiopathic). Treatment involves oral antihistamines, topical corticosteroids, monitor the area surrounding the mouth. Massage is contraindicated during acute/allergic episodes, and in chronic cases it's a local contraindication.
- Decubitus Ulcers: Breakdown of skin integrity due to lack of blood flow and prolonged pressure. Tissue necrosis can occur rapidly (within 12 hours). Most common affected areas include sacrum, greater trochanter, heels; skin over bony prominences. Four stages:
- Stage I: Non-blanchable erythema (intact skin).
- Stage II: Partial-thickness skin loss.
- Stage III: Full-thickness skin loss (adipose tissue visible).
- Stage IV: Full-thickness tissue loss (muscle/bone visible).
- Massage is a local contraindication*; postpone treatment if signs of infection, odor, or discharge are present, and refer to a physician.
Dermatitis
- Atopic Dermatitis (Eczema): Most common inflammatory skin condition; immune-mediated inflammation. Involves dry, scaly, leathery, or crusty skin that can crack, ooze fluid, and bleed; an "itch-scratch-rash" cycle is common. Triggers include genetics (over-production of IgE), food/environmental allergies, emotional stress, humidity, and skin irritation. Commonly found on flexor surfaces. Treatment includes identifying and eliminating triggers, use of OTC moisturizers and topical corticosteroids. Massage is a local contraindication for broken skin; proceed with caution/consent if skin is intact, and avoid vigorous pressure.
- Primary Irritant Contact Dermatitis: Inflammation from non-immunological contact (e.g., cleaning products, detergents, dyes, fertilizers, fiberglass, latex, certain metals). Symptoms include an itchy or painful rash, erythema, scaling, or blistering with demarcated borders. Often found on hands or lips. Treatment focuses on removing the irritant; antihistamines and corticosteroids may help. Massage is a local contraindication.
- Allergic Contact Dermatitis (ACD): Type IV (delayed) cell-mediated hypersensitivity reaction. Subsequent exposure to the allergen causes pruritus and inflammation. Triggers include cosmetics, metal compounds (nickel), plants (poison ivy), drugs, skin creams, and chemicals in clothing. Intense pruritus, vesicles, and oozing are common. Treatment involves allergen avoidance, and oral/topical antihistamines and corticosteroids. Massage is a local contraindication.
- Phototoxic Dermatitis: Cutaneous reaction occurring within minutes to hours of sun exposure due to light-absorbing substances that increase skin damage via free radicals. Triggers include topical and ingested substances (perfumes, sunscreens, aftershave, oils, coal tar, tri and tetracyclic antibiotics). Painful, swollen erythematous lesions (burn-like) that are localized to sun-exposed skin. Massage is a local contraindication.
- Photoallergic Dermatitis: Type IV (delayed) cell-mediated immune response 1-3 days after sun exposure. Light absorption changes a substance into an antigen. Triggers include topical medications or photosensitizing agents (aftershave, sunscreens, sulfonamides). Erythematic vesicles and pruritus; reaction may also affect non-sun-exposed areas. Massage is a local contraindication.
- Stasis Dermatitis: Skin inflammation of the lower legs due to chronic venous insufficiency (blood pooling). Risk factors include a history of DVT (deep vein thrombosis), varicose veins, obesity, pregnancy, lack of physical activity, and smoking. Chronic, bilateral redness, warmth, swelling, scaling, dark brown hyperpigmentation (increased blood), and potential for oozing/fluid leakage (often in ankles). Massage is a local contraindication in areas with venous ulcers; be cautious.
- Neurodermatitis: Chronic, itchy inflammation leading to skin thickening (lichen simplex chronicus). Psychogenic factors, anxiety, and stress may be involved. Repeated scratching creates a vicious cycle. Common locations include arms, legs, neck, anus, and vagina. Treatment focuses on treating the potential underlying psychological issues and educating the client about the effects of scratching, using topical corticosteroids, and antihistamines. Avoid affected areas due to potential for broken skin.
- Seborrheic Dermatitis: Chronic, inflammatory disease of sebaceous glands. Possible association with Malassezia Furfur yeast, weakened immunity, stress, cold/dry climate, and diet. Pruritus, extensive dandruff, and yellow, greasy flakes. Commonly found on the face, hairline, and scalp. Treatment includes anti-inflammatory shampoos, and antifungal topicals. May be treated; adjust pressure if areas are sensitive.
- Perioral Dermatitis: Dermatitis around the mouth. Often mistaken for acne or rosacea; potential triggers include topical steroid use. Papules, pustules, scaling, and erythema are common. May be treated if areas are not sensitive.
Neoplasms of the Skin
- Melanocytic Nevi (Moles): Recognize atypical/dysplastic nevi as potential melanoma indicators using the ABCDEs (Asymmetry, Borders, Color, Diameter, Evolving).
- Malignant Melanoma: Highly dangerous, caused primarily by UV light exposure. Rapid growth and lymphatic system metastasis are characteristic. Early detection and surgical removal offer high survival rates.
- Basal Cell Carcinoma (BCC): Most common skin cancer; rarely metastasizes; originates from stratum basale (mutations from UV radiation). Appears as a pearly white nodule (various appearances). Virtually no metastasis, 100% 5-year survival rate.
- Basosquamous Carcinoma (BSC): Rare, aggressive cancer; mutates, and differentiates from BCC; caused by UV radiation.
- Sebaceous Neoplasms: Usually benign, but can be malignant; involves sebaceous glands. Can be mistaken for other tumors.
- Cutaneous Papilloma (Skin Tags): Extremely common, benign skin growths found in areas where skin rubs together, possibly associated with HPV. All skin neoplasms are local contraindications; consult with a physician and observe for new suspicious lesions.
Ichthyosis
- Ichthyosis: Group of over 30 skin diseases with similar presentations (redness, pruritus, flaky skin/plates). Etiology includes genetic mutations/inheritance. Varying symptoms depending on the specific type. Treatment often involves hydrating creams; no contraindications but consider sensitivity.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.