Podcast
Questions and Answers
Which of the following is NOT one of the cardinal signs of inflammation?
Which of the following is NOT one of the cardinal signs of inflammation?
- Pain
- Heat
- Swelling
- Bacterial growth (correct)
What is the first step in the 5-R-I process of the inflammatory response?
What is the first step in the 5-R-I process of the inflammatory response?
- Recognition of injurious agent (correct)
- Regeneration of tissues
- Resolution of inflammation
- Recruitment of leukocytes
Which of the following is considered a type of chronic inflammatory disease?
Which of the following is considered a type of chronic inflammatory disease?
- Rheumatoid arthritis (correct)
- Acute bronchitis
- Fractured bone
- Common cold
Which of the following factors can trigger an inflammatory response due to immune reactions?
Which of the following factors can trigger an inflammatory response due to immune reactions?
Which mechanism describes an acute inflammatory response to tissue necrosis?
Which mechanism describes an acute inflammatory response to tissue necrosis?
What term is used to describe inflammation caused by foreign bodies?
What term is used to describe inflammation caused by foreign bodies?
Which of these conditions involves recurrent inflammation leading to damage over time?
Which of these conditions involves recurrent inflammation leading to damage over time?
What is a potential consequence of misdirected inflammation?
What is a potential consequence of misdirected inflammation?
What is the primary difference between exudate and transudate?
What is the primary difference between exudate and transudate?
Which of the following is NOT a cardinal sign of acute inflammation?
Which of the following is NOT a cardinal sign of acute inflammation?
What causes the dilation of small blood vessels during acute inflammation?
What causes the dilation of small blood vessels during acute inflammation?
Which condition is characterized by a prolonged and persistent inflammatory response?
Which condition is characterized by a prolonged and persistent inflammatory response?
During the inflammatory response, what is one of the first changes observed in blood vessels?
During the inflammatory response, what is one of the first changes observed in blood vessels?
What role do leukocytes play in the inflammatory response?
What role do leukocytes play in the inflammatory response?
Which of the following is a common example of acute inflammation?
Which of the following is a common example of acute inflammation?
What is the primary factor that distinguishes acute inflammation from chronic inflammation?
What is the primary factor that distinguishes acute inflammation from chronic inflammation?
Flashcards are hidden until you start studying
Study Notes
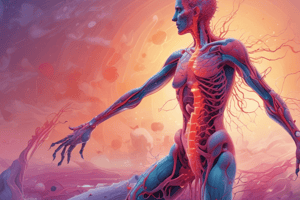
Inflammation
- Inflammation is the body's response to tissue injury or damage.
- It involves bringing cells and molecules to the injury site to eliminate the harmful agent.
- The host's cells detect stimuli from the injury site to initiate the inflammatory response.
- The inflammatory response itself can sometimes be the cause of disease.
Cardinal Signs of Inflammation
- Heat: External manifestation of inflammation.
- Redness: Also known as rubor.
- Swelling: Also known as tumor.
- Pain: Also known as dolor.
- Loss of Function: Also known as functio laesa.
Causes of Inflammation
- Infections: Caused by microbes, viruses, bacteria, and toxins.
- Tissue Necrosis: Unprogrammed cell death that can trigger inflammation in three ways:
- Ischemia: Reduced blood supply leading to hypoxia and necrosis.
- Trauma: Physical injury.
- Physical and Chemical Injuries: Such as chemical burns and frostbite.
- Foreign Bodies: Can be exogenous or endogenous.
- Exogenous: Splinters, dirt, sutures.
- Endogenous: Crystals like urate crystals (gout) and cholesterol crystals (atherosclerosis).
- Immune Reactions: The body's response to damaged tissues, also known as hypersensitivity.
- Can be caused by allergies or autoimmune diseases.
Steps of the Inflammatory Response (5-R-I)
- Recognition: The immune system identifies the injurious agent.
- Recruitment: Leukocytes are drawn to the site of injury.
- Removal: The harmful agent is eliminated.
- Regulation: The inflammatory response is controlled.
- Repair: The damaged tissue is repaired or resolved.
Types of Inflammation
- Acute Inflammation:
- The initial and rapid response to infection and tissue damage.
- Develops within minutes or hours.
- Examples: Rash from a mosquito bite.
- Heals within hours or days, with cardinal signs of pain, swelling, and redness.
- Examples: A cold-induced fever that subsides quickly.
- Chronic Inflammation:
- Persists for weeks, months, or even years.
- Involves persistent inflammation, tissue destruction, and repair attempts.
Acute Inflammation (AI)
- Components:
- Dilation of Small Blood Vessels: Increased blood flow to the injury site, known as hyperemia.
- Increased Permeability of Microvasculature: Allows plasma proteins and leukocytes to exit the circulation and travel to the injury site.
- Movement of Leukocytes: Leukocytes move out of circulation to the site of injury, accumulate, and initiate the inflammatory response.
Vascular Reactions to Acute Inflammation
- Vasodilation: Causes hyperemia.
- Increased Permeability: Allows proteins and leukocytes to enter the injured area.
Exudate and Transudate
- Exudate: Extravascular fluid with high protein concentration and cellular debris. Indicates increased vascular permeability during inflammation.
- Transudate: Extravascular fluid with low protein concentration and little cellular debris, caused by an osmotic or hydrostatic imbalance with normal vascular permeability.
Examples
- Edema: Swelling due to fluid accumulation in interstitial spaces or serous cavities. Can be either exudate or transudate.
- Pus: An exudate rich in leukocytes, dead cells, debris, and microbes.
Role of Vasculature in Acute Inflammation
- Vasodilation: Induced by mediators like histamine, leading to edema and stasis.
- Increased Vascular Permeability: Induced by mediators like histamine, bradykinin, and leukotrienes.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.