Podcast
Questions and Answers
What is the name given to the process by which normal tissue becomes a tumor?
What is the name given to the process by which normal tissue becomes a tumor?
Oncogenesis
What is the function of the mucosal epithelium?
What is the function of the mucosal epithelium?
To protect the mucosal epithelium
What are AMPs, and what is their function?
What are AMPs, and what is their function?
Antimicrobial peptides, they break holes in the lipid bilayers of pathogens.
What is the function of M cells?
What is the function of M cells?
Which of the following are considered 'effector cells' and reside in the lamina propria? (Select all that apply)
Which of the following are considered 'effector cells' and reside in the lamina propria? (Select all that apply)
What is the definition of "gnotobiotic"?
What is the definition of "gnotobiotic"?
What is the function of Peyer's patches?
What is the function of Peyer's patches?
What is an "alloreactive T-cell"?
What is an "alloreactive T-cell"?
What is the term for the safety mechanism of the Tregs that allows for the suppression of autoimmune responses?
What is the term for the safety mechanism of the Tregs that allows for the suppression of autoimmune responses?
Autoimmune diseases are rarely resolved or cured, and are only managed.
Autoimmune diseases are rarely resolved or cured, and are only managed.
What are the 4 methods that the immune system eliminates cancer?
What are the 4 methods that the immune system eliminates cancer?
The higher the levels of TILs (tumor-infiltrating lymphocytes) a patient has, the lower the survival statistics.
The higher the levels of TILs (tumor-infiltrating lymphocytes) a patient has, the lower the survival statistics.
What are two ways that tumors can escape immune detection?
What are two ways that tumors can escape immune detection?
What is the term for the process by which the tumor continues to mutate and divide in subpopulations to evade death and detection?
What is the term for the process by which the tumor continues to mutate and divide in subpopulations to evade death and detection?
What are the two primary ways the immune system inhibits the activation of T-cells?
What are the two primary ways the immune system inhibits the activation of T-cells?
What does "ACT" stand for?
What does "ACT" stand for?
What is the name of the specific type of immune cell used in ACT?
What is the name of the specific type of immune cell used in ACT?
Flashcards
Systemic Immune System
Systemic Immune System
A type of immune response that is reactive to pathogens. It often involves inflammation as a key component.
Mucosal Immune System
Mucosal Immune System
A type of immune response that is proactive in defending against pathogens. Inflammation is typically undesirable in this system.
Mucin
Mucin
A glycoprotein produced by mucosal epithelial cells that acts as a protective barrier.
Defensin
Defensin
Signup and view all the flashcards
Commensal Organism
Commensal Organism
Signup and view all the flashcards
Why Commensal Organisms Can Become Pathogenic
Why Commensal Organisms Can Become Pathogenic
Signup and view all the flashcards
Enterocyte
Enterocyte
Signup and view all the flashcards
Goblet Cell
Goblet Cell
Signup and view all the flashcards
Paneth Cell
Paneth Cell
Signup and view all the flashcards
Intestinal Stem Cell (ISC)
Intestinal Stem Cell (ISC)
Signup and view all the flashcards
Lamina Propria
Lamina Propria
Signup and view all the flashcards
Villi
Villi
Signup and view all the flashcards
Isolated Lymphoid Follicle
Isolated Lymphoid Follicle
Signup and view all the flashcards
Inductive Compartment
Inductive Compartment
Signup and view all the flashcards
Gnotobiotic
Gnotobiotic
Signup and view all the flashcards
M Cell
M Cell
Signup and view all the flashcards
Intraepithelial Lymphocyte (IEL)
Intraepithelial Lymphocyte (IEL)
Signup and view all the flashcards
Peyer's Patches
Peyer's Patches
Signup and view all the flashcards
Intestinal Macrophages vs. Professional Antigen-Presenting Macrophages
Intestinal Macrophages vs. Professional Antigen-Presenting Macrophages
Signup and view all the flashcards
Oral Tolerance
Oral Tolerance
Signup and view all the flashcards
IgA Subclasses
IgA Subclasses
Signup and view all the flashcards
Hypersensitivity Reaction
Hypersensitivity Reaction
Signup and view all the flashcards
Allergen
Allergen
Signup and view all the flashcards
Atopy
Atopy
Signup and view all the flashcards
Anaphylaxis
Anaphylaxis
Signup and view all the flashcards
Type I Hypersensitivity Reaction
Type I Hypersensitivity Reaction
Signup and view all the flashcards
IgE Properties
IgE Properties
Signup and view all the flashcards
Fc Receptor (FceRI)
Fc Receptor (FceRI)
Signup and view all the flashcards
Mast Cell
Mast Cell
Signup and view all the flashcards
Eosinophil
Eosinophil
Signup and view all the flashcards
Basophil
Basophil
Signup and view all the flashcards
PEFR (Peak Expiratory Flow Rate) Test
PEFR (Peak Expiratory Flow Rate) Test
Signup and view all the flashcards
Omalizumab
Omalizumab
Signup and view all the flashcards
AR101 (Palforzia) - Desensitization
AR101 (Palforzia) - Desensitization
Signup and view all the flashcards
Study Notes
Chapter 10: Systemic and Mucosal Immunity
- Systemic immunity is reactive, inflammation is common
- Mucosal immunity is proactive, inflammation is avoided.
- Mucin is a glycoprotein produced by mucosal epithelium; it protects the mucosal epithelium.
- Mucins are large collections of polypeptides, either secreted or membrane-bound.
- Membrane-bound mucins trap microorganisms, aiding pathogen removal.
- Defensins are AMPs (antimicrobial peptides) that create holes in pathogen lipid bilayers.
- Commensal organisms benefit the host but don't have a close relationship.
- Commensal organisms are one step below symbiotic relationships.
- Commensal organisms help synthesize metabolites, break down fibers, inactivate toxins, act as a barrier in the gut and stimulate secondary lymphoid tissue.
- Commensal organisms can become pathogenic if they don't stay put.
Subsets of Gut Epithelial Cells
- AMPs (antimicrobial peptides), such as defensins, disrupt pathogen membranes.
- ILCs (innate lymphoid cells) may or may not care about pathogens, depending on the context.
- Enterocytes absorb nutrients
- Goblet cells produce and secrete mucus.
- Paneth cells secrete AMPs (e.g., defensins).
- ISC (intestinal stem cells) replace gut epithelial cells.
M cells and Intraepithelial Lymphocytes
- M cells transport microbes/antigens into the intestinal tissue.
- IELs (intraepithelial lymphocytes) are essentially cytotoxic T-cells in the epithelium.
- Peyer's patches are secondary lymphoid organs in the small intestine.
Macrophages and Oral Tolerance
-
Intestine macrophages don't secrete cytokines and lack a significant inflammatory response.
-
Oral tolerance relates to the immune system's ability to not respond to food antigens.
Chapter 14: Hypersensitivity Reactions
- Hypersensitivity reactions are exaggerated inflammatory responses to allergens.
- Atopy is a genetic predisposition to allergy.
- Anaphylaxis is a severe hypersensitivity reaction that can cause organ damage and asphyxiation.
- Type I hypersensitivity involves immediate degranulation of mast cells when an allergen binds to IgE.
Mast Cells, Eosinophils and Basophils
- Mast cells, eosinophils, and basophils have high-affinity IgE receptors.
- Mast cells release histamine and other cytokines, causing inflammation.
- Eosinophils release cytotoxic granules, harming tissues in allergic reactions.
- Basophils cause tissue damage in allergic reactions and have regulatory roles in initiating Th2 responses
Chapter 16: Immunological Self-tolerance
- Immunological self-tolerance is a process that prevents the immune system from attacking its own tissues.
- Mechanisms include negative selection of B and T cells in the bone marrow and thymus, induction of anergy, lymphatic exclusion, and T-reg cell suppression.
- Autoimmune diseases fail to resolve because they are only managed.
- AIRE allows for presentation of non-thymus antigens to T-cells for negative selection, defects in AIRE lead to autoimmune disease.
- FOXP3 is a transcriptional repressor involved in T-reg function and autoimmunity.
- HLA is a major genetic factor for autoimmune disease susceptibility, with women more impacted than men.
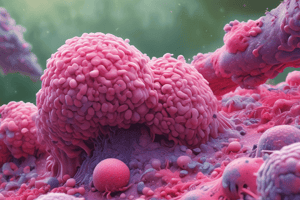
Chapter 17: Oncogenesis, Metastasis, and Cancer
- Oncogenesis is the development of tumors.
- Metastasis signifies tumor spreading to other tissues.
- Proto-oncogenes are genes involved in cell growth and regulation, while oncogenes have mutations that increase proliferation.
- Tumor suppressor genes constrain cell growth and mutation.
- Malignant tumors can invade nearby tissues (metastasis).
- Benign tumors remain localized.
- The multi-hit model suggests that cancer requires multiple mutations for tumor growth.
- Neoantigens are tumor-specific antigens, allowing the immune system to recognize and eliminate tumors.
- The immune system eliminates cancer cells by presentation of antigens with MHC molecules, through cytotoxic T-cells, antibody-dependent cellular cytotoxicity, antibody-dependent phagocytosis, or TIME (tumour immune microenvironment).
Chapter 15: Transplantations
-
Grafts are types of transplanted tissues or cells.
-
Autograft uses self-tissue, isograft uses a identical donor, allograft uses a different donor of the same species, and xenograft uses donors of different species.
-
Histocompatibility is similar between donors and recipients (no inflammation), whereas histoincompatibility shows differences that the immune system does respond to.
-
ABO blood types and Rh factors must be matched for blood transfusions to avoid rejection.
Chapter 14: ABO blood incompatibility
- Different blood types have different antigens (A, B, AB, O).
- Someone with type O blood can donate blood to anyone (universal donor).
- Someone with type AB blood can receive blood from anyone (universal recipient).
Chapter 17: Tumor Immune Editing
- Tumor immunoediting refers to the process by which tumors mutate and divide to evade death and detection from the immune system.
- Tumor-treated as self, low immunogenicity, immune suppression and antigenic modulation are tumor immune escape mechanisms and strategies tumors use to evade immune responses.
- Low immunogenicity means the tumor does not stimulate immune response.
- Tumor cells treated as "self" cells are not targeted, meaning their presence is not acknowledged.
- Immune modulation involves suppressing the immune response within a physical barrier; the tumor then is not attacked.
- Antigenic modulation means the tumor loses its immunogenic antigens and is not targeted.
Chapter 17: Immunotherapy for Cancer
- Chimeric antigen receptor (CAR) T-cells, which are genetically engineered to target specific tumor antigens, can prevent activation of T-cells and thus bypass the need for MHC.
- Radio-conjugated antibodies allow for targeted delivery of radiation to cancer cells.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.