Podcast
Questions and Answers
Which of the following best describes the primary function of the immune system?
Which of the following best describes the primary function of the immune system?
- To produce hormones that regulate growth and development.
- To regulate the body's temperature through vasodilation and vasoconstriction.
- To protect against infectious microbial diseases and cancer. (correct)
- To facilitate the transmission of pathogens.
Which of the following is NOT a physical barrier or secretion that the body uses to prevent pathogen entry?
Which of the following is NOT a physical barrier or secretion that the body uses to prevent pathogen entry?
- Saliva
- Mucus
- Bone marrow (correct)
- Skin
What is the main role of mucosal tissue in the immune system?
What is the main role of mucosal tissue in the immune system?
- To provide structural support to the body.
- To secrete hormones that regulate the immune response.
- To produce red blood cells.
- To trap potential pathogens and transport them out of the body. (correct)
In the context of the immune system, what is the role of pluripotent hematopoietic stem cells found in the bone marrow?
In the context of the immune system, what is the role of pluripotent hematopoietic stem cells found in the bone marrow?
Which process primarily occurs in the thymus?
Which process primarily occurs in the thymus?
Which of the following is a primary function of secondary lymphoid tissue?
Which of the following is a primary function of secondary lymphoid tissue?
What is the role of lymph nodes within the lymphatic system?
What is the role of lymph nodes within the lymphatic system?
How does the spleen function similarly to a lymph node?
How does the spleen function similarly to a lymph node?
Which of the following is the primary function of the follicles within a lymph node?
Which of the following is the primary function of the follicles within a lymph node?
What is the main function of the red pulp in the spleen?
What is the main function of the red pulp in the spleen?
Which component of the spleen houses T cells?
Which component of the spleen houses T cells?
Which of the following characteristics is associated with innate immunity?
Which of the following characteristics is associated with innate immunity?
Which of the following mechanisms is NOT primarily involved in the initial physical defense against pathogens?
Which of the following mechanisms is NOT primarily involved in the initial physical defense against pathogens?
Which of the following is NOT a component of the lymph node?
Which of the following is NOT a component of the lymph node?
A patient presents with symptoms of an allergic reaction. Which of the following cell types is most likely contributing to these symptoms through the release of inflammatory mediators?
A patient presents with symptoms of an allergic reaction. Which of the following cell types is most likely contributing to these symptoms through the release of inflammatory mediators?
What is the primary distinction between adaptive and innate immunity?
What is the primary distinction between adaptive and innate immunity?
The complement system is a part of which type of immunity?
The complement system is a part of which type of immunity?
Which of the following is a primary function of professional phagocytes in the innate immune response?
Which of the following is a primary function of professional phagocytes in the innate immune response?
How does the response of innate immunity differ upon repeated exposure to the same pathogen, compared to adaptive immunity?
How does the response of innate immunity differ upon repeated exposure to the same pathogen, compared to adaptive immunity?
How do innate immune cells recognize pathogens?
How do innate immune cells recognize pathogens?
What is the primary mechanism by which natural killer (NK) cells eliminate target cells?
What is the primary mechanism by which natural killer (NK) cells eliminate target cells?
Macrophages contribute to the immune response by producing immunomodulatory substances. Which of the following is an example of such a substance?
Macrophages contribute to the immune response by producing immunomodulatory substances. Which of the following is an example of such a substance?
Which cell surface protein is present on macrophages and involved in antigen presentation?
Which cell surface protein is present on macrophages and involved in antigen presentation?
How do reflexes such as coughing and sneezing contribute to the innate immune response?
How do reflexes such as coughing and sneezing contribute to the innate immune response?
During a secondary antibody response, which immunoglobulin isotype is predominantly produced and what characteristic distinguishes its affinity compared to the primary response?
During a secondary antibody response, which immunoglobulin isotype is predominantly produced and what characteristic distinguishes its affinity compared to the primary response?
A researcher is studying the effects of a novel cytokine on T cell activation. Which cellular process is directly initiated by cytokine binding to its receptor on the T cell surface?
A researcher is studying the effects of a novel cytokine on T cell activation. Which cellular process is directly initiated by cytokine binding to its receptor on the T cell surface?
If a patient lacks the ability to perform isotype switching, what would be the predictable outcome after a viral infection?
If a patient lacks the ability to perform isotype switching, what would be the predictable outcome after a viral infection?
A new therapeutic drug aims to enhance the immune response by increasing the serum concentration of antibodies during a secondary exposure to a pathogen. What specific aspect of the secondary response is the drug targeting?
A new therapeutic drug aims to enhance the immune response by increasing the serum concentration of antibodies during a secondary exposure to a pathogen. What specific aspect of the secondary response is the drug targeting?
Following a successful vaccination, memory B cells are generated. What role do these memory B cells play when the individual encounters the same antigen years later?
Following a successful vaccination, memory B cells are generated. What role do these memory B cells play when the individual encounters the same antigen years later?
Which of the following is NOT a typical outcome of complement activation?
Which of the following is NOT a typical outcome of complement activation?
A patient's blood sample shows an elevated level of C3b. Which of the following processes is most likely to be enhanced in this patient?
A patient's blood sample shows an elevated level of C3b. Which of the following processes is most likely to be enhanced in this patient?
Which pathway of complement activation is LEAST dependent on the presence of antibodies?
Which pathway of complement activation is LEAST dependent on the presence of antibodies?
A researcher is studying the effects of a novel drug on the inflammatory response. Which of the following would indicate that the drug is successfully reducing inflammation?
A researcher is studying the effects of a novel drug on the inflammatory response. Which of the following would indicate that the drug is successfully reducing inflammation?
How does the adaptive immune system enhance its response upon repeated exposure to the same pathogen?
How does the adaptive immune system enhance its response upon repeated exposure to the same pathogen?
Cytotoxic T cells (CD8+) are primarily involved in which type of adaptive immune response?
Cytotoxic T cells (CD8+) are primarily involved in which type of adaptive immune response?
Which of the following best describes the role of T helper cells (CD4+) in adaptive immunity?
Which of the following best describes the role of T helper cells (CD4+) in adaptive immunity?
How do T cell receptors (TCRs) interact with the major histocompatibility complex (MHC)?
How do T cell receptors (TCRs) interact with the major histocompatibility complex (MHC)?
Which cell surface proteins are characteristically found on T helper cells?
Which cell surface proteins are characteristically found on T helper cells?
What distinguishes MHC class I receptors from MHC class II receptors in terms of their expression?
What distinguishes MHC class I receptors from MHC class II receptors in terms of their expression?
What is the primary function of B cells in adaptive immunity?
What is the primary function of B cells in adaptive immunity?
If a patient's cells are deficient in MHC class I expression, which immune function would be most significantly impaired?
If a patient's cells are deficient in MHC class I expression, which immune function would be most significantly impaired?
During an adaptive immune response, how do T helper cells and B cells interact to enhance antibody production?
During an adaptive immune response, how do T helper cells and B cells interact to enhance antibody production?
Flashcards
What is immunology?
What is immunology?
Protection against infectious diseases caused by microorganisms and protection against cancer
What are the body's main barriers to pathogens?
What are the body's main barriers to pathogens?
Physical barriers (skin), secretions (saliva and tears), mucosal tissue (lungs, airways, and gut), and tissue-resident immune cells
What comprises the immune system?
What comprises the immune system?
Tissues and cells throughout the body, including primary and secondary lymphoid tissues.
What are primary lymphoid tissues?
What are primary lymphoid tissues?
Signup and view all the flashcards
What is located in the bone marrow?
What is located in the bone marrow?
Signup and view all the flashcards
What is the role of the thymus?
What is the role of the thymus?
Signup and view all the flashcards
What are secondary lymphoid tissues?
What are secondary lymphoid tissues?
Signup and view all the flashcards
What is the function of lymph nodes?
What is the function of lymph nodes?
Signup and view all the flashcards
Lymph Node Function
Lymph Node Function
Signup and view all the flashcards
Lymph Node Follicle
Lymph Node Follicle
Signup and view all the flashcards
Lymph Node Medulla
Lymph Node Medulla
Signup and view all the flashcards
Lymph Node Paracortex
Lymph Node Paracortex
Signup and view all the flashcards
Spleen Sinusoids
Spleen Sinusoids
Signup and view all the flashcards
PALS (Periarterial Lymphatic Sheath)
PALS (Periarterial Lymphatic Sheath)
Signup and view all the flashcards
Innate Immunity
Innate Immunity
Signup and view all the flashcards
Acquired/Adaptive Immunity
Acquired/Adaptive Immunity
Signup and view all the flashcards
Skin's Role
Skin's Role
Signup and view all the flashcards
Mucus Function
Mucus Function
Signup and view all the flashcards
Cilia's Role
Cilia's Role
Signup and view all the flashcards
Reflexes in Immunity
Reflexes in Immunity
Signup and view all the flashcards
Natural Killer (NK) Cells
Natural Killer (NK) Cells
Signup and view all the flashcards
Phagocytes Function
Phagocytes Function
Signup and view all the flashcards
Mast Cells & Basophils
Mast Cells & Basophils
Signup and view all the flashcards
PAMPs and PRRs
PAMPs and PRRs
Signup and view all the flashcards
Humoral Innate Immune Response
Humoral Innate Immune Response
Signup and view all the flashcards
Complement
Complement
Signup and view all the flashcards
Complement Activation Pathways
Complement Activation Pathways
Signup and view all the flashcards
Cell-Mediated Immunity
Cell-Mediated Immunity
Signup and view all the flashcards
Humoral Immunity
Humoral Immunity
Signup and view all the flashcards
Primary Antibody Response
Primary Antibody Response
Signup and view all the flashcards
Secondary Antibody Response
Secondary Antibody Response
Signup and view all the flashcards
Cytokines
Cytokines
Signup and view all the flashcards
Cytokine Mode of Action
Cytokine Mode of Action
Signup and view all the flashcards
Antibody Titre
Antibody Titre
Signup and view all the flashcards
T cells vs. B cells
T cells vs. B cells
Signup and view all the flashcards
TCRs and BCRs
TCRs and BCRs
Signup and view all the flashcards
MHC Class I vs. Class II
MHC Class I vs. Class II
Signup and view all the flashcards
Cellular vs. Humoral Immunity
Cellular vs. Humoral Immunity
Signup and view all the flashcards
What cells does the Cellular adaptive response use?
What cells does the Cellular adaptive response use?
Signup and view all the flashcards
What cells does the Humoral adaptive response use?
What cells does the Humoral adaptive response use?
Signup and view all the flashcards
CD4 vs. CD8
CD4 vs. CD8
Signup and view all the flashcards
MHC Genetic Encoding
MHC Genetic Encoding
Signup and view all the flashcards
Study Notes
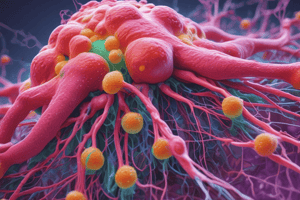
- Immunology provides protection against infectious diseases caused by microorganisms like bacteria, viruses, protozoa, fungi, and parasites
- Immunology provides protection against cancer
Pathogen Transmission
- Pathogens can be transmitted through airborne transmission, contact, contaminated water, blood stream, or tissues
The Immune System
- The immune system is divided into the innate and adaptive immune systems
Innate Immune System
- Provides physical defenses like skin, cough reflex, tears, mucosal layers, and stomach acids
- Includes phagocytes such as monocytes, macrophages, neutrophils, NK cells, and dendritic cells
Adaptive Immune System
- Includes T-lymphocytes, specifically helper T-cells, suppressor T-cells, and cytotoxic T-cells
- Contains B-lymphocytes, further divided into clonal B-cells and memory B-cells
Physical Barriers
- Skin is a physical barrier
Secretions
- Secretions contain molecules that can neutralize bacteria
- Secretions include saliva and tears
Mucosal Tissue
- Lungs, airways, and the gut are coated with mucus
- Mucosal tissue traps potential pathogens
- Mobile ciliate hair transports 'contaminants' out
Tissue Resident Immune Cells
- Skin, mucosal surfaces, and airways have cells that fight pathogens
Organisation of the Immune System
- The immune system is comprised of tissues and cells throughout the body
Primary Lymphoid Tissue
- Bone marrow contains pluripotent hematopoietic stem cells and is the source of most cells in the immune system
- T cells produced in the bone marrow must travel to the thymus to complete their maturation
Secondary Lymphoid Tissue
- Lymph nodes
- Spleen
Primary Lymphoid Tissue - Thymus
- Thymus is an encapsulated lymphoid organ
- T cell maturation and differentiation occurs in the thymus
- The cortex is rich with immature T cells, and the medulla contains sparse mature T cells
Secondary Lymphoid Tissue
- Lymph nodes
- Spleen
- Mucosa-associated lymphoid tissue
- Secondary lymph tissues are an important site for adaptive immune responses and contain lymphocytes
- The lymphatic system consists of vessels draining fluids from body tissue
- Lymph nodes monitor lymph for signs of infection
- Mucosa-associated lymphoid tissues are important for mucosal immune response in the gut and airways
- The spleen serves as a lymph node for the blood
Secondary Lymphoid Tissue - Lymph Node
- A lymph node is an encapsulated, trabeculated lymphoid organ that has many afferent and one or more efferent branches
- Lymph nodes act as a filter, storage, activation centre for B and T lymphoid cells, and a centre for antibody production
Lymph Node Components
- Follicles are the site of B cell storage and proliferation
- The medulla is composed of medullary cords and sinuses acting as a filter
- The paracortex is the location of the T cells
Secondary Lymphoid Tissue - Spleen
- Sinusoids are composed of elongated channels with a fenestrated membrane and adjacent macrophages, functioning as filters.
- Periarterial lymphatic sheath (PALS) houses T cells
- Follicles are the site where white pulp houses B cells
- The spleen contains two major units: white pulp and red pulp
- The white pulp is composed of lymphatic tissue and contains mainly WBC which initiate adaptive immune response
- White pulp around the spleen is surrounded by red pulp
Immune Cells
- Immune cells derive from stem cells
- Myeloid progenitor cells produce dendritic cells, macrophages, monocytes, and neutrophils
- Lymphoid progenitor cells make NK-cells, T-cells and B-cells
Immune System Overview
- Innate immunity provides physical and biochemical barriers inside and outside the body
- Innate immunity uses cells with specific functions and responses
- Innate immunity has no memory
- Innate immunity does not use antibodies but does involve a complement system
- Acquired/adaptive immunity provides a specific response to infectious agents, which depends on antigen presentation, recognition, and the antigen-antibody response
- Adaptive immunity has memory and uses antibodies
Innate Immune System Overview
- The nonspecific immune response indiscriminately attacks invaders (virus, bacteria, parasite)
- There is no memory; repeated exposures to the same pathogen generate the same response as the first exposure
- The first line of defense comes from the innate immune system
- Most pathogens enter the body via the respiratory system, gut, or genitourinary tract
- Skin provides an effective physical barrier to pathogens
- Mucus can trap and remove particles and small organisms
- Cilia lining the trachea and main bronchi catch and remove pathogens
- Reflexes (coughing, sneezing, fever) eliminate and destroy pathogens
Innate Immunity - Cell Types
- 2 primary cell types are involved in the innate immune response: natural killer (NK) cells and phagocytes
- Natural killer (NK) cells recognize virally infected and malignant cells, as well as antibody-opsonized cells
- NK cell binding to a target cell releases cytolytic and cytotoxic granules to kill target cells via apoptosis
- Phagocytic cells engulf debris, infectious particles, and bacteria, which are then destroyed and removed
- Neutrophils are efficient phagocytes
- Macrophages are recruited to the site of infection
Innate Immunity - Cells
- Cellular and humoral components make up innate immunity Mast cells and basophils secrete histamines to mediate inflammation
- Mast cells are tissue resident
- Basophils are found in the blood
- Mast cells and basophils play a key role in allergic response (hypersensitivity type I)
- Phagocytosis is carried out by Neutrophils and Macrophages
- These respond to signs of infection (i.e. inflammation) in the tissue
- Phagocytosis Recognizes microorganisms by pathogen-associated molecular patterns (PAMPs) on the microbial surface
- Recognition is carried out by pattern recognition receptors (PRRs), e.g., Toll-like receptors (TLRs)
- This results in neutralisation and phagocytosis
Phagocytes in the Body
- Phagocytes enter an infected site from circulation
- Phagocytes bind, engulf, and kill a wide variety of microbial agents
- Phagocytes produce immunomodulatory substances (cytokines, chemokines), which regulate the immune response
- Phagocytes act as the first line of defense against infection
Cell Surface Proteins of Immune Cells
- Immune cells have cell surface proteins
- Macrophages have MHC II, B7, CD40, CD14
- Proteins have distinct functions, supporting cell interaction and communication
- Macrophages (APC) express MHC II
- MHC II in complex with antigenic peptides bind to T cell TCR
Non-Cellular (Humoral) Innate Immune Response
- Humoral innate immune response attacks pathogens in a rapid, non-specific manner
Complement
- Plasma proteins destroy cell membranes (lytic pore)
- Plasma proteins attract phagocytes & stimulate activity of other immune cells. (C3a, and C5a)
- Plasma proteins promote phagocytosis (Opsonins, C3b/iC3b, C4b)
Fever
- Elevation of body temperature due to pyrogens (COX-2)
Inflammation
- Mast cells release pro-inflammatory cytokines & chemokines
- Blood vessels dilate
- Allows influx of immune cells and fluid (plasma)
- Results in symptoms of pain, swelling, redness and heat
Complement
- The complement system consists of small proteins in the blood that interact with the immune system
- Important in humoral immunity and inflammation
- There are 3 pathways that activate the complement system: classical, alternative, and lectin
- A classical pathway requires antibodies, typically IgG and IgM, bound to antigens
- An alternative pathway requires the presence of antigens, such as endotoxin, or a foreign surface, such as a bacterial surface
- The Lectin pathway requires the presence of bacterial carbohydrates
Adaptive Immune System
- Involves both humoral and cell-mediated immunity
- Cell-mediated immunity relies on direct contact between immune cells and the pathogen
- Humoral immunity is an antibody-mediated response that relies on proteins (antibodies) to convey signals between cells
- Adaptive immunity is specific for a given pathogen
- Repeated exposure causes an enhanced immune response
T and B Cells
- Provide for acquired immunity
- T cells promote cell-mediated activation of B cells and other immune cells (T helper or CD4+ T cells), or direct cell killing (cytotoxic or CD8+ T cells)
- B cells make antibodies: IgM, IgG, IgD, IgE, IgA
Adaptive Immunity - Receptors
- T CELLS carry T cells receptors (TCRs)
- B CELLS carry B cell receptors (BCRs)
- Structures allow for high specificity
- Major histocompatibility complex plays an important role in adaptive immunity
- MHC class I receptors are on all nucleated body cells
- MHC class II receptors are on antigen-presenting cells (APCs)
- Both interact with TCRs
Cellular vs Humoral Adaptive Response
- The cellular adaptive response is mediated by cytotoxic T cells (CD8+)
- Targets infected body cells (e.g. viruses) and malignant cells (e.g. cancer)
- The humoral adaptive response is affected by B cells (antibodies)
- Targets pathogens or antigens in the blood stream or on mucosal surfaces
- Helper T cells (CD4+) are essential as 'gatekeepers'
Cell Surface Proteins of Immune Cells
- T helper cells have CD4, TCR, CD3, CD28, CD40L
- Cytotoxic T cells have CD8, TCR, CD3
- Proteins have distinct functions, supporting cell interaction and communication
- T cell TCR binds and interacts with MHC class I or II
MHC I and II
- An important acquired immunity component is the major histocompatibility complex or MHC
- MHC I and MHC II have distinct functions
- The MHC is a complex of proteins encoded by human leukocyte antigen (HLA) genes
- MHC I is encoded by HLA-A, HLA-B, and HLA-C and expressed on nucleated cells
- MHC II is encoded by HLA-DR, HLA-DP, and HLA-DQ and expressed on antigen-presenting cells (APCs)
T Cell Differentiation
- T cells play an important role in cell-mediated acquired immunity
- T cell precursor cells from the bone marrow travel to the thymus where they differentiate into CD8+ and CD4+ cells
- These cells then travel to the lymph node where they further differentiate:
- CD8+ cells: differentiate into cytotoxic T cells
- CD4+ cells: differentiate into T helper cells
T Helper Cell Subsets
- Th1 guides the adaptive response towards a cellular profile (Cytotoxic T cells, intracellular pathogens)
- Th2 guides the adaptive response towards a humoral profile (B cells, extracellular pathogens)
- Th17 responds to extracellular bacteria and fungi, IL-17
- T regs control the immune response to self and foreign particles (antigens)
The Role of B Cells
- B cells are essential for The primary and secondary antibody response The body produces B cells that express a wide variety of surface receptors (BCRs) of IgD or IgM class
- Humoral adaptive immune reposnse recognizes antigens via antibodies
- An antigen is a substance that elicits an antibody's production, and binds specifically with that antibody
- An antibody are proteins that are classified as immunoglobulins, are produced by plasma cells (B cell derived), and are defined functionally
- Antibodies include IgM, IgG, IgE, IgD, IgA
Antibodies
- Fab fragment: Binds to antigens with light and heavy chains that recognize distinct antigens.
- Fc fragment: Determines the antibody class and fixes complement.
Antibody Function
- Opsonisation - Promotes phagocytosis via Fc receptors recognizing antibody-antigen complexes and binding antibody via its Fc fragment
- Neutralisation - Inhibits the antigen (e.g. bacterial adherence) by blocking a surface protein required for adhering to cell surfaces
- Complement activation - Antibody-antigen complexes bind, triggering the classical pathway of complement
- Complement pathway activation results in opsonins (C4b, C3b) and amplification via the alternative pathway
Antibody Responses
- Primary response involves B cells proliferating into plasma cells, which secrete antibodies and create memory B cells
- IgM is also involved
Secondary Response
- Involves antigen-specific memory, where B cells secrete antibodies and cause isotype switching
- Involves IgG
- Displays higher affinity and higher titre (serum concentration)
Cytokines
- Cytokines are immune mediators
- A particular cytokine's effects occur through its high-affinity binding of its receptor on the surface of a target cell.
- Can stimulate or inhibit the differentiation, proliferation and activity of immune cells
Examples of Cytokines
- Interferon family act as antiviral proteins
- Chemokine family directs cell migration, adhension and activation
- Tumour necrosis factor family regulate inflammatory and immune responses
- Interleukin family vary in action depending on upon interleukin and cell type
- Haematopoietins promotes cell proliferation and differentiation
- Transforming growth factor beta family regulates immune cells
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore the primary functions of the immune system. Learn about physical barriers, mucosal tissues, and hematopoietic stem cells. Also, understand the roles of the thymus, lymph nodes, spleen, innate immunity and lymphoid tissue.