Podcast
Questions and Answers
What is the main purpose of the respiratory system in relation to the circulatory system?
What is the main purpose of the respiratory system in relation to the circulatory system?
- To regulate body temperature through air exchange.
- To exchange oxygen and carbon dioxide with the external environment. (correct)
- To supply nutrients and remove waste products from tissues.
- To transport hormones to various tissues.
Which of the following processes is NOT a part of pulmonary physiology?
Which of the following processes is NOT a part of pulmonary physiology?
- Breathing in and out through the lungs.
- Exchanging oxygen with the environment.
- Metabolism of organic molecules for energy. (correct)
- Eliminating carbon dioxide from the blood.
Which structures are a part of the human respiratory system?
Which structures are a part of the human respiratory system?
- Spinal cord and nerves.
- Lungs and airways. (correct)
- Kidneys and bladder.
- Heart and blood vessels.
How do complex organisms like humans primarily exchange gases?
How do complex organisms like humans primarily exchange gases?
What principle of physiology is illustrated by gas diffusion in the respiratory system?
What principle of physiology is illustrated by gas diffusion in the respiratory system?
What is the primary function of the alveoli in the respiratory system?
What is the primary function of the alveoli in the respiratory system?
During which phase of the respiratory cycle does air flow into the lungs?
During which phase of the respiratory cycle does air flow into the lungs?
Which structure separates the respiratory and digestive pathways in humans?
Which structure separates the respiratory and digestive pathways in humans?
Which zone of the airways is responsible for gas exchange?
Which zone of the airways is responsible for gas exchange?
What is the role of the cilia in the airway epithelium?
What is the role of the cilia in the airway epithelium?
What genetic mechanism causes cystic fibrosis?
What genetic mechanism causes cystic fibrosis?
Which type of alveolar cell is responsible for producing surfactant?
Which type of alveolar cell is responsible for producing surfactant?
What is the primary function of macrophages in the alveoli?
What is the primary function of macrophages in the alveoli?
What adaptation allows for low resistance in pulmonary circulation?
What adaptation allows for low resistance in pulmonary circulation?
Which protective mechanism helps prevent lung infection by trapping pathogens?
Which protective mechanism helps prevent lung infection by trapping pathogens?
What is the role of intrapleural fluid in the respiratory system?
What is the role of intrapleural fluid in the respiratory system?
How does ventilation occur according to the principles of physics?
How does ventilation occur according to the principles of physics?
What happens to intrapleural pressure during normal breathing?
What happens to intrapleural pressure during normal breathing?
Which of the following layers of pleura is attached directly to the lung?
Which of the following layers of pleura is attached directly to the lung?
What is the significance of the equation F = ΔP/R in the context of respiratory physiology?
What is the significance of the equation F = ΔP/R in the context of respiratory physiology?
What happens to the transpulmonary pressure at the end of inspiration?
What happens to the transpulmonary pressure at the end of inspiration?
During expiration at rest, which of the following primarily contributes to the process?
During expiration at rest, which of the following primarily contributes to the process?
What is the effect of the contraction of the inspiratory muscles on the thoracic dimensions?
What is the effect of the contraction of the inspiratory muscles on the thoracic dimensions?
Boyle's law describes the relationship between which two factors in the context of lung mechanics?
Boyle's law describes the relationship between which two factors in the context of lung mechanics?
What initiates active expiration during exercise compared to passive expiration at rest?
What initiates active expiration during exercise compared to passive expiration at rest?
What occurs when the alveolar pressure (Palv) is greater than the atmospheric pressure (Patm)?
What occurs when the alveolar pressure (Palv) is greater than the atmospheric pressure (Patm)?
According to Boyle's law, what happens to gas pressure when the volume of its container is decreased?
According to Boyle's law, what happens to gas pressure when the volume of its container is decreased?
What is the role of intrapleural pressure (Pip) during inspiration?
What is the role of intrapleural pressure (Pip) during inspiration?
What is the importance of transpulmonary pressure (Ptp) in lung function?
What is the importance of transpulmonary pressure (Ptp) in lung function?
What effect does chest wall expansion have during the process of inspiration?
What effect does chest wall expansion have during the process of inspiration?
How does low lung compliance affect the work of breathing?
How does low lung compliance affect the work of breathing?
What role does surfactant play in lung function?
What role does surfactant play in lung function?
According to the Law of Laplace, what happens to the pressure in alveoli as their radius decreases?
According to the Law of Laplace, what happens to the pressure in alveoli as their radius decreases?
What is the primary role of surfactant in the alveoli?
What is the primary role of surfactant in the alveoli?
Which of the following conditions would most likely lead to increased stiffness and decreased lung compliance?
Which of the following conditions would most likely lead to increased stiffness and decreased lung compliance?
What occurs during expiration in relation to transpulmonary pressure?
What occurs during expiration in relation to transpulmonary pressure?
Which factor has the greatest influence on airway resistance?
Which factor has the greatest influence on airway resistance?
What happens to airway resistance during forced expiration?
What happens to airway resistance during forced expiration?
What characteristic of respiratory distress syndrome in newborns is primarily caused by surfactant deficiency?
What characteristic of respiratory distress syndrome in newborns is primarily caused by surfactant deficiency?
Which mechanism contributes to airway dilation during inspiration?
Which mechanism contributes to airway dilation during inspiration?
What causes the intrapleural pressure (Pip) to become negative at rest during normal respiratory mechanics?
What causes the intrapleural pressure (Pip) to become negative at rest during normal respiratory mechanics?
What effect does a pneumothorax have on intrapleural pressure (Pip) and transpulmonary pressure (Ptp)?
What effect does a pneumothorax have on intrapleural pressure (Pip) and transpulmonary pressure (Ptp)?
Which muscles are primarily responsible for initiating inspiration during normal resting breathing?
Which muscles are primarily responsible for initiating inspiration during normal resting breathing?
What is the role of transpulmonary pressure (Ptp) in maintaining lung stability at rest?
What is the role of transpulmonary pressure (Ptp) in maintaining lung stability at rest?
During a pneumothorax resulting from a chest wall injury, what happens to the lungs and chest wall?
During a pneumothorax resulting from a chest wall injury, what happens to the lungs and chest wall?
Flashcards are hidden until you start studying
Study Notes
The Respiratory System
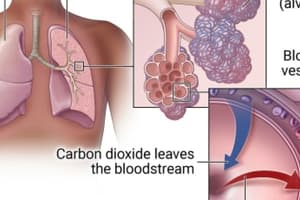
- The respiratory system is responsible for taking in oxygen and expelling carbon dioxide
- Composed of the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles, and alveoli, with the alveoli being the primary sites of gas exchange
- The conducting zone consists of the trachea, bronchi, and bronchioles, which transport air but do not participate in gas exchange
- The respiratory zone includes the respiratory bronchioles, alveolar ducts, and alveolar sacs, which are the sites of gas exchange
- The lungs are divided into lobes and contain approximately 300 million alveoli each
- The right ventricle of the heart pumps blood through the pulmonary arteries into the capillaries surrounding the alveoli
- During inspiration, air travels through the nasal or oral cavity, pharynx, larynx, trachea, bronchi, and bronchioles to the alveoli
- Expiration reverses this process, expelling air from the alveoli through the same pathway
- The airways beyond the larynx are divided into the conducting and respiratory zones
- The conducting zone provides a pathway for airflow, with resistance regulated by bronchiolar smooth muscle
- The conducting zone also protects the lungs from foreign matter through cilia, mucus, and macrophages
- The respiratory zone is the site of gas exchange between the alveoli and pulmonary capillaries
Airway Structure and Function
- The trachea and bronchi contain cartilage rings for structural support
- Bronchioles lack cartilage and rely on smooth muscle to regulate their diameter
- Alveoli are tiny, hollow sacs with thin walls that facilitate rapid gas exchange
- Type I alveolar cells form the primary lining of the alveoli and allow for gas exchange
- Type II alveolar cells produce surfactant, a substance that prevents alveolar collapse
- The capillary network surrounding the alveoli facilitates the rapid exchange of oxygen and carbon dioxide
- Pores between alveoli allow for airflow between adjacent sacs, especially when an airway is blocked
Lung Mechanics and Pleural Sac
- The lungs reside within the thorax, a cavity separated from the abdomen by the diaphragm
- The thoracic wall is formed by the ribs, sternum, spinal column, and intercostal muscles
- The lungs are enclosed in pleural sacs, each consisting of two layers: visceral pleura (lines the lung) and parietal pleura (lines the thoracic wall)
- The pleural sacs are separated by a thin layer of intrapleural fluid, which functions as a lubricant
Principles of Ventilation
- Ventilation is the exchange of air between the atmosphere and alveoli
- Air movement is driven by pressure differences, flowing from high pressure to low pressure
- This flow is governed by the equation: Flow (F) = Pressure difference (ΔP) / Resistance (R)
- The pressure difference is essential for ventilation, with lower pressure in the alveoli drawing air in during inspiration and higher pressure pushing air out during expiration
- Resistance to airflow can be influenced by factors such as bronchiole constriction and the presence of obstructions in the airways
- The mechanics of ventilation involve the interplay of pressures within the alveoli, the pleural space, and the thoracic cavity
Implications of Intrapleural Pressure
- The pressure within the pleural space (intrapleural pressure, Pip) is normally negative relative to atmospheric pressure
- This negative Pip helps to keep the lungs inflated and prevents their collapse
- Changes in Pip are crucial for ventilation, with a decrease in Pip during inspiration expanding the lungs and an increase in Pip during expiration allowing the lungs to recoil
- The interplay of pressures and lung compliance (ability of the lung to stretch) determines the volume changes during ventilation
Overview of Respiratory Physiology
- Understanding the interaction of pressures, volumes, and resistances is necessary to appreciate the various functions of the respiratory system
- The respiratory system plays a crucial role in maintaining homeostasis and providing oxygen to the body while removing carbon dioxide
- The lungs serve as the primary site of gas exchange, with the thin alveolar walls facilitating the efficient transfer of oxygen and carbon dioxide between the air and blood
- The structure of the respiratory system, particularly the alveolar network, is intricately linked to its function in gas exchange
- This intricate system relies on a complex interplay of physical laws, physiological processes, and neural control to maintain the oxygen and carbon dioxide balance in the body
- Abnormalities in any of these aspects can lead to respiratory dysfunction, highlighting the importance of understanding this complex interplay for both normal and diseased states.
Airflow and Pressure
- Airflow into and out of the lungs is determined by the pressure difference between the alveoli (Palv) and the atmosphere (Patm).
- When Palv is less than Patm, air flows into the lungs (inspiration).
- When Palv is greater than Patm, air flows out of the lungs (expiration).
- These pressure changes are driven by changes in the dimensions of the chest wall and lungs.
Boyle's Law
- Boyle's law states that the pressure of a gas is inversely proportional to its volume (at constant temperature).
- An increase in lung volume decreases alveolar pressure, causing inspiration.
- A decrease in lung volume increases alveolar pressure, causing expiration.
Transpulmonary Pressure (Ptp)
- Ptp is the difference in pressure between the inside and outside of the lung.
- Ptp = Palv - Pip (where Pip is intrapleural pressure).
- Ptp is the pressure that governs the static properties of the lungs.
Transmural Pressures
- Transmural pressure is the pressure across a wall, calculated as the pressure inside the structure (Pin) minus the pressure outside the structure (Pout).
- Ptp is one of the major transmural pressures of the respiratory system.
- Ptp is responsible for holding the lungs open.
- Chest wall pressure is another important transmural pressure, holding the chest wall in.
Intrapleural Pressure (Pip)
- Pip is negative relative to atmospheric pressure at rest.
- The negative Pip is created by the elastic recoil of the lungs and chest wall.
- The lungs tend to collapse due to their elastic recoil.
- The chest wall tends to expand due to its elastic recoil.
- These opposing forces create the subatmospheric Pip.
Pneumothorax
- A pneumothorax occurs when air enters the intrapleural space.
- This equalizes the pressure inside and outside the lung, causing the lung to collapse.
- Can occur due to a hole in the chest wall or lung tissue.
- A pneumothorax can be treated by re-expanding the collapsed lung, which requires increasing Ptp by increasing Pip relative to Palv.
Inspiration
- Inspiration is initiated by contraction of the diaphragm and external intercostal muscles.
- Contraction of the diaphragm moves it downwards, increasing thoracic volume.
- Contraction of the external intercostal muscles raises and expands the rib cage, further increasing thoracic volume.
- This increase in thoracic volume lowers Pip, making Ptp more positive and expanding the lungs.
- Expansion of the lungs causes alveolar pressure to decrease, allowing air to flow into the alveoli.
Expiration
- Expiration at rest is passive.
- Relaxation of the inspiratory muscles allows the chest wall and lungs to recoil inward.
- This recoil increases Pip, decreasing Ptp and causing the lungs to collapse.
- Collapse of the lungs compresses the air in the alveoli, increasing alveolar pressure and causing air to flow out of the lungs.
- During active expiration (e.g., exercise), the internal intercostal muscles and abdominal muscles contract to further decrease thoracic volume.
Lung Compliance
- Lung compliance describes the stretchability of the lungs.
- Higher compliance means the lungs expand more easily for a given change in Ptp.
- Lung compliance is an important aspect of lung mechanics.
Lung Compliance
- Lung compliance is the change in lung volume divided by the change in transpulmonary pressure
- Greater lung compliance means easier lung expansion
- Low lung compliance means lungs are stiff and require a larger transpulmonary pressure to expand
- Thickening of lung tissues decreases lung compliance
- Surface tension of water lining alveoli is a major determinant of lung compliance
Surface Tension
- Surface tension resists lung expansion
- Surfactant is a detergent-like substance secreted by type II alveolar cells that reduces surface tension, increasing lung compliance
- Surfactant is a mixture of lipids and proteins, primarily a phospholipid
- Deep breaths increase surfactant secretion
- Respiratory distress syndrome of the newborn is caused by surfactant deficiency
Law of Laplace
- Pressure in an alveolus is directly proportional to surface tension and inversely proportional to the radius of the alveolus
- Surfactant stabilizes alveoli of different sizes by altering surface tension
Airway Resistance
- Airway Resistance is inversely proportional to the fourth power of the airway radius
- Transpulmonary pressure plays a key role in preventing airway collapse, increasing with inspiration
- Lateral traction also helps to hold airways open during inspiration
- Forced expiration increases airway resistance
Asthma
- Characterized by intermittent episodes of airway smooth muscle contraction, increasing airway resistance
- Underlying cause is chronic airway inflammation
- Triggers can include exercise, tobacco smoke, environmental pollutants, allergens, and viruses
Chronic Obstructive Pulmonary Disease (COPD)
- Includes emphysema and chronic bronchitis
- Emphysema is caused by damage to and collapse of smaller airways
- Chronic bronchitis is characterized by excessive mucus production and inflammatory changes in the airways
Lung Volumes and Capacities
- Tidal Volume (Vt): Volume of air entering the lungs during a single inspiration
- Resting Tidal Volume: Vt during quiet breathing (about 500 mL)
- Inspiratory Reserve Volume (IRV): Maximal volume of air that can be inspired above TV (about 3000 mL)
- Functional Residual Capacity (FRC): Amount of air remaining in the lungs after a resting expiration (about 2400 mL)
- Expiratory Reserve Volume (ERV): Maximal volume of air that can be expired after a resting expiration (about 1200 mL)
- Residual Volume (RV): Amount of air remaining in the lungs after maximal expiration (about 1200 mL)
- Vital Capacity (VC): Maximal volume of air that can be expired after a maximal inspiration (sum of IRV, TV, and ERV)
- Forced Expiratory Volume in 1 second (FEV1): Maximum amount of air expired in 1 second after a full inspiration
Pulmonary Function Tests
- Measure lung volumes and capacities, such as VC and FEV1
- Obstructive lung diseases typically have a decreased FEV1
- Restrictive lung diseases are characterized by a reduced VC but a normal FEV1/VC ratio
Alveolar Ventilation
- Minute Ventilation (V˙E): Total ventilation per minute, calculated by multiplying tidal volume by respiratory rate
- Dead Space: Volume of inspired air that does not participate in gas exchange
- Anatomic Dead Space: Volume of the conducting airways (about 150 mL)
- Only air that reaches the alveoli contributes to gas exchange
Understanding the Respiratory System
- Anatomical dead space refers to the airways that don't participate in gas exchange with the blood.
- The volume of fresh air entering the alveoli is calculated by subtracting the anatomical dead space volume from the tidal volume.
- Alveolar ventilation is the total volume of fresh air entering the alveoli per minute.
- Alveolar ventilation is more important than minute ventilation for effective gas exchange.
- Increased depth of breathing is more effective in increasing alveolar ventilation than an increased breathing rate.
- Alveolar dead space refers to alveoli with little or no blood supply, which can be significant in lung diseases.
- Physiological dead space is the sum of anatomical and alveolar dead spaces.
Gas Exchange in Alveoli and Tissues
- Oxygen moves from the alveoli to the blood, then to tissues, and finally into cells.
- Carbon dioxide follows a reverse path, moving from cells to blood, then to the lungs, and finally into the atmosphere.
- The rate of oxygen consumption by cells equals the rate of oxygen added to blood in the lungs.
- The rate of carbon dioxide production by the cells equals the rate of carbon dioxide leaving the blood in the lungs.
- The respiratory quotient (RQ) is the ratio of CO2 produced to O2 consumed.
- It varies for different nutrients: 1 for carbohydrates, 0.7 for fats, and 0.8 for proteins.
- The RQ for a mixed diet is approximately 0.8.
Partial Pressures of Gases
- Dalton's Law states that the total pressure of a gas mixture is the sum of the individual partial pressures of each gas.
- Partial pressure (P) refers to the pressure exerted by individual gases in a mixture.
- Net diffusion of a gas occurs from an area of higher partial pressure to lower partial pressure.
Diffusion of Gases in Liquids
- Henry's Law states that the amount of gas dissolved in a liquid is directly proportional to its partial pressure.
- Diffusional equilibrium is reached when the partial pressure of the gas in the liquid and gaseous phases are equal.
Alveolar Gas Pressures
- Typical alveolar gas pressures are PO2 = 105 mmHg and PCO2 = 40 mmHg.
- Alveolar PO2 is lower than atmospheric PO2 due to the oxygen entering the pulmonary capillaries.
- Alveolar PCO2 is higher than atmospheric PCO2 due to carbon dioxide entering the alveoli from the pulmonary capillaries.
- Factors determining alveolar PO2 are the PO2 of inspired air, alveolar ventilation rate, and total body oxygen consumption.
- Decreased alveolar ventilation lowers alveolar PO2.
- Increased oxygen consumption lowers alveolar PO2.
- Opposite effects apply for increasing alveolar PO2.
- Alveolar PCO2 is influenced by alveolar ventilation rate.
- Decreased alveolar ventilation increases alveolar PCO2.
- Increased alveolar ventilation lowers alveolar PCO2.
Factors Affecting Alveolar Gas Pressures:
- Breathing air with low PO2 decreases alveolar PO2, while alveolar PCO2 remains unchanged.
- Decreased alveolar ventilation decreases alveolar PO2 and increases alveolar PCO2.
- Increased metabolism decreases alveolar PO2 and increases alveolar PCO2.
- Proportional increases in metabolism and alveolar ventilation keep alveolar PO2 and PCO2 unchanged.
Alveolar Ventilation and Partial Pressure
- Changes in alveolar ventilation affect alveolar partial pressure of O2 and CO2
- Increasing alveolar ventilation decreases PCO2 and increases PO2
- Decreasing alveolar ventilation increases PCO2 and decreases PO2
- Increased production of CO2 increases alveolar PCO2
- Increased consumption of O2 decreases alveolar PO2
Ventilation/Perfusion Matching
- Ventilation and perfusion are critical for efficient gas exchange in the lungs
- Mismatches between ventilation and perfusion lead to decreased arterial PO2
- The major disease-induced cause of inadequate O2 movement is ventilation/perfusion mismatch
- In healthy people, small amounts of ventilation/perfusion mismatch occur due to gravity
- Disease states can cause marked ventilation/perfusion inequalities
- Ventilation/perfusion inequalities can lead to wasted ventilation or shunting of blood
Homeostatic Control of Ventilation/Perfusion Matching
- Local mechanisms within the lungs help minimize ventilation/perfusion mismatch
- Low PO2 within alveoli causes vasoconstriction, diverting blood away from poorly ventilated areas
- Decreased blood flow within a lung region causes local bronchoconstriction to divert airflow away from poorly perfused areas
Gas Exchange Between Tissues and Blood
- The body's PO2 gradient: alveoli to blood to cells
- The body's PCO2 gradient: cells to blood to alveoli
- O2 is consumed by cells during metabolism
- CO2 is produced by cells during metabolism
- These gradients drive diffusion of gases
Transport of Oxygen in Blood
- Systemic arterial blood normally contains 200 mL of O2 per liter
- Oxygen is transported in two forms: dissolved in plasma and erythrocytes and reversibly combined with hemoglobin in erythrocytes
- The amount of O2 dissolved in blood is directly proportional to PO2
- Hemoglobin consists of four subunits, each containing one heme group with an iron atom that binds one oxygen molecule
- Percent hemoglobin saturation is the fraction of hemoglobin molecules bound to oxygen
- Percent hemoglobin saturation is primarily determined by blood PO2
- Anemia is a decrease in hemoglobin content in blood
Oxygen-Hemoglobin Dissociation Curve
- The oxygen-hemoglobin dissociation curve describes the relationship between PO2 and hemoglobin saturation
- The curve is sigmoid due to cooperative binding of oxygen to hemoglobin subunits
- The steep slope between 10 and 60 mmHg PO2 reflects increased oxygen binding as PO2 increases
- The plateau portion between 70 and 100 mmHg PO2 shows that a further increase in PO2 has little effect on oxygen binding
- The plateau is important for oxygen delivery, ensuring adequate oxygen saturation even at lower PO2 values in some conditions
- Total oxygen transport is influenced by both hemoglobin saturation and hemoglobin concentration in blood
Hemoglobin Saturation and Oxygen Transport
- Hemoglobin saturation remains high even with reduced oxygen pressure (PO2).
- Even with a drop from 100 to 60 mmHg PO2, only a 10% decrease in oxygen carried by hemoglobin occurs due to the plateau effect.
- The plateau in the oxygen dissociation curve ensures sufficient oxygen saturation despite moderate lung function limitations.
- Hyperventilation or breathing 100% oxygen at sea level in healthy individuals does not significantly increase blood oxygen content.
- Hemoglobin is nearly fully saturated at normal arterial PO2 (100 mmHg), preventing further oxygen uptake even with increased PO2.
- This principle applies to healthy individuals at sea level.
- Individuals with lung disease or those at high altitude who have lower arterial PO2 initially, will have a greater capacity for oxygen uptake with increased PO2.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.