Podcast
Questions and Answers
What is the effect of surfactant in smaller alveoli when the pressure is higher in larger alveoli?
What is the effect of surfactant in smaller alveoli when the pressure is higher in larger alveoli?
- It increases the pressure in the smaller alveoli.
- It has no effect on alveoli pressure.
- It prevents air flow from larger to smaller alveoli. (correct)
- It causes smaller alveoli to collapse into larger ones.
The tidal volume (TV) is the amount of air inhaled or exhaled in one breath.
The tidal volume (TV) is the amount of air inhaled or exhaled in one breath.
True (A)
What happens to air flow between two alveoli when Ta is equal to Tb without surfactant?
What happens to air flow between two alveoli when Ta is equal to Tb without surfactant?
Air flows from b to a.
Surfactant helps to stabilize smaller alveoli by reducing the _____ difference between them.
Surfactant helps to stabilize smaller alveoli by reducing the _____ difference between them.
Match the following terms with their definitions:
Match the following terms with their definitions:
Which process involves the movement of air into the alveoli during breathing?
Which process involves the movement of air into the alveoli during breathing?
The primary function of the respiratory system is to eliminate oxygen from the body.
The primary function of the respiratory system is to eliminate oxygen from the body.
What is the process of gas exchange between alveolar air and blood in lung capillaries called?
What is the process of gas exchange between alveolar air and blood in lung capillaries called?
The __________ zone of the respiratory system consists of bronchioles, alveolar ducts, and alveoli.
The __________ zone of the respiratory system consists of bronchioles, alveolar ducts, and alveoli.
Match the following respiratory processes with their descriptions:
Match the following respiratory processes with their descriptions:
Which of the following plays a role in voice production?
Which of the following plays a role in voice production?
The respiratory system functions only in gas exchange.
The respiratory system functions only in gas exchange.
What is the term for the phase of the respiratory cycle when air moves from the alveoli to the external environment?
What is the term for the phase of the respiratory cycle when air moves from the alveoli to the external environment?
What is the primary driver for gas diffusion at the alveoli and cells?
What is the primary driver for gas diffusion at the alveoli and cells?
The atmosphere contains more carbon dioxide than alveolar gas.
The atmosphere contains more carbon dioxide than alveolar gas.
What gas diffuses from the alveoli into the bloodstream?
What gas diffuses from the alveoli into the bloodstream?
According to Henry's law, the concentration of a dissolved gas is equal to the partial pressure of the gas above the fluid multiplied by its __________ in that fluid.
According to Henry's law, the concentration of a dissolved gas is equal to the partial pressure of the gas above the fluid multiplied by its __________ in that fluid.
Match the following partial pressures with their corresponding locations:
Match the following partial pressures with their corresponding locations:
What is the primary muscle used in inspiration that flattens to increase the thoracic cavity volume?
What is the primary muscle used in inspiration that flattens to increase the thoracic cavity volume?
Expiration involves air entering the lungs.
Expiration involves air entering the lungs.
What happens to the pressure in the lungs when the volume of the thoracic cavity decreases?
What happens to the pressure in the lungs when the volume of the thoracic cavity decreases?
The phase of ventilation in which air enters the lungs is called ______.
The phase of ventilation in which air enters the lungs is called ______.
Match the following phases of ventilation with their correct descriptions:
Match the following phases of ventilation with their correct descriptions:
Which statement is true regarding the relationship between volume and pressure according to Boyle's law?
Which statement is true regarding the relationship between volume and pressure according to Boyle's law?
What role does the pleural fluid play during breathing?
What role does the pleural fluid play during breathing?
The external intercostal muscles depress the ribs during inspiration.
The external intercostal muscles depress the ribs during inspiration.
What percentage of carbon dioxide is transported in plasma as bicarbonate ions?
What percentage of carbon dioxide is transported in plasma as bicarbonate ions?
Fetal hemoglobin has a lower affinity for oxygen compared to adult hemoglobin.
Fetal hemoglobin has a lower affinity for oxygen compared to adult hemoglobin.
What is the enzyme responsible for converting carbon dioxide into bicarbonate in red blood cells?
What is the enzyme responsible for converting carbon dioxide into bicarbonate in red blood cells?
Carbon dioxide is approximately __% dissolved in plasma.
Carbon dioxide is approximately __% dissolved in plasma.
Match the following forms of carbon dioxide transport with their corresponding percentages:
Match the following forms of carbon dioxide transport with their corresponding percentages:
What effect does increased carbon dioxide in blood have on oxygen dissociation from hemoglobin?
What effect does increased carbon dioxide in blood have on oxygen dissociation from hemoglobin?
The chloride shift occurs to balance the movement of bicarbonate ions out of red blood cells.
The chloride shift occurs to balance the movement of bicarbonate ions out of red blood cells.
What happens to bicarbonate ions at the lungs?
What happens to bicarbonate ions at the lungs?
What is the primary role of the diaphragm during breathing?
What is the primary role of the diaphragm during breathing?
The primary function of the respiratory system is to transport carbon dioxide into the blood.
The primary function of the respiratory system is to transport carbon dioxide into the blood.
What process describes the movement of air out of the lungs?
What process describes the movement of air out of the lungs?
The ______ membrane is specialized for gas diffusion in the lungs.
The ______ membrane is specialized for gas diffusion in the lungs.
Match the following gas transport forms with their corresponding percentages:
Match the following gas transport forms with their corresponding percentages:
Which of the following best describes the influence of increased carbon dioxide levels in blood on the release of oxygen from hemoglobin?
Which of the following best describes the influence of increased carbon dioxide levels in blood on the release of oxygen from hemoglobin?
What percentage of oxygen in the blood is bound to hemoglobin?
What percentage of oxygen in the blood is bound to hemoglobin?
What is the primary role of surfactant in the lungs?
What is the primary role of surfactant in the lungs?
Reduced hemoglobin is formed when hemoglobin releases oxygen.
Reduced hemoglobin is formed when hemoglobin releases oxygen.
What is the term for the hemoglobin-oxygen combination?
What is the term for the hemoglobin-oxygen combination?
Increased mucus production narrows the lumen and decreases resistance in air passages.
Increased mucus production narrows the lumen and decreases resistance in air passages.
The respiratory membrane is typically _______ thick, allowing for efficient gas exchange.
The respiratory membrane is typically _______ thick, allowing for efficient gas exchange.
What type of receptors does parasympathetic innervation mainly work on to induce bronchoconstriction?
What type of receptors does parasympathetic innervation mainly work on to induce bronchoconstriction?
Surfactant helps to maintain similar alveolar sizes and reduces lung _____ and transudation.
Surfactant helps to maintain similar alveolar sizes and reduces lung _____ and transudation.
Match the following types of hemoglobin with their descriptions:
Match the following types of hemoglobin with their descriptions:
Which of the following mediators released by inflammatory cells can increase mucus production in asthma?
Which of the following mediators released by inflammatory cells can increase mucus production in asthma?
Which of the following factors does NOT significantly influence the dissociation of oxygen from hemoglobin?
Which of the following factors does NOT significantly influence the dissociation of oxygen from hemoglobin?
Match the following components with their functions:
Match the following components with their functions:
Surfactant increases the effort required for lung inflation.
Surfactant increases the effort required for lung inflation.
What is the relationship between surface tension and lung compliance?
What is the relationship between surface tension and lung compliance?
What is the main purpose of a spirometer?
What is the main purpose of a spirometer?
Anatomical dead space refers to the volume of air that undergoes gas exchange with blood.
Anatomical dead space refers to the volume of air that undergoes gas exchange with blood.
What is the total volume of inhaled air that is not exchanged, known as the sum of anatomic and alveolar dead space?
What is the total volume of inhaled air that is not exchanged, known as the sum of anatomic and alveolar dead space?
The average anatomical dead space is approximately __ mL out of the tidal volume of 500 mL.
The average anatomical dead space is approximately __ mL out of the tidal volume of 500 mL.
Match the following components of lung mechanics with their descriptions:
Match the following components of lung mechanics with their descriptions:
What occurs during pulmonary ventilation?
What occurs during pulmonary ventilation?
Alveolar dead space refers to a volume of inhaled air that enters alveoli with adequate blood supply.
Alveolar dead space refers to a volume of inhaled air that enters alveoli with adequate blood supply.
What is the primary driver for movement of air into the lungs during inspiration?
What is the primary driver for movement of air into the lungs during inspiration?
The process in which the air enters the alveoli during breathing is known as _____.
The process in which the air enters the alveoli during breathing is known as _____.
Which statement about lung mechanics is correct?
Which statement about lung mechanics is correct?
Flashcards are hidden until you start studying
Study Notes
Respiratory System Functions
- Supplies the body with oxygen and eliminates carbon dioxide
- Regulates blood pH in coordination with the kidneys
- Voice production (phonation)
- Olfaction (smell)
- Protection against inhaled microorganisms
Respiration Processes
- Pulmonary ventilation (breathing): movement of air into and out of the lungs
- External respiration: gas exchange between the alveolar air and blood in lung capillaries
- Transport: transport of oxygen and carbon dioxide in the blood
- Internal respiration: gas exchange between blood in tissue capillaries and cells in tissues
Respiration Definitions
- Internal or cellular respiration: the utilization of oxygen in the metabolism of organic molecules
- Pulmonary physiology: the exchange of oxygen and carbon dioxide between an organism and the external environment
Respiratory Cycle Phases
- Inspiration (inhalation): movement of air from the external environment through the airways into the alveoli
- Expiration (exhalation): movement of air from the alveoli through the airways into the external environment
Respiration Steps
- Ventilation: Exchange of air between atmosphere and alveoli by bulk flow
- Exchange of O2 and CO2 between alveolar air and blood in lung capillaries by diffusion
- Transport of O2 and CO2 through pulmonary and systemic circulation by bulk flow
- Exchange of O2 and CO2 between blood in tissue capillaries and cells in tissues by diffusion
- Cellular utilization of O2 and production of CO2
Respiratory System Organization
- Respiratory zone: site of gas exchange (bronchioles, alveolar ducts, and alveoli)
- Conducting zone: provides conduits for air to reach the respiratory zone (all other respiratory structures)
Lung Volumes & Capacities
- Tidal volume (TV): Amount of air inhaled or exhaled in one breath (0.3 - 0.5 L)
- Inspiratory reserve volume (IRV): Amount of air that can be forcefully inhaled after a normal tidal volume inhalation (2.1 - 3.2 L)
- Expiratory reserve volume (ERV): Amount of air that can be forcefully exhaled after a normal tidal volume exhalation (1.0 - 1.2 L)
- Residual volume (RV): Amount of air remaining in the lungs after a forceful exhalation (1.2 L)
Lung and Breathing
- The pleural space contains pleural fluid, forming a seal that holds the lungs against the thoracic wall.
- Changes in thoracic cavity volume alter lung volume, affecting internal pressure.
- Boyle's law: volume of gas is inversely proportional to pressure (at constant temperature).
Inspiration
- Contraction of inspiratory muscles (diaphragm and external intercostal muscles) increases thoracic cavity volume.
- Increased lung volume decreases internal pressure, drawing air into the lungs down the pressure gradient.
Passive Expiration
- Relaxation of inspiratory muscles allows elastic recoil of lungs and thoracic cage, decreasing thoracic cavity volume.
- Increased internal pressure expels air out of the lungs.
Gas Exchange
- Gases move from areas of high partial pressures to areas of low partial pressure.
- Venous blood has the same PO2 as tissues.
Factors Affecting Gas Diffusion Rate
- Concentration gradient: higher gradient, faster diffusion.
- Surface area for diffusion: larger area, faster diffusion.
- Length of diffusion pathway: shorter pathway, faster diffusion.
Gas Exchange at the Alveoli
- Oxygen diffuses from alveoli to blood.
- Carbon dioxide diffuses from blood to alveoli.
- Alveolar gas composition differs from atmospheric due to gas exchange, humidification, and mixing.
Transport of Oxygen in Blood
- Dissolved in plasma: 1.5%
- Bound to hemoglobin: 98.5%
- Hemoglobin saturation with oxygen increases with increasing partial pressure of oxygen (pO2).
Carbon Dioxide Transport in Blood
- Dissolved in plasma: 7-10%
- Bound to hemoglobin: 20% (carbaminohemoglobin)
- Bicarbonate ion in plasma: 70%
Transport and Exchange of Carbon Dioxide
- At the tissues:
- More carbon dioxide enters the blood.
- More oxygen dissociates from hemoglobin (Bohr effect).
- More carbon dioxide combines with hemoglobin, and more bicarbonate ions are formed.
- Bicarbonate diffuses from RBCs into the plasma.
- Chloride shift: chloride ions move from the plasma into RBCs to balance the outflux of bicarbonate ions.
- At the lungs:
- The process reverses.
- Bicarbonate ions move into the RBCs and bind with hydrogen ions to form carbonic acid.
- Carbonic acid is split into carbon dioxide and water by carbonic anhydrase.
- Carbon dioxide diffuses from the blood into the alveoli.
Regulation of Respiration
- Voluntary control: cerebral cortex (conscious control)
- Automatic control: medulla and pons (unconscious control)
Respiratory Centers in the Brain
- Medullary rhythmicity center: sets basic breathing rhythm.
- Pons: fine-tunes breathing rhythm and depth.
- Pneumotaxic center: inhibits inspiration, making it shorter.
- Apneustic center: promotes inspiration, making it longer.
Factors Influencing Breathing Rate and Depth
- Chemical factors:
- Carbon dioxide: increases in blood CO2 stimulate breathing.
- Oxygen: decreases in blood O2 stimulate breathing (but less effective than CO2).
- Hydrogen ions: increases in blood H+ stimulate breathing.
- Other factors:
- Proprioceptors: sense joint movement and muscle position, influencing breathing during exercise.
- Irritants: dust, smoke, and other irritants in airways stimulate breathing.
- Emotions: stress and anxiety increase breathing rate and depth.
Key Points
- The respiratory system provides oxygen to the body and eliminates carbon dioxide.
- Respiration involves four processes: pulmonary ventilation, external respiration, transport, and internal respiration.
- Gas exchange occurs in the alveoli, driven by partial pressure gradients.
- Oxygen is transported in the blood primarily bound to hemoglobin, while carbon dioxide is transported in multiple forms: dissolved in plasma, bound to hemoglobin, and as bicarbonate ions.
- Breathing is regulated by automatic and voluntary controls involving respiratory centers in the brain.
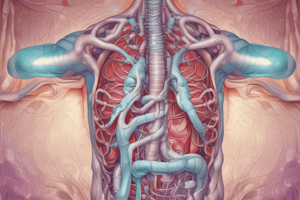
Respiratory System Structure and Function
-
The respiratory system is responsible for gas exchange, allowing oxygen to enter the bloodstream and carbon dioxide to be removed.
-
The lungs, thorax (chest cavity), and airways are crucial components.
-
The diaphragm and other respiratory muscles control breathing, expanding and contracting the thoracic cavity.
-
The alveolar capillary membrane, thin and large in surface area, facilitates efficient gas diffusion between alveoli and blood.
-
Inspiration (inhaling) draws air into the lungs, while expiration (exhaling) releases air.
Airway Resistance
-
Airway resistance is influenced by the diameter of the airways, which can be affected by various factors:
-
Bronchoconstrictors: Parasympathetic nervous system stimulation through muscarinic receptors constricts smooth muscle in the airways, reducing diameter. This can be triggered by irritants, inflammation, and release of mediators like histamine and leukotrienes.
-
Mucus Production: Increased mucus production in asthma narrows the lumen and increases resistance.
-
Surfactant
-
Surfactant, secreted by type II alveolar cells, reduces surface tension in the alveoli, enhancing lung function:
-
Increases Compliance: Surfactant makes the lungs easier to inflate by reducing the surface tension that hinders lung distensibility.
-
Keeps Lungs Dry: Surfactant helps prevent fluid buildup in the alveoli, which could interfere with gas exchange.
-
Lung Volumes and Capacities
-
Spirometer: A device used to measure lung volumes and capacities.
-
Dead Spaces: Areas in the respiratory system where gas exchange doesn't occur:
-
Anatomic Dead Space: The volume of air in the conducting airways (e.g., trachea, bronchi) that doesn't reach the alveoli (~150 mL out of a typical tidal volume of 500 mL).
-
Alveolar Dead Space: The volume of air in alveoli that lack adequate blood supply, leading to minimal gas exchange (normally minimal but can increase with lung diseases).
-
Physiologic Dead Space: The combined volume of anatomic and alveolar dead space, representing wasted ventilation.
-
Mechanics of Breathing
-
External Respiration (Pulmonary Gas Exchange): The process of oxygen and carbon dioxide movement across the respiratory membrane:
-
Partial Pressure Gradients & Gas Solubilities: Differences in partial pressures of oxygen and carbon dioxide drive their movement across the membrane, influenced by their solubilities.
-
Structural Characteristics of the Respiratory Membrane: The membrane's thinness (0.5-1 µm), large surface area (~50-70 m2 in males), and potential for thickening due to edema or emphysema affect gas exchange efficiency.
-
Transport of Oxygen in Blood
-
Hemoglobin (Hb): The primary carrier of oxygen in the blood. It's found in red blood cells (RBCs) and reversibly binds oxygen molecules.
-
Oxyhemoglobin (HbO2): Hemoglobin with bound oxygen.
-
Reduced Hemoglobin (HHb): Hemoglobin that has released oxygen.
-
-
Hemoglobin Saturation Curve: Illustrates the relationship between oxygen partial pressure (PO2) and hemoglobin saturation. At higher PO2, hemoglobin becomes almost fully saturated.
Factors Influencing Hemoglobin Saturation
-
PO2: The partial pressure of oxygen in the blood is the primary factor influencing hemoglobin saturation.
-
pH: Blood pH affects hemoglobin's affinity for oxygen. Lower pH (more acidic) promotes oxygen release.
-
Temperature: Higher temperatures increase oxygen release from hemoglobin.
-
2,3-Diphosphoglycerate (2,3-DPG): An organic phosphate in red blood cells that decreases hemoglobin's affinity for oxygen, facilitating oxygen delivery to tissues.
Control of Respiration
-
Neural Control: Breathing is regulated by the respiratory centers in the brainstem (medulla oblongata and pons).
-
Chemoreceptors: Specialized sensory cells that detect chemical changes in the blood:
-
Central Chemoreceptors: Located in the medulla oblongata, they primarily detect changes in CO2 and H+ concentration in cerebrospinal fluid.
-
Peripheral Chemoreceptors: Located in the carotid and aortic bodies, they sense changes in PO2, PCO2, and H+ in arterial blood.
-
-
Mechanoreceptors: Sensory receptors located in the airways:
-
Stretch Receptors: Located in the bronchial walls, they respond to lung inflation, inhibiting inspiration and contributing to the Hering-Breuer inspiratory reflex.
-
Juxtapulmonary Receptors: Located on the alveolar and bronchial walls, they respond to various stimuli like fluid buildup, edema, or inflammation, leading to shallow breathing or apnea.
-
Irritant Receptors: Located throughout the airways, they trigger coughing or rapid breathing in response to irritants like smoke or dust.
-
-
Proprioceptors: Located in muscles and joints, they provide information about body position and movement, influencing breathing effort, especially during exercise.
-
Factors Affecting Breathing: Various factors can influence breathing patterns, including exercise, emotional state, and chemical changes (CO2, O2, H+).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.