Podcast
Questions and Answers
Which of the following is NOT a major subdivision of the digestive tract?
Which of the following is NOT a major subdivision of the digestive tract?
What is the primary function of the salivary glands in the digestive system?
What is the primary function of the salivary glands in the digestive system?
What is peristalsis?
What is peristalsis?
Which function of the digestive system is responsible for the breakdown of food into smaller components?
Which function of the digestive system is responsible for the breakdown of food into smaller components?
Signup and view all the answers
Which of the following neurotransmitters primarily excites gastrointestinal activity?
Which of the following neurotransmitters primarily excites gastrointestinal activity?
Signup and view all the answers
What is the role of the large intestine in the digestive system?
What is the role of the large intestine in the digestive system?
Signup and view all the answers
Which of the following processes involves the movement of food through the alimentary tract?
Which of the following processes involves the movement of food through the alimentary tract?
Signup and view all the answers
Which organ is responsible for the storage of bile in the digestive system?
Which organ is responsible for the storage of bile in the digestive system?
Signup and view all the answers
What is primarily secreted by the mucous neck cells in the stomach?
What is primarily secreted by the mucous neck cells in the stomach?
Signup and view all the answers
Which type of cell in the stomach secretes pepsinogen?
Which type of cell in the stomach secretes pepsinogen?
Signup and view all the answers
What causes local epithelial stimulation in the gastrointestinal tract?
What causes local epithelial stimulation in the gastrointestinal tract?
Signup and view all the answers
Which substance is NOT a characteristic of the gastric secretions?
Which substance is NOT a characteristic of the gastric secretions?
Signup and view all the answers
What is the role of hydrochloric acid in the stomach?
What is the role of hydrochloric acid in the stomach?
Signup and view all the answers
Which glands are considered the principal salivary glands?
Which glands are considered the principal salivary glands?
Signup and view all the answers
What is the primary function of esophageal secretions?
What is the primary function of esophageal secretions?
Signup and view all the answers
What type of stimuli activates the enteric nervous system of the gut wall?
What type of stimuli activates the enteric nervous system of the gut wall?
Signup and view all the answers
What forms do most proteins take when absorbed through intestinal epithelial cells?
What forms do most proteins take when absorbed through intestinal epithelial cells?
Signup and view all the answers
What mechanism provides energy for the absorption of most proteins?
What mechanism provides energy for the absorption of most proteins?
Signup and view all the answers
What percentage of fat is absorbed in the presence of bile micelles?
What percentage of fat is absorbed in the presence of bile micelles?
Signup and view all the answers
What is a characteristic of the absorption of short- and medium-chain fatty acids?
What is a characteristic of the absorption of short- and medium-chain fatty acids?
Signup and view all the answers
What happens to fat absorption in the absence of bile micelles?
What happens to fat absorption in the absence of bile micelles?
Signup and view all the answers
What is the primary ion secreted by parietal cells to form hydrochloric acid?
What is the primary ion secreted by parietal cells to form hydrochloric acid?
Signup and view all the answers
What is the approximate pH of the hydrochloric acid secreted by parietal cells?
What is the approximate pH of the hydrochloric acid secreted by parietal cells?
Signup and view all the answers
Which process allows hydrogen ions to replace potassium ions in the canaliculus?
Which process allows hydrogen ions to replace potassium ions in the canaliculus?
Signup and view all the answers
What role does carbonic anhydrase play in the secretion process of HCl?
What role does carbonic anhydrase play in the secretion process of HCl?
Signup and view all the answers
What happens to pepsinogen when it comes in contact with hydrochloric acid?
What happens to pepsinogen when it comes in contact with hydrochloric acid?
Signup and view all the answers
What is the function of intrinsic factor secreted by parietal cells?
What is the function of intrinsic factor secreted by parietal cells?
Signup and view all the answers
What type of cells are primarily found in the pyloric glands?
What type of cells are primarily found in the pyloric glands?
Signup and view all the answers
How is sodium reabsorbed by parietal cells during HCl secretion?
How is sodium reabsorbed by parietal cells during HCl secretion?
Signup and view all the answers
What role do peptidases play in digestion?
What role do peptidases play in digestion?
Signup and view all the answers
Which enzymes are responsible for breaking down disaccharides?
Which enzymes are responsible for breaking down disaccharides?
Signup and view all the answers
What does cholesterol-ester-hydrolase specifically hydrolyze?
What does cholesterol-ester-hydrolase specifically hydrolyze?
Signup and view all the answers
How much fluid is typically absorbed per day by the intestines?
How much fluid is typically absorbed per day by the intestines?
Signup and view all the answers
Which secretion in the large intestine protects the intestinal wall?
Which secretion in the large intestine protects the intestinal wall?
Signup and view all the answers
What type of cells secrete mucins in the intestinal mucosa?
What type of cells secrete mucins in the intestinal mucosa?
Signup and view all the answers
What is the purpose of the alkalinity of the large intestine's secretions?
What is the purpose of the alkalinity of the large intestine's secretions?
Signup and view all the answers
Which enzyme is involved in the hydrolysis of phospholipids?
Which enzyme is involved in the hydrolysis of phospholipids?
Signup and view all the answers
What is the primary mechanism for glucose absorption in the small intestine?
What is the primary mechanism for glucose absorption in the small intestine?
Signup and view all the answers
Which of the following statements about sodium absorption in the intestine is correct?
Which of the following statements about sodium absorption in the intestine is correct?
Signup and view all the answers
What significantly enhances calcium absorption in the intestines?
What significantly enhances calcium absorption in the intestines?
Signup and view all the answers
How does the structure of the small intestine enhance its absorptive capacity?
How does the structure of the small intestine enhance its absorptive capacity?
Signup and view all the answers
Which ions are mostly actively absorbed in the small intestine?
Which ions are mostly actively absorbed in the small intestine?
Signup and view all the answers
Approximately what percentage of carbohydrate calories absorbed in the small intestine comes from glucose?
Approximately what percentage of carbohydrate calories absorbed in the small intestine comes from glucose?
Signup and view all the answers
What typically happens to sodium reserves during extreme diarrhea?
What typically happens to sodium reserves during extreme diarrhea?
Signup and view all the answers
Which of the following monosaccharides is the least abundant in absorption?
Which of the following monosaccharides is the least abundant in absorption?
Signup and view all the answers
Study Notes
Digestive System, Digestion, and Absorption of Food
- The alimentary tract delivers continual water, electrolytes, and nutrients to the body. This necessitates:
- Food movement through the tract.
- Digestive juice secretion and food digestion.
- Water and electrolyte absorption, along with digestive product absorption.
- Blood circulation carrying absorbed substances through gastrointestinal organs.
- Regulation of these functions by local, nervous, and hormonal systems.
Learning Objectives
- Identify different parts of the digestive system and their roles in digestion.
- Detail gastric secretion and HCl formation.
- Describe different phases of digestion.
- Explain digestion of food in the duodenum and small intestine.
- Understand absorption of nutrients, ions, and water from the GI tract.
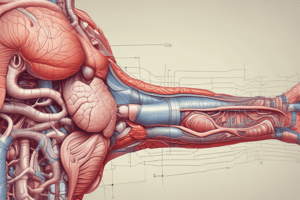
Components of the Digestive System
-
Digestive Tract:
- Oral Cavity (teeth, tongue, soft and hard palates)
- Pharynx
- Esophagus
- Stomach
- Small Intestine
- Large Intestine
-
Accessory Organs:
- Salivary Glands
- Liver
- Gallbladder
- Pancreas
Functions of the Digestive System
- Ingestion
- Mechanical processing
- Digestion
- Secretion
- Absorption
- Excretion
General Principles of Gastrointestinal Motility
- Smooth muscle fibers in the GI tract are organized into bundles.
- Longitudinal muscle bundles extend down the intestinal tract.
- Peristalsis is smooth muscle contraction that moves food toward the rectum.
Digestive System and Digestion
- The digestive system continually supplies the body with water, electrolytes, and nutrients.
- Essential steps include movement of food, digestive juice secretion and digestion of food, absorption of water/electrolytes/digestion products, circulation of blood through organs to remove absorbed substances, and regulation by local, nervous, and hormonal systems.
Neurotransmitters/Neurohormones Secreted by Enteric Neurons
- Acetylcholine, norepinephrine, adenosine triphosphate, serotonin, dopamine, cholecystokinin, substance P, vasoactive intestinal polypeptide, somatostatin, leuenkephalin, metenkephalin, and bombesin are secreted.
- Acetylcholine typically stimulates GI activity.
- Norepinephrine usually inhibits GI activity.
Mechanisms of Stimulation in Alimentary Tract Glands
- Food mechanically stimulating a segment of the GI tract typically triggers gland secretions in that region, and sometimes adjacent regions.
- Local mucosal stimulation also activates the enteric nervous system, responding to tactile stimulation, chemical irritation, and distension of the gut wall.
Daily Secretion of Intestinal Juices
- Provides a table detailing the volume and pH of saliva, gastric secretion, pancreatic secretion, bile, small intestine secretion, Brunner's gland secretion, and large intestinal secretion.
Regulation of Glandular Secretion by Hormones
- Gastrointestinal hormones are secreted from the gastrointestinal mucosa in response to food in the gut lumen.
- These are typically polypeptides or polypeptide derivatives.
Salivary Glands and characteristics of saliva
- There are parotid, submandibular, sublingual glands and small buccal glands.
- Saliva has serous secretions containing ptyalin (a-amylase, a starch digesting enzyme) and mucus secretions containing mucin (acts for lubrication and surface protection).
Esophageal Secretion
- Primarily mucous, this secretion lubricates for swallowing.
- Simple mucous glands line the esophagus.
Gastric Secretion, Phases of Digestion, and Digestion in Duodenum and Small Intestine
- Learning Objectives: To identify gastric secretion and HCl formation stages, stages of digestion, and duodenum/small intestine food digestion.
Gastric Secretions
- Typical oxyntic glands comprise mucous neck cells (secrete mucus), peptic cells (secrete pepsinogen), and parietal cells (secreting HCl and intrinsic factor).
- Secretion of hydrochloric acid is a complex mechanism involving potassium ions, sodium ions, and chloride ions.
- HCl's concentration differs significantly from arterial blood during this process (much more acidic).
Basic Mechanism of Hydrochloric Acid Secretion
- Parietal cells secrete a highly acidic solution (pH about 0.8) containing 160 millimoles of HCl per liter. This process involves active transport.
Secretion and Activation of Pepsinogen
- Pepsinogen is the inactive form of pepsin.
- Hydrochloric acid activates pepsinogen into the active protease pepsin.
- Pepsin activity is optimal in highly acidic environments (pH 1.8-3.5).
Pyloric Glands
- Mostly mucous cells.
- Secrete some pepsinogen and substantial mucus.
- Mucous lubricates food movement and protects the stomach wall from the digestive activity of gastric enzymes.
- Pyloric glands also secrete gastrin (a hormone to control gastric secretion).
Phases of Gastric Secretion
- Cephalic Phase: occurs before food enters, triggered by smell, taste, thought, or chewing of food.
- Gastric Phase: stimulated by ingested food, involving long vagovagal reflexes, local enteric reflexes, and gastrin's action.
Pancreatic Secretion
- Digestive enzymes are secreted by pancreatic acini.
- Sodium bicarbonate and enzymes flow through a pancreatic duct that eventually connects with the hepatic duct.
- Insulin is secreted by pancreatic islets of Langerhans directly into the bloodstream.
Pancreatic Digestive Enzymes
- Trypsin and chymotrypsin break down proteins into peptides.
- Carboxypolypeptidase breaks down peptides to amino acids.
- Pancreatic amylase hydrolyzes starches, glycogen, most carbohydrates (except cellulose) to form mostly disaccharides.
- Pancreatic lipase breaks down neutral fats into fatty acids and monoglycerides.
- Cholesterol esterase hydrolyzes cholesterol esters.
- Phospholipase splits fatty acids from phospholipids.
Digestion in the Small Intestine
- Enterocytes in the mucosa, especially those covering villi, contain digestive enzymes.
- Key enzymes are peptidases for small peptides to amino acids, sucrase, maltase, isomaltase, lactase for splitting disaccharides.
- Intestinal lipase for splitting neutral fats into glycerol and fatty acids.
Digestion of Carbohydrates
- Saliva and pancreatic amylase break down starches and glycogen.
- Maltose and glucose polymers are partly digested.
- Lactase and sucrase digest lactose and sucrose into glucose, galactose, and fructose respectively
Digestion of Proteins
- Pepsin, trypsin, and chymotrypsin break down protein chains into peptides and free amino acids.
- Carboxypeptidase further breaks down proteins into amino acids.
Digestion of Cholesterol Esters and Phospholipids
- Cholesterol ester hydrolase and phospholipase A2 are enzymes that digest cholesterol esters and phospholipids.
Absorption of Water
- Water is absorbed entirely by diffusion through the intestinal membrane.
Absorption of Ions
- Sodium is secreted and absorbed in significant quantities through the intestinal secretions and daily diets.
- Active transport mechanism is crucial for sodium absorption in the small intestine.
- Adequate sodium absorption prevents net loss in the feces.
- Excessive loss of intestinal secretions (e.g., diarrhea) can lead to sodium depletion.
Absorption of Bicarbonate Ions
- Large quantities of bicarbonate ions must be reabsorbed from the small intestine due to high concentrations in pancreatic and bile secretions.
Absorption of Other Ions
- Calcium ions are absorbed primarily in the duodenum via active transport mechanisms mediated by parathyroid hormone and vitamin D activation.
- Iron, potassium, magnesium, phosphate, and other ions are also actively absorbed in the small intestine.
Absorption of Carbohydrates
- Glucose is the most abundant absorbed monosaccharide (80% or more).
- Glucose transport occurs via a sodium co-transport mechanism.
- Galactose and fructose are primarily absorbed via facilitated diffusion.
Absorption of Proteins
- Proteins, after digestion, are absorbed as di- and tri-peptides and amino acids through the intestinal mucosa using a sodium co-transport mechanism.
Absorption of Fats
- Fatty acids, monoglycerides, and other breakdown products of fat digestion are mostly absorbed in the presence of bile micelles.
- Short- and medium-chain fatty acids are absorbed directly into the portal blood, while long-chain fatty acids require conversion into triglycerides. Lymph channels absorb these triglycerides before they enter the bloodstream.
Secretions of the Large Intestine
- Mucus is secreted by goblet cells within the large intestine lining to protect the intestinal wall from bacterial activity and acid in the feces. The alkaline nature of the mucus and sodium-bicarbonate acts as a barrier.
Anatomical Basis of Absorption
- The total amount of fluid absorbed daily equals ingested fluids plus intestinal secretions (about 8-9 liters).
- The small intestine absorbs most of the fluid, allowing only about 1.5 liters to move to the colon daily.
Absorptive Surface of the Small Intestinal Mucosa
- Valvulae conniventes (folds of Kerckring) triple the surface area.
- Villi and microvilli increase surface area 1000-fold, creating 250+ square meters for absorption in the small intestine.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Test your knowledge of the human digestive system with this quiz. From the major subdivisions of the digestive tract to the functions of various glands, this quiz covers essential concepts. Perfect for students studying biology or health sciences.